Category Archives: Operating Expenses
National Hospital Flash Report: October 2023
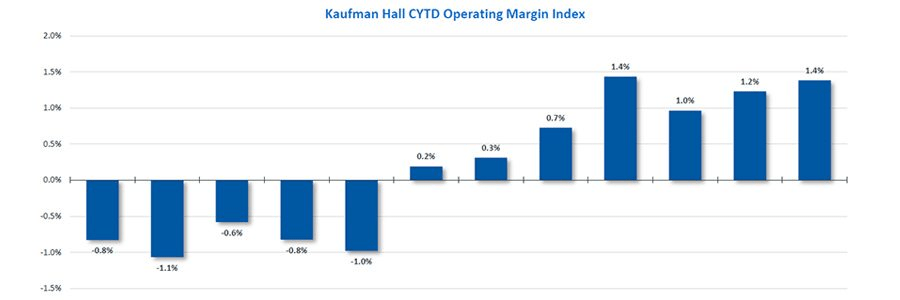
While hospitals’ overall performance declined slightly in September compared to the previous month, the median Kaufman Hall Calendar Year-To-Date Operating Margin Index reflecting actual margins was 1.4% in September. This slight increase was due to the historical variation in the performance of hospitals across 2023.
Volume decreased across the board, but data indicate improvement in the overall financial picture compared to 2022.
The October issue of the National Hospital Flash Report covers these and other key performance metrics.
California passes law raising healthcare worker hourly minimum wage to $25
https://mailchi.mp/59f0ab20e40d/the-weekly-gist-october-27-2023?e=d1e747d2d8

Earlier this month, Governor Gavin Newsom signed a bill that puts all full- and part-time California healthcare workers, including all ancillary support staff, on a path to earning $25 per hour.
While wage increases will begin phasing in next year, the timeline for implementation depends on facility type and other factors like payer mix. Large health systems and dialysis centers have until 2026 to fully implement the new wage, while rural, independent hospitals and those with high public payer mixes, as well as other clinical facilities, have more time to comply.
The law, which replaces the $15.50 state minimum wage for all workers, is projected to impact over 469K healthcare workers in the state, potentially including 50K who already earn more than $25 per hour but are forecasted to receive wage increases to maintain their pay premiums. Strongly backed by California healthcare unions, the law ultimately received the support of the California Hospital Association on the grounds that it will “create stability and predictability for hospitals” by preempting local wage and compensation measures active in many California cities.
The Gist: On the heels of a tentatively successful labor negotiation with Kaiser Permanente—which would raise the system’s hourly minimum wage to $25—California healthcare unions have flexed their might for another win.
While this new law directly benefits healthcare workers earning less than $25 an hour, its knock-on effects will extend to those earning above that to avoid pay compression, as well as to workers in other industries that draw from the same labor pool.
The mandated higher pay may provide California healthcare employers with a recruitment edge (and lure talent away from neighboring states), but higher costs will exacerbate the margin challenges plaguing many hospitals in the state.
Uneven operating margin recovery for national health systems
https://mailchi.mp/de5aeb581214/the-weekly-gist-october-13-2023?e=d1e747d2d8

Using data from Kaufman Hall’s latest National Hospital Flash Report and publicly available investor reports for some of the nation’s largest health systems, the graphic below takes stock of the state of health system margins.
After the median hospital delivered negative operating margins for twelve-straight months, 2023 has made for a positive but slim year so far, with margins hovering around one percent. Amid this breakeven environment, fortunes have diverged between nonprofit and for-profit health systems.
The largest for-profit systems, HCA Healthcare and Tenet Healthcare, posted operating margins of around 10 percent between July 2022 and June 2023, while the three largest nonprofit systems, Kaiser Permanente, CommonSpirit Health, and Ascension, suffered net losses.
Although Kaiser Permanente’s margin bounced back in the first half of this year, CommonSpirit and Ascension’s margins continued to decline, more than doubling the operating losses of the prior six months.
One key to the recent success of the largest for-profit systems is their diversification away from inpatient care.
Case in point: almost half of Tenet’s profits in 2023 have come from its ambulatory division, driven by its United Surgical Partners International (USPI) ambulatory surgery center network, which has posted 40 percent margins over the past several quarters.
2023 State of Healthcare Performance Improvement Report: Signs of Stabilization Emerge

Executive Summary
Hospitals and health systems are seeing some signs of stabilization in 2023 following an extremely difficult year in 2022. Workforce-related challenges persist, however, keeping costs high and contributing to issues with patient access to care. The percentage of respondents who report that they have run at less than full capacity at some time over the past year because of staffing shortages, for example, remains at 66%, unchanged from last year’s State of Healthcare Performance Improvement report. A solid majority of respondents (63%) are struggling to meet demand within their physician enterprise, with patient concerns or complaints about access to physician clinics increasing at approximately one-third (32%) of respondent organizations.
Most organizations are pursuing multiple strategies to recruit and retain staff. They recognize, however, that this is an issue that will take years to resolve—especially with respect to nursing staff—as an older generation of talent moves toward retirement and current educational pipelines fail to generate an adequate flow of new talent. One bright spot is utilization of contract labor, which is decreasing at almost two-thirds (60%) of respondent organizations.
Many of the organizations we interviewed have recovered from a year of negative or breakeven operating margins. But most foresee a slow climb back to the 3% to 4% operating margins that help ensure long-term sustainability, with adequate resources to make needed investments for the future. Difficulties with financial performance are reflected in the relatively high percentage of respondents (24%) who report that their organization has faced challenges with respect to debt covenants over the past year, and the even higher percentage (34%) who foresee challenges over the coming year. Interviews confirmed that some of these challenges were “near misses,” not an actual breach of covenants, but hitting key metrics such as days cash on hand and debt service coverage ratios remains a concern.
As in last year’s survey, an increased rate of claims denials has had the most significant impact on revenue cycle over the past year. Interviewees confirm that this is an issue across health plans, but it seems particularly acute in markets with a higher penetration of Medicare Advantage plans. A significant percentage of respondents also report a lower percentage of commercially insured patients (52%), an increase in bad debt and uncompensated care (50%), and a higher percentage of Medicaid patients (47%).
Supply chain issues are concentrated largely in distribution delays and raw product and sourcing availability. These issues are sometimes connected when difficulties sourcing raw materials result in distribution delays. The most common measures organizations are taking to mitigate these issues are defining approved vendor product substitutes (82%) and increasing inventory levels (57%). Also, as care delivery continues to migrate to outpatient settings, organizations are working to standardize supplies across their non-acute settings and align acute and non-acute ordering to the extent possible to secure volume discounts.
Survey Highlights
| 98% of respondents are pursuing one or more recruitment and retention strategies |
| 90% have raised starting salaries or the minimum wage |
| 73% report an increased rate of claims denials |
| 71% are encountering distribution delays in their supply chain |
| 70% are boarding patients in the emergency department or post-anesthesia care unit because of a lack of staffing or bed capacity |
| 66% report that staffing shortages have required their organization to run at less than full capacity at some time over the past year |
| 63% are struggling to meet demand for patient access to their physician enterprise |
| 60% see decreasing utilization of contract labor at their organization |
| 44% report that inpatient volumes remain below pre-pandemic levels |
| 32% say that patients concerns or complaints about access to their physician enterprise are increasing |
| 24% have encountered debt covenant challenges during the past 12 months |
| None of our respondents believe that their organization has fully optimized its use of the automation technologies in which it has already invested |
Health “insurtechs” struggling to stay relevant
https://mailchi.mp/9fd97f114e7a/the-weekly-gist-october-6-2023?e=d1e747d2d8
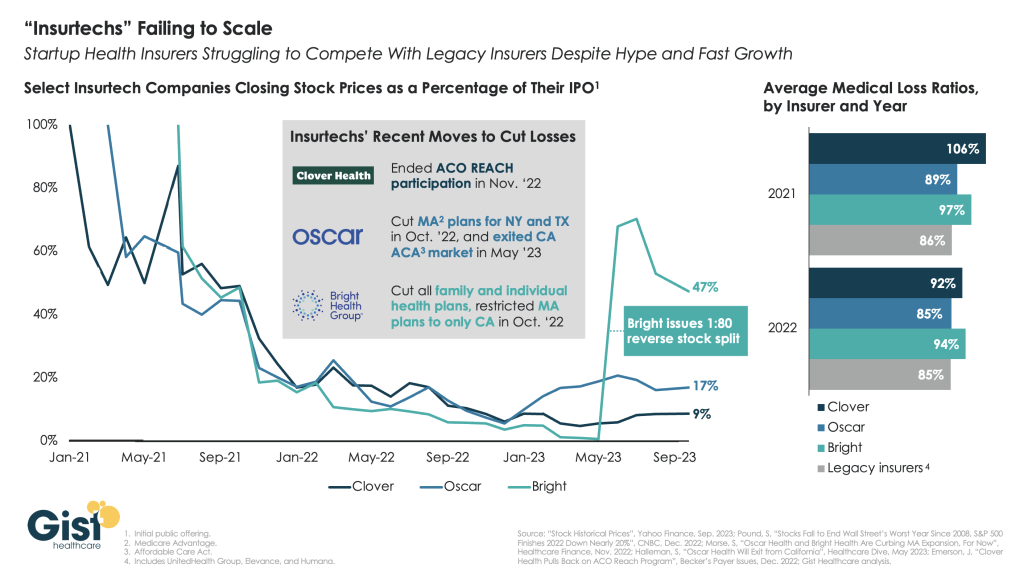
“Insurtechs” Clover Health, Oscar Health, and Bright Health all went public in the midst of the hot equity market of 2021. Investors were excited by the fast growth of these health insurer startups, and their potential to revolutionize an industry dominated by a few large players.
However, the hype has dissipated as financial performance has deteriorated. After growing at all costs during a period of low interest rates, changing market conditions directed investors to demand a pivot to profitability, which the companies have struggled to deliver—two years later, none of the three has turned a profit.
Oscar and Bright have cut back their market presence significantly, while Clover has mostly carried on while sustaining high losses. In the last two years, only Oscar has posted a medical loss ratio in line with other major payers, who meanwhile are reporting expectation-beating profits. While Oscar has shown signs of righting the ship since the appointment of former Aetna CEO Mark Bertolini,
the future of these small insurers remains uncertain. As their losses mount and they exit markets, they may become less desirable as acquisition targets for large payers.
Kaiser Permanente healthcare workers initiate record strike
https://mailchi.mp/9fd97f114e7a/the-weekly-gist-october-6-2023?e=d1e747d2d8

On Wednesday, 75K Kaiser Permanente (KP) healthcare workers in five states and Washington, DC walked off the job as part of the largest healthcare strike in US history.
The striking workers are a diverse group, based mostly in California, that includes support staff, X-ray technicians, medical assistants, and pharmacy workers. They will continue their work stoppage until Saturday morning, though union leadership is threatening an even larger strike in November if a new contract agreement is not reached by then.
Their employment contract expired on September 30th, and while negotiations have progressed on issues like shift-payment differentials and employee training investments, union leaders and KP executives remain at odds over key wage increase demands, with the unions asking for a $25 national minimum wage, and KP proposing $21.
The company has sought to minimize disruptions to patient care during the strike, bringing in temporary labor to keep critical infrastructure open, but has told its members to expect some non-urgent procedures to be rescheduled, some clinic and pharmacy operating hours to be reduced, and call center wait times to be lengthy.
The Gist: Kaiser Permanente has enjoyed solid relations with its unions for decades, making this strike a significant break from precedent, fueled by post-pandemic burnout and staffing shortages.
While KP is keeping all essential services open, care disruptions are inevitable with around one third of its total workforce on strike.
The stakes of these labor negotiations extend far beyond just KP and its employees, as union success could inspire other unionized healthcare workers to adopt similar tactics and demands. (Case in point: Employees at eleven Tenet Healthcare facilities in California represented by SEIU-UHW, one of the unions representing striking KP workers, just voted to authorize their own strike.)
While happening alongside high-profile strikes in other industries, labor unrest is a troubling trend for health systems, whose margins remain well below historical levels amid persistently high labor and supply expenses.
Thousands of US health care workers go on strike in multiple states over wages and staff shortages
https://apnews.com/article/kaiser-health-care-workers-strike-b8b40ce8c082c0b8c4f1c0fb7ec38741

Picketing began Wednesday at Kaiser Permanente hospitals as some 75,000 health care workers went on strike in Virginia, California and three other states over wages and staffing shortages, marking the latest major labor unrest in the United States.
Kaiser Permanente is one of the country’s larger insurers and health care system operators, with 39 hospitals nationwide. The nonprofit company, based in Oakland, California, provides health coverage for nearly 13 million people, sending customers to clinics and hospitals it runs or contracts with to provide care.
The Coalition of Kaiser Permanente Unions, representing about 85,000 of the health system’s employees nationally, approved a strike for three days in California, Colorado, Oregon and Washington, and for one day in Virginia and Washington, D.C.
A cheer went up from union members outside Kaiser Permanente Los Angeles Medical Center when the strike deadline arrived before dawn.
The strikers include licensed vocational nurses, home health aides and ultrasound sonographers, as well as technicians in radiology, X-ray, surgical, pharmacy and emergency departments.
Doctors are not participating, and Kaiser says its hospitals, including emergency rooms, will remain open during the picketing. The company said it was bringing in thousands of temporary workers to fill gaps during the strike. But the strike could lead to delays in getting appointments and non-urgent procedures being rescheduled.
It comes amid unprecedented worker organizing — from strike authorizations to work stoppages — within multiple industries this year, including, transportation, entertainment and hospitality.
Wednesday’s strike is the latest one for the health care industry this year as it continues to confront burnout with the heavy workloads — problems that were exacerbated greatly by the pandemic.
Unions representing Kaiser workers in August asked for a $25 hourly minimum wage, as well as increases of 7% each year in the first two years and 6.25% each year in the two years afterward.
They say understaffing is boosting the hospital system’s profits but hurting patients, and executives have been bargaining in bad faith during negotiations.
“They’re not listening to the frontline health care workers,” said Mikki Fletchall, a licensed vocational nurse based in a Kaiser medical office in Camarillo, California. “We’re striking because of our patients. We don’t want to have to do it, but we will do it.”
Kaiser has proposed minimum hourly wages of between $21 and $23 next year depending on the location.
Since 2022, the hospital system has hired 51,000 workers and has plans to add 10,000 more people by the end of the month.
Kaiser Permanente reported $2.1 billion in net income for this year’s second quarter on more than $25 billion in operating revenue. But the company said it still was dealing with cost headwinds and challenges from inflation and labor shortages.
Kaiser executive Michelle Gaskill-Hames defended the company and said its practices, compensation and retention are better than its competitors, even as the entire sector faces the same challenges.
“Our focus, for the dollars that we bring in, are to keep them invested in value-based care,” said Gaskill-Hames, president of Kaiser Foundation Health Plan and Hospitals of Southern California and Hawaii.
She added that Kaiser only faces 7% turnover compared to the industry standard of 21%, despite the effects of the pandemic.
“I think coming out of the pandemic, health care workers have been completely burned out,” she said. “The trauma that was felt caring for so many COVID patients, and patients that died, was just difficult.”
The workers’ last contract was negotiated in 2019, before the pandemic.
Hospitals generally have struggled in recent years with high labor costs, staffing shortages and rising levels of uncompensated care, according to Rick Gundling, a senior vice president with the Healthcare Financial Management Association, a nonprofit that works with health care finance executives.
Most of their revenue is fixed, coming from government-funded programs like Medicare and Medicaid, Gundling noted. He said that means revenue growth is “only possible by increasing volumes, which is difficult even under the best of circumstances.”
Workers calling for higher wages, better working conditions and job security, especially since the end of the pandemic, have been increasingly willing to walk out on the job as employers face a greater need for workers.
The California legislature has sent Democratic Gov. Gavin Newsom a bill that would increase the minimum wage for the state’s 455,000 health care workers to $25 per hour over the next decade. The governor has until Oct. 14 to decide whether to sign or veto it.
National Hospital Flash Report: September 2023
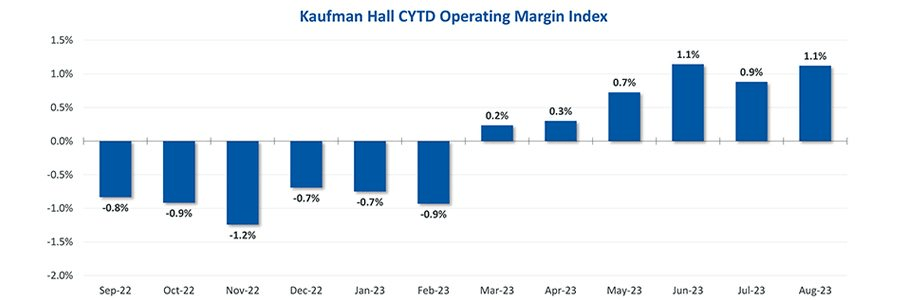
While hospital operating margins remain below historical levels, overall conditions have stabilized in 2023. The median Kaufman Hall Calendar Year-To-Date Operating Margin Index reflecting actual margins was 1.1% in August.
The September issue of the National Hospital Flash Report covers these and other key performance metrics.
DOWNLOAD REPORT
How 23 health systems’ labor costs are trending

The hospital workforce is critical to the care process and is most often the largest expense on a hospital or health system’s balance sheet. Even before the pandemic, labor expenses — which include costs associated with recruitment and retention, employee benefits and incentives — accounted for more than 50 percent of hospitals’ total expenses, according to the American Hospital Association.
As a result, a slight increase in labor costs can have a tremendous effect on a hospital or health system’s total expenses and operating margins. Hospitals across the country are focused on managing the premium cost of labor, while recruiting and retaining talent remains a priority, and the cost of supplies and drugs also increases due to inflation.
Here’s how 23 health systems’ labor costs are tracking based on the results of their most recent financial documents.
Note: This is not an exhaustive list. Most of the following health systems’ labor costs are for the three months ending 30, with others for the six months ending June 30 and the 12 months ending June 30 — the most recent periods for which financial data is available. The year-over-year percentage increase/decrease is also included.
1. HCA Healthcare Nashville, Tenn.)
Q2 salaries and benefits: $7.3 billion (+7.1 percent YOY)
2. Tenet Healthcare (Dallas)
Q2 salaries, wages and benefits: $2.3 billion (+7.5 percent YOY)
3. Community Health Systems (Franklin, Tenn.)
Q2 salaries and benefits: $1.3 billion (+3.2 percent YOY)
4. Universal Health Services (King of Prussia, Pa.)
Q2 salaries, wages and benefits: $1.8 billion (+4.7 percent YOY)
5. Mayo Clinic (Rochester, Minn.)Q2 salaries and benefits: $2.4 billion (+5.9 percent YOY)
6. SSM Health (St. Louis)
Q2 salaries and benefits: $1.1 billion. (+14.1 percent YOY)
7. Cleveland Clinic
Q2 salaries, wages and benefits: $2.1 billion (+8.9 percent YOY)
8. McLaren Health Care (Grand Blanc, Mich.)
Q2 salaries, wages, employee benefits and payroll taxes: $1.3 billion (+0.5 percent)
9. Sutter Health (Sacramento, Calif.)
Q2 salaries and employee benefits: $1.7 billion (6.7 percent YOY)
10. IU Health (Indianapolis)
Q2 salaries, wages and benefits: $1.1 billion (-1.6 percent YOY)
11. Mass General Brigham (Boston)
Q2 employee compensation and benefits: $2.4 billion (+4.2 percent YOY)
12. ProMedica (Toledo, Ohio)Q2 salaries, wages and employee benefits: $388.8 million (-2.5 percent YOY)
13. Orlando (Fla.) Health
Q2 salaries and benefits: $734.4 million (+17.9 percent YOY)
14. MultiCare Health (Tacoma, Wash)
Salaries, wages and employee benefits: $1.5 billion (+14.4 percent YOY)
*For the six months ended June 30
15. Banner Health (Phoenix)Salaries, benefits and contract labor: $3 billion (+4.7 percent YOY)
*For the six months ended June 30
16. UPMC (Pittsburgh)
Salaries, professional fees and benefits: $4.8 billion (+6.7 percent YOY)
*For the six months ended June 30
17. Northwell Health (New Hyde Park, N.Y.)
Salaries and employee benefits: $5.3 billion (+10.6 percent YOY)
*For the six months ended June 30
18. Providence (Renton, Wash.)
Salaries and benefits: $7.5 billion (+4.9 percent YOY)
*For the six months ended June 30
19. Sanford Health (Sioux Falls, S.D.)
Salaries and benefits: $1.8 billion (+2.6 percent YOY)
*For the six months ended June 30
20. Intermountain Health (Salt Lake City)
Employee compensation and benefits: $3.4 billion (+27.9 percent YOY)
*For the six months ended June 30
21. CommonSpirit Health (Chicago)
Salaries and benefits: $18.3 billion (+0.7 percent YOY)
*For the 12 months ended June 30
**Merged with Broomfield, Colo. -based SCL Health in April 2022
22. Ascension (St. Louis)
Salaries, wages and employee benefits: $14.3 billion (-1.3 percent YOY)
*For the 12 months ended June 30
23. Mercy Health (Chesterfield, Mo.)
Salaries and benefits: $4.6 billion (+5.3 percent)
*For the 12 months ended June 30

