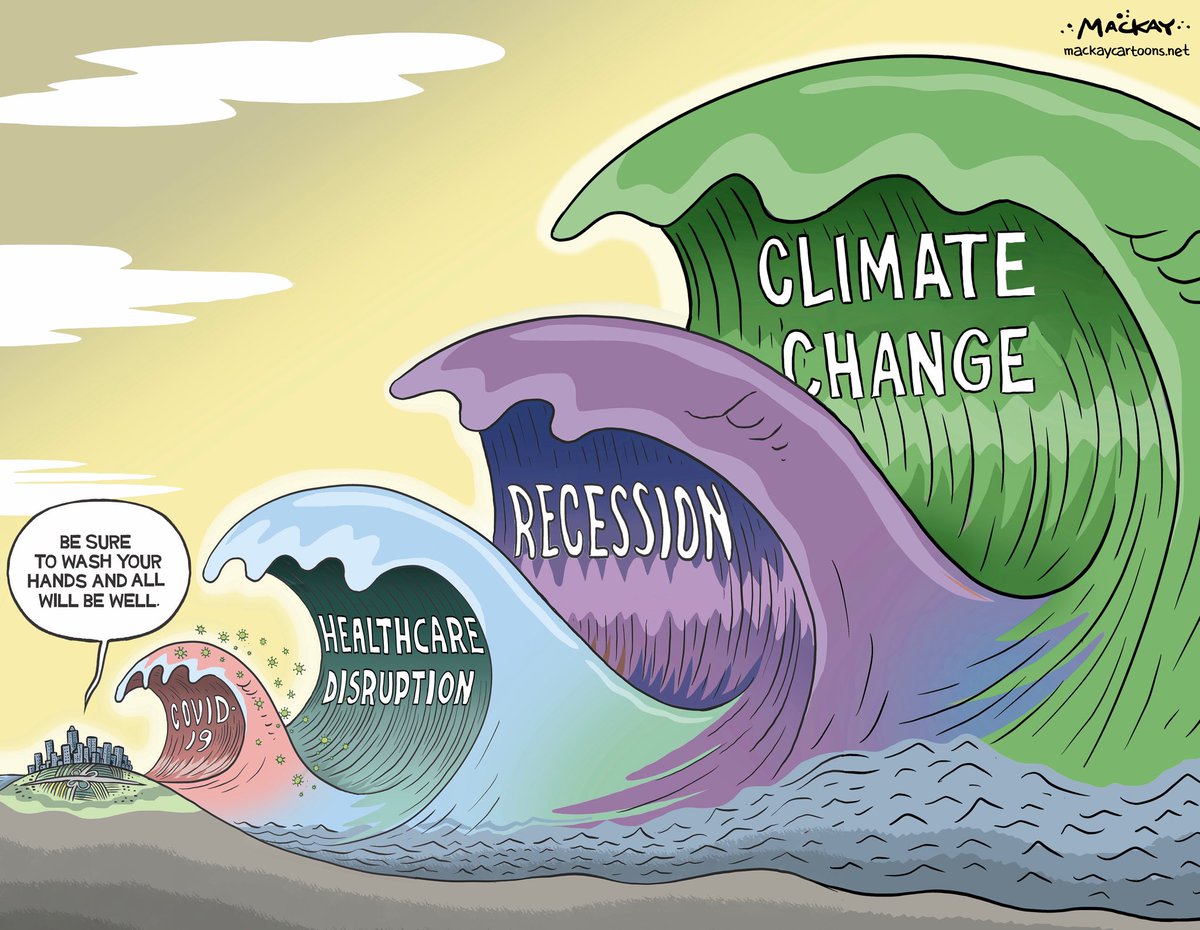
Another challenging year defined by the continued COVID-19 fight and vaccination drives has created a unique healthcare landscape. Pandemic-induced telehealth booms, continued strain due to understaffing and pressure from big tech disruptors are just some of the issues that have presented themselves this year.
Here are five major trends that hospitals and health systems may see in 2022. While some present challenges, others present significant opportunities for healthcare facilities.
Workforce pressure
Record numbers of workers have quit their jobs in 2021, with some 4.4 million people quitting in September. That means that 1 in 4 people quit their jobs this year across all industries. Around 1 in 5 healthcare workers have left their positions, creating issues with understaffing and lack of resources in hospitals and health systems. Stress, burnout and lack of balance have all been cited as reasons for staff leaving their roles. An increase in violence toward medical professionals, continued COVID-19 surges and low pay and benefits have contributed to the exodus of healthcare workers. None of those problems seems poised to disappear come 2022, so the new year could bring continued workforce and staffing challenges.
Pressure from disruptors
Big tech and retail giants have continued their push into healthcare this year. Companies like Apple, Amazon and Google stepped up their game in the wearables market. Pharmacy and retail chains Walmart and CVS Health both detailed their intended expansions into primary care. The pandemic also encouraged big corporations outside the healthcare sector, like Pepsi and Delta Airlines, to consider hiring CMOs to make sense of public health regulations guide them on their policy. These moves all mean there is a tightening of competition for the top physicians and hospital executives. Going into 2022, health systems may be under pressure to hang onto top talent and keep patients from using other convenient health services offered by retail giants.
Health equity
The unequal toll of the pandemic on people of color both medically and economically helped shed a light on the rampant inequities in American healthcare and society at large. Indigineous, Black and Hispanic people were much more likely than white or Asian people to suffer severe illness or require hospitalization as a result of COVID-19. Increasing numbers of hospitals, health systems and organizations are starting initiatives to advance health equity and focus on the socioeconomic drivers of health. The American Medical Association launched a language guide to encourage greater awareness about the power of language. Z-code usage has also been encouraged by CMS to increase knowledge and data about the social determinants of health. Next year, the perspective of health as holistic instead of just a part of an individual’s life will continue, with special attention being paid to social drivers.
Telehealth expansion
The pandemic helped the telemedicine industry take off in a big way. Telehealth was often the only healthcare option for many patients during the height of the lockdown measures introduced during the pandemic. Despite a return to in-person visits, telehealth has retained its popularity with patients. Some advocates argue that telehealth can help increase access to healthcare and improve health equity. About 40 percent of patients said that telehealth makes them more engaged and interact more frequently with their providers. However, while Americans see telehealth as the future of healthcare, a majority still prefer in-person visits. Regardless of patient opinion, telehealth will remain a key part of health strategy. In late December, the FCC approved $42.7 million in funding for telehealth for 68 healthcare providers. This suggests that there are investments and subsidies available in the future for health systems to bolster their telehealth services.
Climate change
At the 2021 UN Climate Conference, Cop26, in Glasgow, Scotland, hospitals and health systems acknowledged the role they have to play in mitigating the effects of climate change. Hospitals and health systems shed light on the health-related effects of climate change, such as illness and disease from events like wildfires and extreme weather. Health systems are also becoming more aware of their own contributions to climate change, with the U.S. healthcare system emitting 27 percent of healthcare emissions worldwide. To that end, HHS created an office of climate change and health equity that will work alongside regulators to reduce carbon emissions from hospitals. More health systems too are taking charge and pledging net neutrality and zero carbon emissions goals, including Kaiser Permanente and UnitedHealth group. It’s expected that more systems will follow suit in the coming year and make more concrete plans to address emissions reduction.