Covid-19 death rates in the United States are “eye-wateringly” high compared with other wealthy nations—a problem that several health experts say underscores the shortfalls of the country’s pandemic response.
U.S. Covid-19 death rates exceed those of other wealthy nations
According to CDC data, over 880,000 Americans have died from Covid-19 since the beginning of the pandemic—a death toll greater than that of any other country. And during the current omicron wave, Covid-19 deaths are now greater than the peak number seen during the delta wave and more than two-thirds as high as record numbers seen last winter before vaccines were available, the New York Times reports.
Moreover, since Dec. 1, when omicron was first detected in the United States, the proportion of Americans who have died from Covid-19 has been at least 63% higher than other large, wealthy countries, including Britain, Canada, France, and Germany, according to a Times analysis of mortality figures.
Currently, the daily Covid-19 death rate in the United States is nearly double that of Britain and four times that of Germany. The only large European countries to surpass the United States’ Covid-19 death rates have been the Czech Republic, Greece, Poland, Russian, and Ukraine—all of which are less wealthy nations where the most effective treatments may be limited.
“Death rates are so high in the States—eye-wateringly high,” said Devi Sridhar, head of the global public health program at the University of Edinburgh. “The United States is lagging.”
Similarly, Joseph Dieleman, an associate professor at the University of Washington, said the United States “stands out” with its high Covid-19 death rate. “There’s been more loss than anyone wanted or anticipated,” he said.
Vaccination shortfalls plague the U.S.
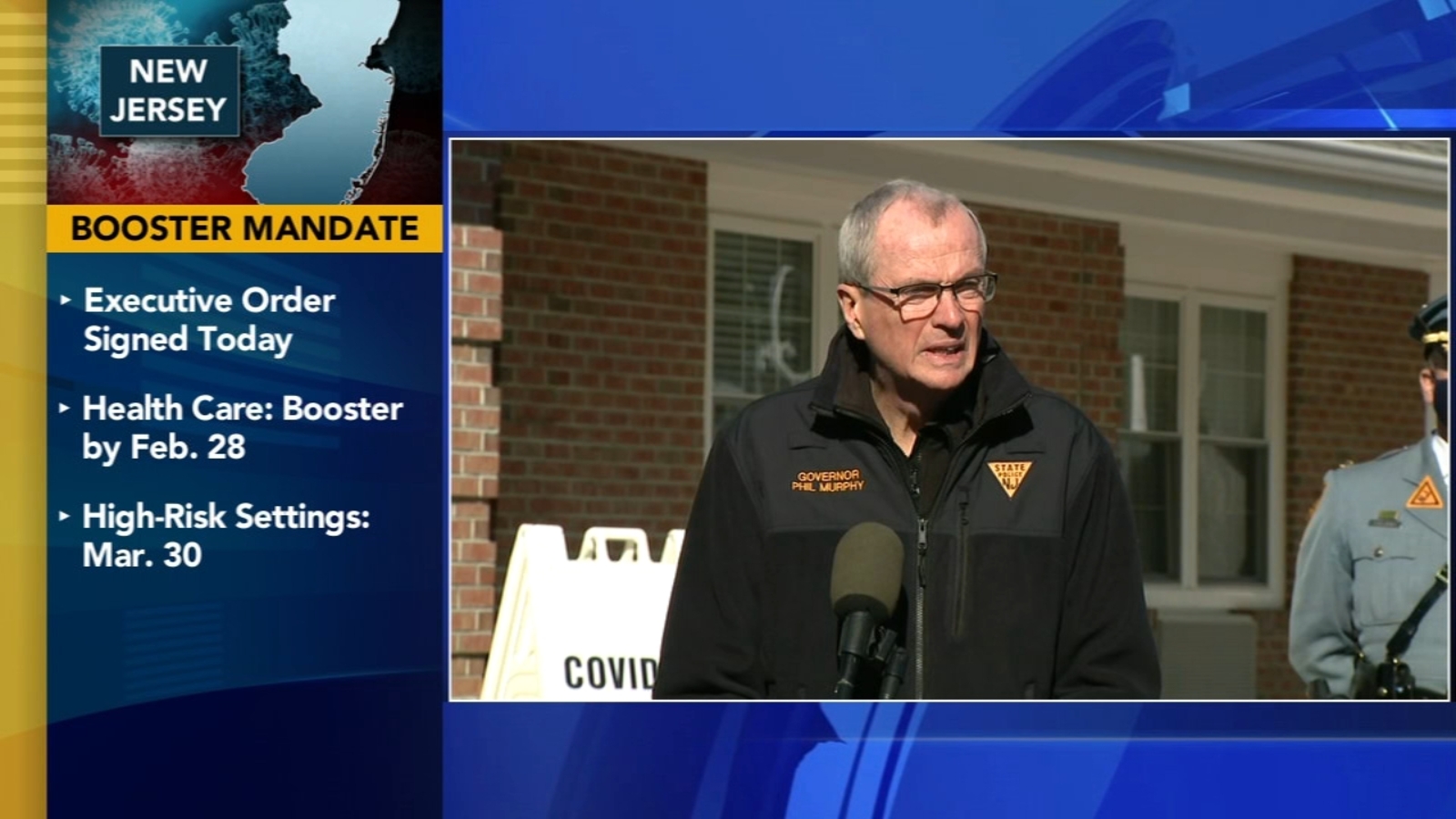
Lagging Covid-19 vaccination rates among Americans likely contributed to the country’s outsized death toll compared with other nations, several health experts said.
Currently, around 64% of the U.S. population has been fully vaccinated. However, several peer countries, including Australia (80%), Canada (80%), and France (77%), have achieved higher vaccination rates.
Unvaccinated people make up the majority of hospitalized Covid-19 patients, according to the Times, but lagging vaccination and booster rates among vulnerable groups, such as older Americans, has also led to increased hospitalizations.
Around 12% of Americans ages 65 and older are not fully vaccinated, and among those who are fully vaccinated, 43% still have not received a booster shot, leaving them with waning immunity against the omicron variant. In comparison, only 4% of Britons ages 65 and older are not fully vaccinated, and only 9% have not had a booster shot.
“It’s not just vaccination—it’s the recency of vaccines, it’s whether or not people have been boosted, and also whether or not people have been infected in the past,” said Lauren Ancel Meyers, director of the University of Texas at Austin’s Covid-19 modeling consortium.
Similarly, former FDA Commissioner Scott Gottlieb said that the United States‘ lagging vaccination rates compared to the U.K.’s, particularly for boosters, may be due to “protracted wrangling” that “may have sowed confusion, sapping consumer interest.”
How the U.S. could fare in future Covid-19 waves
According to some scientists, the gap between the United States and other wealthy nations may soon begin to narrow. Although U.S. vaccination rates have been slow, the delta and omicron waves have infected so many people that overall immunity against the coronavirus has increased—which could potentially help blunt the effect of future waves.
“We’ve finally started getting to a stage where most of the population has been exposed either to a vaccine or the virus multiple times by now,” said David Dowdy, an epidemiologist at the Johns Hopkins Bloomberg School of Public Health. “I think we’re now likely to start seeing [American and European Covid-19 death rates] be more synchronized going forward.”
However, other experts noted that the United States has other disadvantages that could make future Covid-19 waves difficult. For example, many Americans have chronic health problems, such as diabetes and obesity, that increase the risk of severe Covid-19 outcomes.
Overall, health experts said the impact of future Covid-19 waves will depend on what new variants emerge, as well as what level of death people decide is tolerable.
“We’ve normalized a very high death toll in the U.S.,” said Anne Sosin, who studies health equity at Dartmouth University. “If we want to declare the end of the pandemic right now, what we’re doing is normalizing a very high rate of death.”