The Supreme Court on Thursday issued an opinion upholding the Affordable Care Act by a 7-2 vote, allowing millions to keep their insurance coverage amid the coronavirus pandemic.
In the decision, the court reversed a lower court ruling finding the individual mandate unconstitutional. However, the court did not get to the key question of whether the individual mandate is severable from the rest of the law. Instead, the court held the plaintiffs do not have standing in the case, or a legal right to bring the suit.
Justice Stephen Breyer wrote the opinion while Justices Samuel Alito and Neil Gorsuch filed dissenting opinions.
Breyer wrote that a court must address a plaintiffs’ injuries. But Breyer found there were no injuries, so he asked: “What is that relief? The plaintiffs did not obtain damages.” Breyer added, “There is no one, and nothing, to enjoin.”
A wide swath of industry cheered Thursday’s news.
The American Medical Association called it a victory for patients, so too did America’s Essential Hospitals, a safety net trade group that called it a win. The American Hospital Association said the more than 30 million of Americans who obtained coverage from the law can “breathe a sigh of relief.”
Millions of Americans gained health insurance coverage as a result of the Affordable Care Act, President Barack Obama’s landmark law passed in 2010 and reshaped virtually every corner of American healthcare. The latest challenge threatened to undo coverage gains under the law that helped drive down the uninsured rate to a record low.
Proponents feared the law was in greater jeopardy following the death of Supreme Court Justice Ruth Bader Ginsburg, part of the court’s liberal wing, which shrunk to just three of a total of nine justices without her.
Those fears now seem to be overblown. Chief Justice John Roberts joined the courts liberals in upholding the law, as did two of President Donald Trump’s Supreme Court picks, Justices Brett Kavanaugh and Amy Coney Barrett.
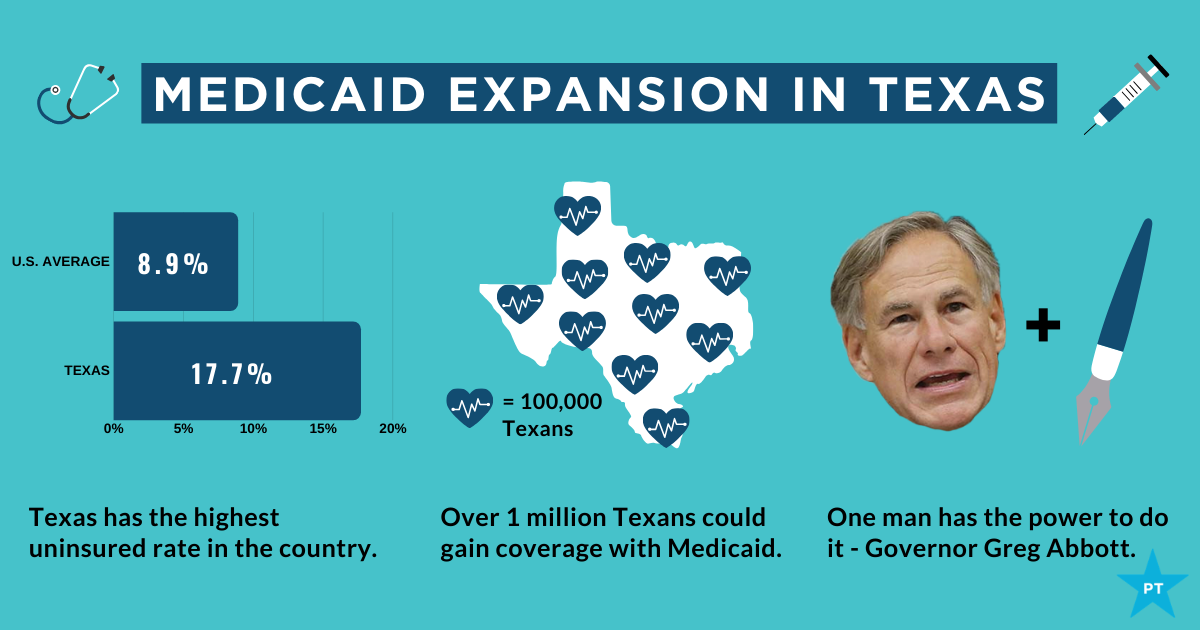
In a rare move, Trump’s DOJ declined to defend the ACA, when the challenge was brought by a group of red states and two men with marketplace plans. Former California Attorney General Xavier Becerra, now HHS secretary, led a group of blue states to defend the law in federal court.
Recap of the controversial case
The case centers on the individual mandate, the part of the law that compelled Americans to purchase health insurance or pay a fee. The framers of the ACA believed the mandate would help drive healthy people to ensure they weren’t just filled with sick people, risking higher costs and adverse selection for insurers.
Congress effectively killed the mandate in 2017 by setting the penalty to $0.
The plaintiffs’ legal argument was strategic. They directly targeted the linchpin that saved the law in 2012. The Supreme Court largely upheld the ACA in 2012 when it ruled the mandate could be considered a tax and therefore was constitutional. Roberts infuriated conservatives by siding with liberals in that case.
Take that penalty away, by zeroing it out, and the plaintiffs argue the law is no longer constitutional because it can no longer be considered a tax if no money is collected.
The key question before the Supreme Court was whether they could simply pluck the individual mandate from the remainder of the monumental health law, throw the entire law out or find some middle ground.
The plaintiffs have argued that the individual mandate is so intertwined and closely linked to the rest of the law that the entire piece of legislation must fall if the individual mandate is ruled unconstitutional.
Before arriving at the Supreme Court, a lower court ruled in 2019 the mandate was unconstitutional but sent back the key question of whether the mandate could be extracted from the remainder of the law back to the district court. The federal appeals court ruling by a three-judge panel came down along party lines: two Republicans and one Democrat.
A question of standing
Some legal experts have criticized the challenge because the individual plaintiffs, two Texas men, no longer face any financial penalty if they were to forgo coverage. SCOTUS’ ruling agrees with that logic.
The two men joined the case originally brought by a group of red states. Legal experts said it would have been harder for the group of red states to prove an injury than the two men, John Nantz and Neill Hurley.
The court seemed skeptical of whether the plaintiffs had standing to bring the case during oral arguments in November. Justices spent a large portion of the two-hour hearing on the topic.
The word standing was mentioned at least 59 times, according to the court’s transcript of the hearing, outnumbering other key words such as severability, another important legal concept in the case.
In one now-telling exchange from oral arguments, Gorsuch seemed confused over the premise of the challenge to begin with: “I guess I’m a little unclear who exactly they want me to enjoin and what exactly do they want me to enjoin them from doing?”