MA pays 10% to 15% less than what is paid by the government in original Medicare, report says.
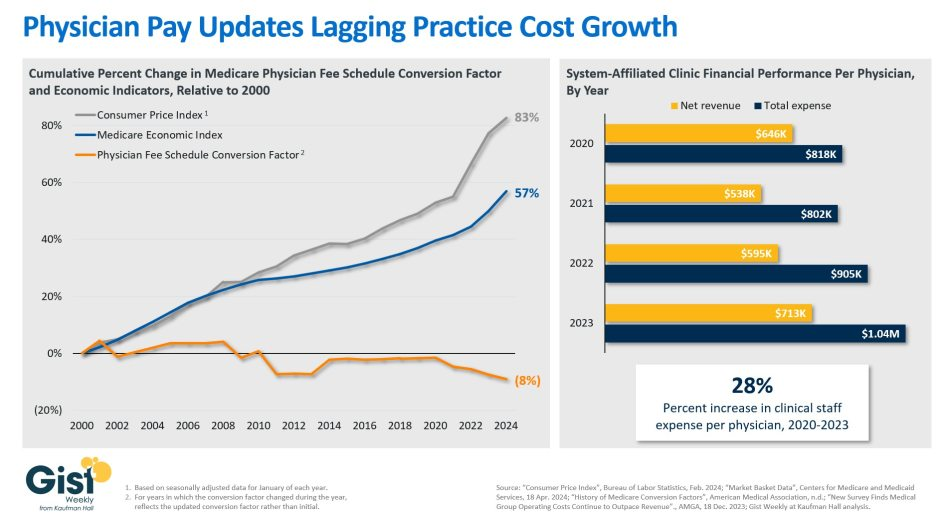
A new study confirms what the American Medical Association and other medical groups have long been saying about physician pay: Medicare reimbursement is not keeping up with inflation.
In original Medicare, doctors are paid one-third less than a decade ago, the report said. Medicare reimbursement rates for outpatient procedures have decreased every year since 2016, for an overall decline of 10%.
Over the same period, inflation has risen by almost 30%, according to the report.
The report also sheds light on Medicare Advantage reimbursement. Medicare Advantage plans pay physicians an estimated 10% to 15% less than what is paid by the government in traditional Medicare, according to the 2025 Omniscient Health Physician Medicare Income Report.
This can create negative margins for physicians considering MA plans take roughly twice as long to reimburse providers compared to original Medicare along with factoring in prior authorization and denials, the report said.
An estimated 54% of Medicare beneficiaries are enrolled in a MA plan.
WHY THIS MATTERS
The MA reimbursement gap is driving shifts in network participation. A 2024 survey by the Healthcare Financial Management Association found that 19% of health systems have stopped accepting at least one MA plan, with another 61% planning to do so or actively considering it, according to the Omniscient report.
“Despite the rising demand for care from an aging U.S. population, the financial strain is forcing physicians to rethink whether they will continue serving Medicare patients,” said Meade Monger, CEO of Omniscient Health, a healthcare data science company. “High-volume Medicare practices, especially those in primary care and rural areas, are increasingly unable to sustain operations under current revenue structures.”
The federal government’s push toward streamlining and speeding up the prior authorization process and requiring an electronic process over paper represents improvement, the report said. Some insurers have announced plans to decrease the number of procedures that require prior auth.
But payment rates need to change, said Omniscient, which recommends policymakers index Medicare reimbursement rates to inflation and set payment standards for MA plans.
THE LARGER TREND
On Tuesday, the American Medical Association released what it called flawed proposals in the Centers for Medicare and Medicaid Services’ physician payment rule released in July.
Despite getting a 3.6% payment boost after five consecutive years of cuts, physician pay, after adjusting for practice-cost inflation, has plummeted since 2001, the AMA said.
The proposed 2026 Medicare Physician Fee Schedule includes a 2.5% cut in work relative-value units (RVUs, which measure a physician’s time, technical skill, mental effort, decision-making and stress) and physician intraservice time for most services, the AMA said. This reduction would affect 95% of the services that doctors provide.
The cut is based on an assumption of greater efficiency and less time involved for each service, an assumption that is not grounded in new data or physician input, the AMA said.
CMS also proposes a reduction in practice-expense RVUs, which are the costs of running a practice, such as staff, equipment, supplies, utilities and overhead.
The bottom line, the AMA said, is that physician payment for services performed in a facility will drop overall by 7%.
CMS is accepting comments on its proposed rule until Sept. 12.