https://www.axios.com/2025/07/01/real-cost-health-coverage-losses
Nearly 12 million people would lose their health insurance under President Trump’s “big, beautiful bill,” an erosion of the social safety net that would lead to more unmanaged chronic illnesses, higher medical debt and overcrowding of hospital emergency departments.
Why it matters:
The changes in the Senate version of the bill could wipe out most of the health coverage gains made under the Affordable Care Act and slash state support for Medicaid and SNAP.
- “We are going back to a place of a lot of uncompensated care and a lot of patchwork systems for people to get care,” said Ellen Montz, a managing director at Manatt Health who oversaw the ACA federal marketplace during the Biden administration.
The big picture:
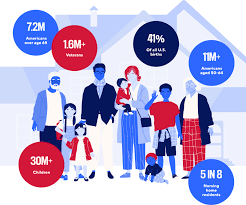
The stakes are huge for low-income and working-class Americans who depend on Medicaid and subsidized ACA coverage.
- Without health coverage, more people with diabetes, heart disease, asthma and other chronic conditions will likely go without checkups and medication to keep their ailments in check.
- Those who try to keep up with care after losing insurance will pay more out of pocket, driving up medical debt and increasing the risk of eviction, food insecurity and depleted savings.
- Uninsured patients have worse cancer survival outcomes and are less likely to get prenatal care. Medicaid also is a major payer of behavioral health counseling and crisis intervention.
Much of the coverage losses from the bill will come from new Medicaid work reporting requirements, congressional scorekeepers predict. Work rules generally will have to be implemented for coverage starting in 2027, but could be earlier or later depending on the state.
- Past experiments with Medicaid work rules show that many eligible people fall through the cracks verifying they’ve met the requirements or navigating new state bureaucracies.
- Often, people don’t find out they’ve lost coverage until they try to fill a prescription or see their doctor. States typically provide written notices, but contacts can be out of date.
- Nearly 1 in 3 adults who were disenrolled from Medicaid after the COVID pandemic found out they no longer had health insurance only when they tried to access care, per a KFF survey.
Zoom out:
The Medicaid and ACA changes will also affect people who keep their coverage.
- The anticipated drop-off in preventive care means the uninsured will be more likely to go to the emergency room when they get sick. That could further crowd already bursting ERs, resulting in even longer wait times.
- Changes to ACA markets in the bill, along with the impending expiration of enhanced premium subsidies, may drive healthier people to drop out, Montz said, skewing the risk pool and driving up premiums for remaining enrollees.
- States will likely have to make further cuts to their safety-net programs if the bill passes in order to keep state budgets functioning with less federal Medicaid funding.
The other side:
The White House and GOP proponents of the bill say the health care changes will fight fraud, waste and abuse, and argue that coverage loss projections are overblown.
- Conservative health care thinkers also posit that there isn’t strong enough evidence that public health insurance improves health.
Reality check:
Not all insurance is created equally, and many people with health coverage still struggle to access care. But the bill’s impact would take the focus off ways to improve the health system, Montz said.
- “This is taking us catastrophically backward, where we don’t get to think about the things that we should be thinking about how to best keep people healthy,” she said.
The bottom line:
The changes will unfold against a backdrop of Health Secretary Robert F. Kennedy Jr.’s purported focus on preventive care and ending chronic illness in the U.S.
- But American health care is an insurance-based system, said Manatt Health’s Patricia Boozang. Coverage is what unlocks access.
- Scrapping millions of people’s health coverage “seems inconsistent with the goal of making America healthier,” she said.