At the Annual Meeting of the American Hospital Association in DC last week, its all-out attack on “corporate insurance” was a prominent theme. In the meeting recap, AHA CEO Rick Pollack made the influential organization’s case:
“This year, there was special focus on educating policymakers that our health care system is suffering from multiple chronic conditions. These include continued government underpayment, cyberattacks, workforce shortages, broken supply chains, access to behavioral health, and irresponsible behavior by corporate commercial health insurance companies, among others — that put access to services in serious jeopardy.”
The AHA’s declaration of war came on the heels of last week’s Congressional investigation of Change Healthcare’ (UnitedHealth Group subsidiary) cybersecurity breech and the widely-noticed earnings release by Elevance (aka Anthem) that featured prominently its plans to build a $4 billion business unit focused on primary care and chronic care management. Per company CEO Gail Boudreaux:
“This will help us continue through having a focus on advanced primary care; it’s still very much focused on our chronic patients and complex patients. We are still building specialty care enablement, which is another very important component of what we’re trying to prime through… In time, Elevance Health will have full ownership of what we expect will be a leading platform for value-based care delivery and physician enablement at scale.”
To industry watchers, the war is no surprise.
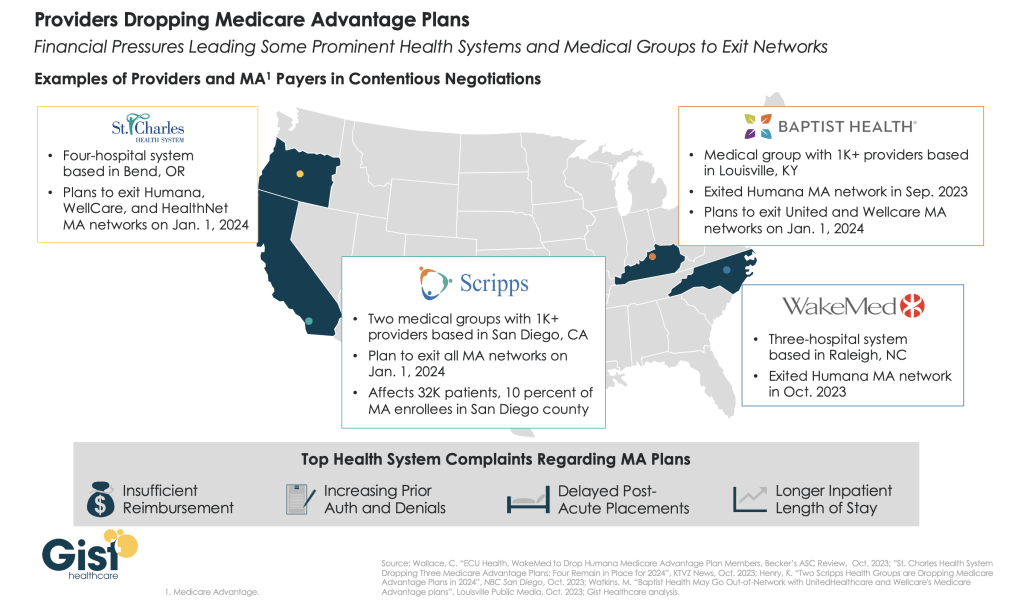
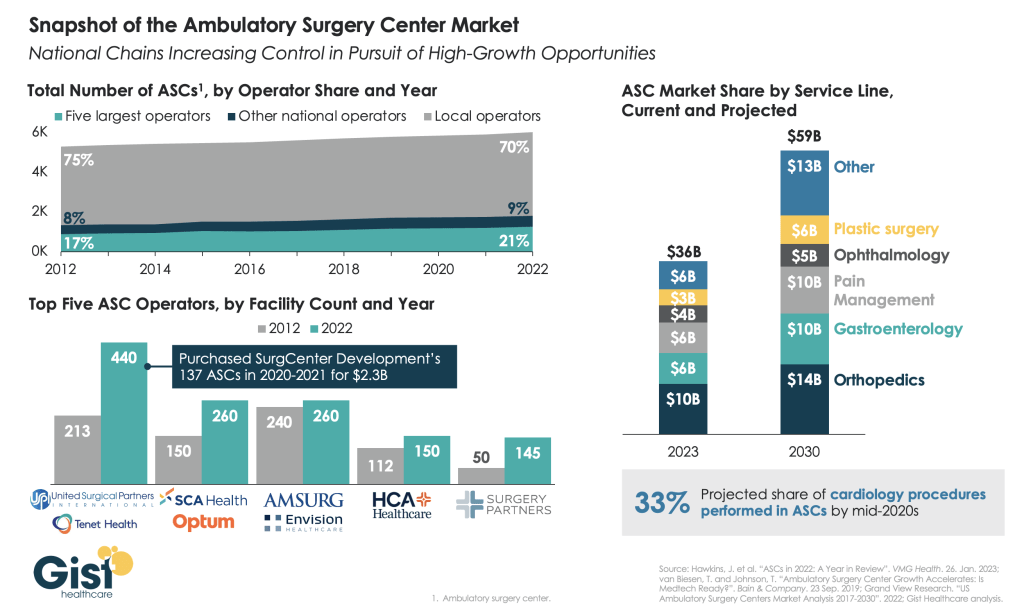
It’s been simmering for years but most recently inflamed as operating margins for most hospitals eroded while profits among corporate insurers led by Big 6 (UnitedHealth, Humana, CVS-Aetna, Elevance, Cigna, Centene) swelled at double-digit rates.
To outsiders, it’s not quite so clear.
Big names (Brands) are prominent in both. Corporatization seems embedded in the business models for both. And both appear complicit in well-documented beliefs that the health system is failing as unnecessary higher costs make it less accessible, affordable and effective.
As the War intensifies, each combatant is inclined to make their cases aggressively contrasting “us” against “them.” Here’s where things stand today:
| Consideration | Hospitals | Corporate Insurers | Advantage |
| Public Standing | Hospitals enjoy relatively strong public support but growing discontent about their costs, prices and household affordability. Hospitals blame insurers & drug companies for increasing health costs.Increased attention to affordability, value and low prices is a threat. | Insurers enjoy reasonably high support among middle & high-income consumers who think it necessary to their financial security. Insurers blame drug companies, hospitals and unhealthy consumer behaviors for increased health costs. | It’s a tossup. Though polls show trust in hospitals is higher than insurers, both are declining especially among younger, urban and low-middle income consumers |
| Regulatory positioning | Scrutiny of business practices & the impact of consolidation on consumer prices, workforce wage compression, competition et al is significant and increasing in 5 Congressional Committees and 3 Federal agencies. Hospitals also face state and local regulatory challenges around pricing, community benefits, et al. | Compliance with plan transparency rules, prior authorization requirements, Medicare Advantage marketing & coverage, and antitrust are targets. Levels of Congressional attention to business practices are relatively low. Insurers are primarily overseen by states, so the regulatory landscape varies widely except. | Insurers enjoy regulatory advantages today not withstanding current attention to UnitedHealth Group. Hospitals are “soft targets” for state legislatures, Congress and investigators in state and federal agencies. |
| Confidence of capital markets in their core businesses: Hospitals: inpatient, outpatient careInsurers: group & individual coverage, claims data commercialization | The acute sector, especially rural & systems operating in low-growth markets, face insurmountable headwinds due to reimbursement cuts, value-based purchasing initiatives by Medicare and private insurers and clinical innovations that drive demand away from inpatient care. Hospital Outpatient services are profitable for the near term despite growing competition from privately investors. | The consolidation of power, financial strength & influence among the corporate insurers is assuring to lenders & investors who value their performance and support their vertical integration expansion role. | Lenders and investors favor “corporate insurers” over others. The potential (likelihood) that hospitals will lose on high profile revenue-enhancer issues (facility fees, site neutral payments, et al) and restrict tax exemptions for NFP hospital operators is concerning to the capital markets. |
| Relationships with Physicians | Hospitals employ 58% of physicians directly & relate to all. Regulations (i.e. Stark Laws, et al), capital deployment for hospital programs and administrative overhead are factors of high importance to physicians seeking clinical autonomy & financial security. Hospitals are a viable option to physicians seeking income security though not without concern. | Insurers employment of physicians plus contractual relationships with network physicians are transactional. Physicians inclined toward business relationships with “corporate insurers” believe their role in healthcare’s future is more stable than that of hospitals based on the belief hospitals are wasteful and non-responsive to physician input. | Hospitals enjoy a relationship advantage with most physicians. Corporate insurers enjoy a transactional relationship with physicians that’s premised on shared views about the future of the system vs. hospitals that focus on protecting the past. Hospitals enjoy a near-term advantage but the long-term is uncertain. |
| Unity of voice | Relatively strong around “chronic ailments” of the system but unclear about long-term destination and limited to universal hospital concerns (i.e. 340B) vs. cohort issues (tax exemptions for not for profits). The delineations between not-for-profit, investor-owned and public/government restricts the strength of hospital voice overall as each seeks unique recognition and regulatory protections. | Corporate insurers have corporate boards, broader membership, stronger balance sheets and scale. Their messaging is customized to their key customers and influencers and aligned with but not controlled by their trade groups. And they direct considerable resources to their proprietary messaging strategies. | Corporate insurers have fewer constraints in their messaging and enjoy an advantage in opining to issues that resonate with consumers (prices, quality, value). |
| Long-term Vision for the U.S. Health System | A private connected system of health in which hospitals coordinate and provide services for patients across the continuum of their care: preventive, chronic, acute and long-term. | A private system of comprehensive, customized products and services that operates efficiently, effectively and in the interests of all consumers. | The public and Congress aren’t sure which is better positioned to develop a “new” system of health. |
This war has been simmering. It’s now a blaze. The outcome is uncertain despite the considerable resources both will spend to win.
Stay tuned.
Paul
P.S. Last week, I participated in Scottsdale Institute’s Annual Leadership Summit in Arizona. It’s 62 institutional members and corporate partners include most of the major not-for-profit health systems and the biggest names in healthcare information technology solutions.
I left with two strong impressions I’ll share:
1-How GenAI and HCIT influence the future of healthcare services delivery is very much speculative but no-less certain. It’s a work in process for everyone.
2- To navigate its evolution, knowledge sharing (and mistake sharing) among those in the trenches is essential. SI afforded a great venue for both, and also a platform for those of us who are easily overwhelmed by all this to ask honest questions and get candid answers.
Check it out. http://www.scottsdaleinstitute.org.