
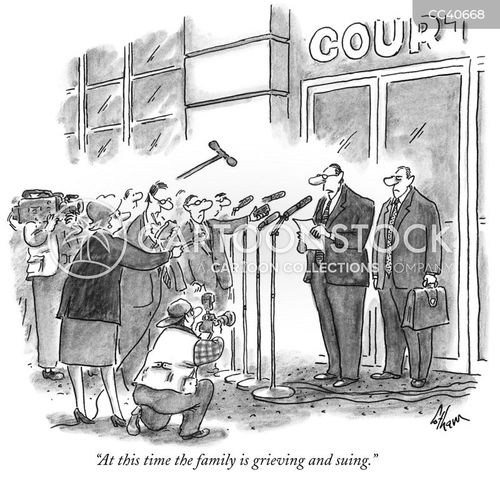
Cartoon – Sign of the Times



Horizon Blue Cross Blue Shield of New Jersey threatened to stop paying medical claims for about 14,000 employees of the Jersey City Board of Education, a lawsuit filed by the board alleges, according to NJ.com.
Horizon Healthcare Services, the district’s medical claim manager, planned to stop processing insurance claims Nov. 25 amid an ongoing dispute over payment, the lawsuit alleges. On Nov. 24, a judge granted a temporary restraint aimed at protecting the insured until Dec. 17.
The school board accused Horizon of not complying with lowering out-of-network rates and charging hidden fees, among other allegations, according to the lawsuit.
Horizon denied the allegations. In a statement to NJ.com, Thomas Vincz, public relations manager for Horizon Blue Cross Blue Shield of New Jersey, said: “At no time did Horizon ever threaten to terminate the [Board of Education]’s coverage and Jersey City Board of Education employees should know that their coverage has remained in place, uninterrupted, while we continue to work with Board staff to resolve the issues preventing them from paying the charges owed under their existing contract.”
The lawsuit was filed in the Hudson County Superior Court. Horizon has until Dec. 9 to respond to the lawsuit, according to NJ.com.

Purdue Pharma, the maker of OxyContin, pleaded guilty Tuesday to three federal criminal charges related to the company’s role in creating the nation’s opioid crisis. Purdue Pharma board chairman Steve Miller pleaded guilty on behalf of the company during a virtual federal court hearing in front of US District Judge Madeline Cox Arleo.
The counts include one of dual-object conspiracy to defraud the United States and to violate the Food, Drug, and Cosmetic Act, and two counts of conspiracy to violate the Federal Anti-Kickback Statute.
The plea deal announced in October includes the largest penalties ever levied against a pharmaceutical manufacturer, including a criminal fine of $3.544 billion and an additional $2 billion in criminal forfeiture, according to a Department of Justice press release.
The company, which declared bankruptcy last year, will be dissolved as a part of the plea agreement, and its assets will be used to create a new “public benefit company” controlled by a trust or similar entity designed for the benefit of the American public.
The Justice Department has said Purdue Pharma will function entirely in the public interest rather than to maximize profits. Its future earnings will go to paying the fines and penalties, which in turn will be used to combat the opioid crisis.
In pleading guilty to the criminal charges, the company is taking responsibility for past misconduct, Purdue Pharma said in a statement to CNN Tuesday.”Having our plea accepted in federal court, and taking responsibility for past misconduct, is an essential step to preserve billions of dollars of value for creditors and advance our goal of providing financial resources and lifesaving medicines to address the opioid crisis,” the statement said. “We continue to work tirelessly to build additional support for a proposed bankruptcy settlement, which would direct the overwhelming majority of the settlement funds to state, local and tribal governments for the purpose of abating the opioid crisis.”
According to the US Centers for Disease Control and Prevention, about 70,000 Americans died of drug overdoses in 2018, just one year of the opioid crisis, and about 70% of those deaths were caused by prescription or illicit opioids like OxyContin. In that year, an estimated 10.3 million Americans 12 and older misused opioids, including 9.9 million prescription pain reliever abusers and 808,000 heroin users, according to the US Department of Health and Human Services Substance Abuse and Mental Health Services Administration.
The Sackler family, and other current and former employees and owners of the company, still face the possibility that federal criminal charges will be filed against them. The court did not set a date for a sentencing hearing.

A federal appeals court upheld a ruling that would allow hospitals to calculate their disproportionate share hospital (DSH) payments using Medicaid patients as well as patients eligible for treatment under experimental Medicaid “demonstration projects” approved by the Department of Health and Human Services (HHS).
The opinion, issued Friday, upheld the decision of a lower court that sided with 10 Florida hospitals seeking to include days of care funded by Florida’s Low Income Pool, an approved Medicaid demonstration project. Through the pool, the state and federal governments jointly reimbursed hospitals for care provided to uninsured and underinsured patients.
HHS argued against allowing the hospitals to include those patients in their Medicaid fraction on the ground that the patients were treated out of charity rather than as designated beneficiaries of a demonstration project.
“The district court found the Secretary’s arguments to the contrary unpersuasive. The Secretary argued the text of the regulation allows hospitals to include days of care provided under a demonstration project only if the project entitles specific patients to specific benefit packages,” the judges said (PDF). “As the court noted, however, this is not what the regulation says. Rather, a patient must have been ‘eligible for inpatient services,’ meaning the demonstration project enabled the patient to receive inpatient services, regardless whether the project gave the patient a right to these services or allowed the patient to enroll in an insurance plan that provided the services.”
DSH payments have traditionally been calculated using the costs incurred to treat Medicaid and uninsured patients. However, the Centers for Medicare & Medicaid’s 2017 rule says costs incurred treating other patients are applicable. For example, a dually eligible patient who’s admitted to the hospital will likely have their stay paid for by Medicare, the agency said, as Medicaid is treated as the “payer of last resort.” As such, those costs would be eligible to be subtracted from DSH payouts.
In backing the hospitals on the DSH dispute, the judges pointed to a similar case considered by the Fifth Circuit last year in which the agency sought to exclude from the Medicaid fraction days of care funded through an “uncompensated care pool” created by a demonstration project. That pool reimbursed hospitals in Mississippi for services provided to uninsured patients affected by Hurricane Katrina but did not entitle specific patients to specific services.
In that case, the Fifth Circuit held “plain regulatory text demands that such days be included—period.”
“We see no flaw in Judge Collyer’s analysis and therefore embrace the district court’s opinion as the law of this circuit,” the judges said.

Even a solidly conservative Supreme Court could find a pretty easy path to preserve most of the Affordable Care Act — if it wants to.
The big picture: It’s too early to make any predictions about what the court will do, and no ACA lawsuit is ever entirely about the law. They have all been colored by the bitter political battles surrounding the ACA.
How it works: There are two steps to the current ACA case. First, the justices will have to decide whether the law’s individual mandate has become unconstitutional. If it has, they’ll then have to decide how many other provisions have to fall along with it.
“If you picture severability being like a Jenga game — it’s kind of, if you pull one out, can you pull it out while it all stands? Or if you pull two out, will it still stand?” Barrett explained during Wednesday’s questioning.
Severability is a question of congressional intent — whether Congress still would have passed the rest of a law if it knew it couldn’t have the piece the courts are striking down. And conservative judges make a point of relying only on a law’s text when determining congressional intent.
The other side: The red states challenging the law, on the other hand, get further away from straight textualism.
What we’re watching: Barrett acknowledged in this week’s hearings that the law has changed since it was first passed — a potentially encouraging sign, if you’re an ACA defender hoping the conservative justices will look at legislative text Congress wrote in 2017 instead of expert statements from 2010.
A case from earlier this year — tied to another big-ticket Obama policy — might also help illuminate the current court’s approach to severability.
Yes, but: None of this means that the threat to the entire ACA, or to its protections for people with pre-existing conditions, has been exaggerated.
The bottom line: The ACA’s allies may not be able to save the remains of the individual mandate, but that’s a loss they can live with. And there is at least a clear path to a ruling, even from a conservative court, that would leave the rest of the law intact.

The U.S. Supreme Court is set to hear a case questioning the legality of the ACA on Nov. 10.
Five things to know:
1. At the center of the case is whether the health law should be struck down. In a brief filed June 25 in Texas v. United States, the Trump administration argues the entire ACA is invalid because in December 2017, Congress eliminated the ACA’s tax penalty for failing to purchase health insurance. The administration argues the individual mandate is inseverable from the rest of the law and became unconstitutional when the tax penalty was eliminated; therefore, the entire health law should be struck down.
2. The administration’s brief was filed in support of a group of Republican-led states seeking to undo the ACA. Meanwhile, California Attorney General Xavier Becerra is leading a coalition of more Democratic states to defend the ACA before the Supreme Court.
3. The case goes before the Supreme Court days after media outlets projected Joe Biden as the next president of the U.S. President-elect Biden has said he seeks to expand government-subsidized insurance coverage and wants to the bring back the ACA’s tax penalty for failing to purchase health insurance, according to The Wall Street Journal. If a change regarding the tax penalty did occur, the publication notes that Republicans’ argument on severability would no longer apply.
4. The case also goes before the Supreme Court about two weeks after the Senate voted Oct. 26 to confirm Amy Coney Barrett to the Supreme Court. Ms. Barrett previously criticized Chief Justice John Roberts’ 2012 opinion sustaining the law’s individual mandate, The New York Times reported, but she said during her confirmation hearings in October that “the issue in the case is this doctrine of severability, and that’s not something that I have ever talked about with respect to the Affordable Care Act.”
5. According to the Journal, the Supreme Court is not expected to make a decision in the case until the end of June.
https://mailchi.mp/f2794551febb/the-weekly-gist-october-23-2020?e=d1e747d2d8
This week Nebraska became the latest state to receive waiver authority from the Trump administration to implement work requirements as part of its Medicaid expansion program.
The program, called “Heritage Health Adult”, will be a two-tiered system, with expansion-eligible adults choosing between “Basic” and “Prime” coverage levels. The lower tier will provide coverage for physical and behavioral health services, with a prescription drug benefit, and is open to adults not eligible for traditional Medicaid with incomes under 138 percent of the federal poverty line.
“Prime” enrollees will get additional dental, vision, and over-the-counter drug benefits, in exchange for agreeing to 80 hours per month of work, volunteering, or active job seeking, which must be reported to the state.
Nebraska voters approved the Medicaid expansion two years ago, although enrollment only began this August, and the work-linked demonstration project is slated to start next year. An estimated 90,000 additional Nebraskans are expected to enroll in Medicaid under the expanded program.
The approval of Nebraska’s Medicaid work requirement comes a week after the Trump administration approved a partial expansion of Medicaid in Georgia, called “Pathways to Coverage”, which is also tied to a requirement to seek or engage in employment or education activities.
The Georgia program also requires premium payments by eligible adults who make between 50 and 100 percent of the federal poverty line. Court challenges will inevitably ensue for both the Nebraska and Georgia programs—only Utah has successfully implemented Medicaid work requirements, with 16 other state programs either pending approval, held up in court, or awaiting implementation. We continue to be deeply skeptical of Medicaid work requirements, and believe they only serve to deter those who would otherwise qualify for coverage from enrolling, and that the expense of their implementation and ongoing operation often outweighs any savings to the state.
The argument that “work encourages health”, often advanced by proponents of work requirements, gets it exactly backwards—rather, health security encourages work, a reality that has become ever more urgent as the COVID pandemic has drawn on.
As the economy continues to falter, Medicaid’s importance as a safety net program grows ever greater, and work requirements create an unhelpful obstacle to basic healthcare access.

https://www.pionline.com/courts/blue-cross-blue-shield-sues-allianzgi-over-investment-strategies

Blue Cross Blue Shield’s national employee benefits committee filed a lawsuit against Allianz Global Investors and its investment consultant Aon Investments USA, charging both with breaches of fiduciary responsibilities and breach of contract regarding more than $2 billion in losses in the insurer’s defined benefit plan trust.
The lawsuit, filed Wednesday in U.S. District Court in New York, alleges that AllianzGI took “reckless actions” in the management of three funds the manager had said offered downside protection against market declines and volatility, according to the court filing.
As of Jan. 31, the National Retirement Trust of the Blue Cross and Blue Shield Association had a total of $2.9 billion invested in the AllianzGI Structured Alpha Multi-Beta Series LLC I, AllianzGI Structured Alpha Emerging Markets Equity 350 LLC, and the AllianzGI Structured Alpha 1000 LLC, according to the filing.
After the funds experienced heavy losses in February and March, the investments were liquidated and redeemed, and the committee received about $540 million, according to the filing.
As of Dec. 31, 2018, the Blue Cross and Blue Shield Association National Retirement Trust had $4.6 billion in assets, according to its most recent Form 5500 filing.
The lawsuit, which includes claims breach of fiduciary duty and breach of contract against both AllianzGI and Aon, alleges that AllianzGI “caused the (benefits) committee to believe that structured alpha’s risk profile was consistent with Allianz’s stated investment strategy rather than the actual risk profile, either by making false or misleading representations about structured alpha or failing to disclose information necessary to correct prior representations that were inconsistent with how Allianz was actually managing the strategy.”
The suit alleges Aon breached its obligations by “failing to monitor and inform the committee of breakdowns in Allianz’s risk management protocols, learning only after the catastrophic events of March 2020 that Allianz had inadequate risk management in place.”
AllianzGI’s structured alpha strategies have historically been designed to be both long and short volatility, according to a September 2016 presentation: Taking range-bound spread positions, to sell options that were most likely to expire worthless (short volatility); hedged positions designed to protect against market crashes (long volatility); and directional spread positions designed to generate returns when equity indexes rise or fall more than usual during multiweek periods (long/short volatility).
The lawsuit alleges that “when equity markets declined, volatility spiked and the funds’ option positions were exposed to a heightened risk of loss in February and March 2020, those promised protections were absent.”
The lawsuit seeks relief including restoration of all losses, actual damages and accounting and disgorgement of fees and profits.
John Wallace, AllianzGI spokesman, said in an email: “While the losses sustained by the Structured Alpha portfolio during the market downturn in late February and March were disappointing, AllianzGI believes the allegations made by Blue Cross Blue Shield are legally and factually flawed. We will defend ourselves vigorously against these claims. Blue Cross Blue Shield was advised by a sophisticated investment consultant to evaluate the Structured Alpha strategy. These funds sought to deliver substantial returns of as much as 10% above, net of fees, the returns of the fund’s benchmark, an index like the S&P 500. As was fully disclosed to Blue Cross Blue Shield, the Structured Alpha strategy involved risks commensurate with those higher returns. Blue Cross Blue Shield and their consultant determined that the Structured Alpha Portfolio fit with their overall investment goals and risk tolerances.”
The $15.3 billion Arkansas Teacher Retirement System, Little Rock, filed its own lawsuit against Allianz Global Investors and subsidiaries in July, regarding its own losses in structured alpha strategies.
Robert Elfinger, Aon spokesman, said the company does not comment on pending litigation.
Sean W. Gallagher, Adam L. Hoeflich, Nicolas L. Martinez, Abby M. Mollen and Mark S. Ouweleen, partners at Bartlit Beck, attorney for the plaintiffs, could also not be immediately reached for comment.