The Nelson A. Rockefeller Institute of Government is a public policy think tank founded in 1981 that conducts cutting-edge research and analysis to inform lasting solutions to the problems facing New York State and the nation.
Introduction & Definitions
In 2023, I noted 10 trends within three broad categories in healthcare worth watching and provided a mid-year update on those trends. They included: the impact of unwinding the Public Health Emergency on insurance coverage, healthcare workforce shortages, price inflation, declining margins at hospitals, private equity in healthcare, consolidations, alternate payment models, attention to health equity, digital telehealth expansion, and the expansion of non-traditional providers in healthcare. These trends continue to be worth watching in 2024.
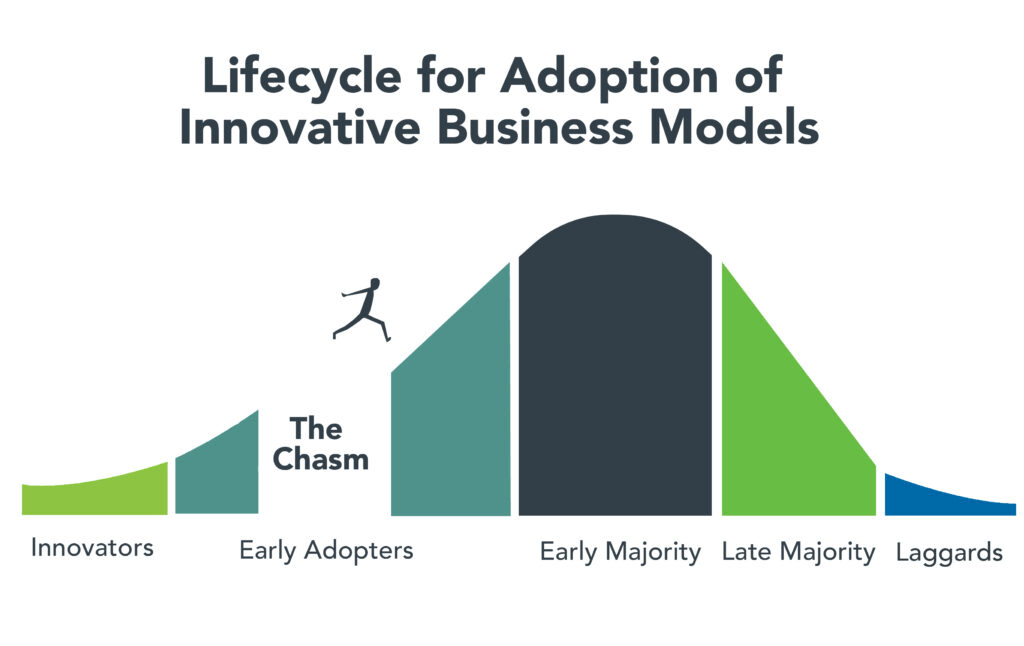
More significant than any one of these trends is the combined interaction of the trends in the industry overall—what I’ll call a “mega-trend,” which results in a trifurcation of the industry. Currently, there are parts of the healthcare industry struggling to exist. This is due to different factors, including high expenses, staffing challenges, and a lack of access to capital and technology, among other things. I call the types of healthcare entities that fall into this category “Today” entities because they exist now but may or may not exist in the future. In contrast, there is another set of entities in healthcare that have emerged in the last five or so years. They are becoming larger through consolidation and integration, and have greater access to capital and technology. I call these types of healthcare entities the “Tomorrow” entities because their size, resources, and forward-looking strategies are changing the future of healthcare.
In between these two categories, are existing and traditional entities in healthcare that seek sustaining strategies. I call these entities the “Striving Survivors” whose success and ability to persevere is still an open question. Most look like the healthcare entities of Today, but what distinguishes them is their ability to partner, use technology, and diversify what they offer. To understand the mega–trend phenomena of this trifurcation in healthcare and what’s happening within and across each of these three categories, this blog dissects how the trends I highlighted in 2023 are impacting the Today and the Tomorrow entities and discusses how the Striving Survivors are attempting to keep pace as the healthcare industry evolves.
The “Today” Healthcare Entities
As noted in my 2023 blog, price inflation and expense growth—particularly as they relate to workforce and labor costs—were two trends impacting existing healthcare organizations. Today’s healthcare entities are heavily reliant on people, and, unsurprisingly, increased expenses for personnel, which had a major impact on organizations’ bottom lines for the past few years, as did general inflation and increased supply prices. However, for some providers, revenue and patient volume have returned to levels comparable to pre–pandemic. According to Kaufman Hall, a healthcare consulting firm, by the end of 2023, some hospitals’ margins were beginning to stabilize.
In looking at what may happen in 2024 for providers, however, the return of patient volume and, therefore, more predictable revenue may not be enough to yield positive margins. This is because expenses are predicted to be challenging. Industry experts estimate that healthcare prices will grow 7 percent in the coming year. The estimate reflects increases in pharmaceutical costs, growing provider expenses given the high labor and supply costs noted earlier, and insurer rate increases.
Another challenge to the healthcare entities of Today is the availability of capital to make strategic investments. More of this capital is now being provided by private equity firms, an estimated $750 billion in the last decade. To secure capital in the private market, bond rating agencies typically favor larger providers because they are less risky. This, among other factors, has contributed to growing consolidation in the industry among physician groups, insurers, and hospitals. Not only do these entities need capital for projects like upgrades to existing facilities, but to also make strategic investments. Such investments include acquisitions of other providers or companies that add to the revenue base, or technologies that allow improvements in care delivery.
The Today entities are increasingly challenged with adapting to consumer demands for tech–enabled care options. Consumers want more tech–supported smart applications that allow them to book appointments or get assistance with care more quickly via chatbots. Consumers also want new options for care at home—including hospital–at–home, which provides acute care in a home-based setting, and home–based care. As noted in my November blog on AI in healthcare, access to such technologies is not only creating further separation between healthcare entities, but can also create further inequities among consumers.
The “Tomorrow” Healthcare Entities
With the challenges for the healthcare entities of Today outlined above, it is important to note that those same challenges are not as significant for the healthcare players of Tomorrow. This is because most are substantial in size and have sufficient revenue, technology, and capital resources—often in the form of private equity. And many of them did not start in healthcare. They include, for example, Amazon—which started as an online bookstore and now has annual revenues of over $500 billion, CVS—which started as a retail pharmacy and now has revenues close to $300 billion; Uber—which started as a tech-enabled taxi-like transport application and now has revenues of over $30 billion, and Microsoft—which started as computer company but has expanded into healthcare with annual revenues of over $200 billion.
Some of these companies have entered healthcare by partnering with, or acquiring companies already in the sector such as Amazon’s 2023 acquisition of One Medical, a tech–enabled primary care entity; the 2022 partnership between United Health Group and Change Healthcare, a technology company; and CVS’s official 2023 acquisition of Signify, a home health organization. This was on top of CVS’s earlier (2018) merger with health insurance company Aetna, and its 2022 partnership announcement with Uber with the stated aim of improving access to care and decreasing health inequities in underserved communities across the country. Other entities have increased their footprint in healthcare by launching their products, such as Microsoft’s 2020 launch of Cloud services, specifically for healthcare. Some of these companies are now collaborating, including the 2021 partnership between CVS Health and Microsoft, which was designed to customize care further, enable frontline workers to more easily access and use data, and digitize operations.
In addition to these large nontraditional healthcare entities, the health insurance industry has also experienced large–scale consolidation and diversification that enables them to compete. One of the most notable companies in the world of healthcare integration is the nation’s largest insurer, United Health Group (UHG). UHG continued to outpace provider margins, with 2023 third quarter margins for UHG at levels 14 percent higher year-over-year. The continued growth at UHG was largely due to the increasing number of individuals served and a growing provider base of 90,000 physicians, or 10 percent of all physicians nationwide. This contrasts with one of the largest provider margins (Kaiser) whose 2023 third-quarter margin was only $239 million, an improvement from the $1.5 billion loss they experienced in the third quarter from the previous year. Although no other insurers are as big as UHG, the next biggest including, Aetna, Anthem, Cigna, and Humana all had 2023 third–quarter net incomes ranging from $1 billion to $1.4 billion.
The Striving Survivors
Not all traditional healthcare entities are being left behind; I call these the Striving Survivors. They may currently be considered Today entities, but they are attempting to put in place strategies so they can be Tomorrow entities in the future. Here are three primary strategies that may help these entities survive into the future:
- Partnering—The number of independent hospitals as well as the number of independent physician groups has shrunk dramatically in the past decade, and there is increasing pressure for both to consider merging. A report by Kaufman Hall prepared at the request of the American Hospital Association, shows that merging can have advantages such as creating economies of scale, improving leverage to bargain for better payments from increasingly large insurance companies, and allowing better access to capital markets. Other advantages to partnering include diversifying what services can be offered to patients, allowing providers to assume risk for the care of a larger population, or leveraging complementary strengths for strategic investments. Although many of these consolidations used to be regional in nature (providers would merge with neighboring providers), new mergers are occurring across broader geographic areas, as was the case with the merger of west–coast–based Kaiser and Pennsylvania-based Geisinge.
- Maximizing Technology—Striving Survivors are also seeking to compete and survive into the future by partnering to maximize technology. Technologies like telehealth, remote monitoring, artificial intelligence, and hospital–at–home, are growing because they are delivering care in ways that are preferable to consumers. As recently noted by Deloitte, “Adopting new technologies and business models—while under sustained financial pressure—might be the biggest challenge health care executives will face in 2024.” The good news for the healthcare players of Today is the use of data and technology in new and creative ways can counteract some of their current financial and care delivery challenges. Technology can make care more convenient for consumers, reduce costs, or provide care in places where it is sometimes inaccessible. Some recent examples of partnerships between technology companies and today’s healthcare entities include women’s health tech startup Tia’s partnership with Common Spirit, one of the largest healthcare systems in the country. Similarly, Strive Health is managing kidney patients for Bon Secours Mercy Health; Carbon Health is providing tech–enabled urgent care for Milwaukee–based Froedtert Health. Even Best Buy, a home electronics store, has begun offering homecare through several partnerships, including, for example, Mass General Brigham.
- Revenue Diversification—Revenue diversification has long been a growth strategy in many industries. Up until recently, there hasn’t been the same pressure for such diversification for healthcare entities. That is changing, in part, because many of the healthcare entities of Tomorrow come from non–health–related industries. Diversification can occur using either of the strategies noted above (partnership or maximizing the use of technology). Diversification might also include providing services in areas of healthcare where demand is growing (e.g. urgent care or outpatient instead of legacy inpatient services). It might also include services that are not currently widely used but are likely to become more commonplace in the future, such as precision medicine or hospital–at–home.
Conclusion
In 2024, it will not only be important for healthcare policymakers to monitor single trends such as the continued focus on health equity, the expansion of alternate payment models, or the cost of the healthcare workforce, but it will also be important to understand how trends may be interacting with each other to create larger market trends. Such is the case for the emergence of non-traditional players in healthcare, the influx of private equity, digital expansion, and major consolidations— which when combined —are resulting in a mega trend of trifurcation of the industry into Today, Tomorrow, and Striving entities in healthcare that are seeking to survive into the future. For healthcare policymakers, all these trends along with their interaction will be worth monitoring and understanding so that effective policies can be developed that result in a healthcare system that supports innovation, protects patients, reduces inequities, and results in better health outcomes at lower cost.