Amid a nationwide staffing shortage, rising demand for nurses has led hospitals to increase salaries and other benefits to attract and retain workers, Melanie Evans reports for the Wall Street Journal.
Hospitals increase salaries, benefits to keep up with nursing demand
Hospitals across the country have been struggling amid staffing shortages, particularly of nurses, Evans reports. According to health care consultancy Premier, nurse turnover rates have increased to around 22% this year, up from the annual rate of about 18% in 2019.
“We are employing more nurses now than we ever have, and we also have more vacancies than we ever had,” said Greg Till, chief people officer at Providence Health & Services.
To retain their current nurses and attract new staff, many hospitals have increased their nurses’ salaries to remain competitive in the job market, Evans reports.
For example, HCA Healthcare, one of the largest hospital chains in the country, said it increased nurse pay this year to keep up with Covid-19 surges and compete with rivals also trying to fill vacant positions.
Similarly, Jefferson Health in May raised salaries for its nearly 10,000 nurses by 10% after the system discovered that rivals had increased their compensation. “The circumstances required it,” said Kate Fitzpatrick, Jefferson’s chief nurse executive.
In addition, Citizens Memorial Hospital in Bolivar, Mo., this month raised its nurses’ salaries by up to 5% after rivals in other nearby cities increased their workers’ wages. Sarah Hanak, Citizen Memorial’s CNO, said the hospital also increased the hourly wages of nurses working overnight shifts by around 15% to ensure sufficient staffing for those shifts.
“We were forced to,” Hanak said. “We absolutely have to stay competitive.”
Overall, the average annual salary for RNs, not including bonus pay, grew to $81,376, according to Premier—a 4% increase across the first nine months of the year. This is larger than the 3.3% increase in the average annual nurse salary for 2020 and the 2.6% increase in 2019, Evans writes.
In addition to salary increases, some organizations, such as Providence, are also offering other benefits to attract and retain nurses, such as more time off, greater schedule flexibility, and new career development opportunities. Many hospitals are also hiring new graduates to work in specialized roles in ORs and other areas, allowing them to advance their careers more quickly than they would have before.
Overall, this rising demand for nurses has allowed those entering the workforce to negotiate higher salaries, more flexible working hours, and other benefits, Evans writes.
“I think you get to write your ticket,” said Tessa Johnson, president of the North Dakota Nurses Association.
Nurse compensation increases were inevitable—here’s why
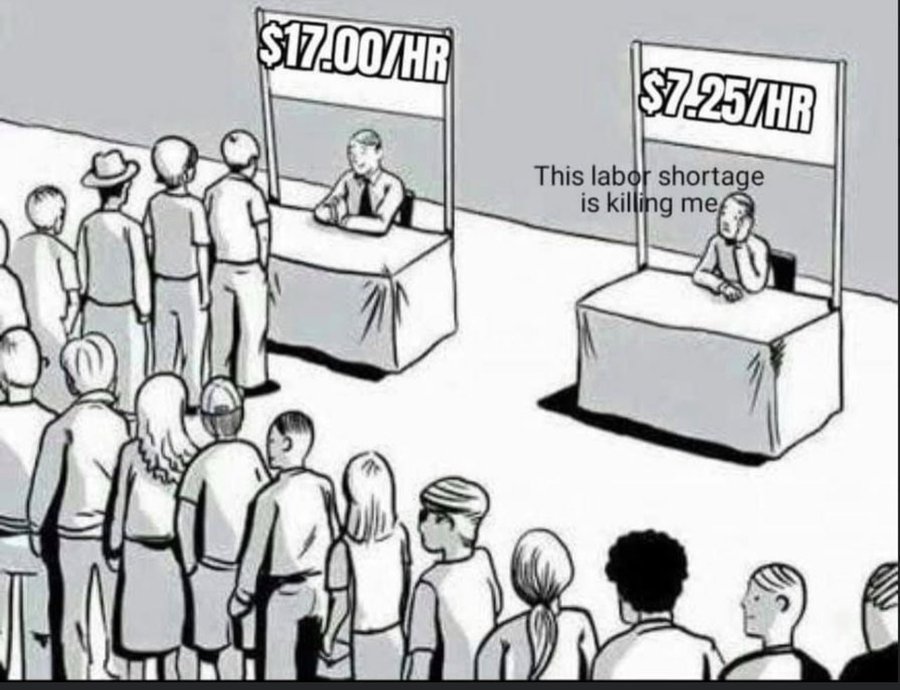
It was inevitable that we would get to this point: baseline nurse compensation on a clear upward trajectory. Inevitable because this boils down to laws of supply and demand. Amid a clear nursing shortage, organizations are being forced to raise baseline compensation to compete for increasingly scarce qualified nurses. This is true in nearly every market, even for those considered to be ‘destination employers.’
If anything, what’s most surprising in the data from Premier is the moderated increase of around 4%. From a worker’s perspective, that’s not even covering cost of living increases due to inflation. However, amid this new data, it’s important to keep two things in mind:
Two considerations for health care leaders
- New data only captures baseline compensation.Differentials—which organizations must standardize and expand across shifts, specialties, and even settings—plus overtime put baseline compensation much higher. Not to mention lucrative sign-on bonuses, that members tell us are increasingly table stakes in their markets. In general, we don’t recommend this type of incentive that does nothing for retention. You’re better off investing those resources in baseline compensation as well as beefing up your RN bonus plan to incentivize retention.
- There is a new floor for wages (and it’s only going up from here).
Open questions (and important indicators) we are assessing
- What happens to wages for entry-level clinical roles? As the shortage of RNs persists, organizations will need to make a shift to team-based models of care, and those are only possible with a stable workforce of entry-level personnel. Right now, that part of the health care workforce is anything but stable. When you consider their work and their wages in comparison to out-of-industry players that pay the same or better, that’s a clear area where investment is required.
- Will the share of nurses working permanently with travel agencies return to pre-pandemic levels? That’s to say, what will those RNs who experienced the traveler lifestyle and pay value more moving forward: the flexibility and premium pay or stability of permanent employment? Even if this number stabilizes a couple percentage points above pre-pandemic levels, that will aggravate provider’s sense of shortage.