https://www.npr.org/sections/health-shots/2022/06/16/1104679219/medical-bills-debt-investigation

Elizabeth Woodruff drained her retirement account and took on three jobs after she and her husband were sued for nearly $10,000 by the New York hospital where his infected leg was amputated.
Ariane Buck, a young father in Arizona who sells health insurance, couldn’t make an appointment with his doctor for a dangerous intestinal infection because the office said he had outstanding bills.
Allyson Ward and her husband loaded up credit cards, borrowed from relatives, and delayed repaying student loans after the premature birth of their twins left them with $80,000 in debt. Ward, a nurse practitioner, took on extra nursing shifts, working days and nights.
“I wanted to be a mom,” she said. “But we had to have the money.”
The three are among more than 100 million people in America ― including 41% of adults ― beset by a health care system that is systematically pushing patients into debt on a mass scale, an investigation by KHN and NPR shows.
The investigation reveals a problem that, despite new attention from the White House and Congress, is far more pervasive than previously reported. That is because much of the debt that patients accrue is hidden as credit card balances, loans from family, or payment plans to hospitals and other medical providers.
To calculate the true extent and burden of this debt, the KHN-NPR investigation draws on a nationwide poll conducted by KFF (Kaiser Family Foundation) for this project. The poll was designed to capture not just bills patients couldn’t afford, but other borrowing used to pay for health care as well. New analyses of credit bureau, hospital billing, and credit card data by the Urban Institute and other research partners also inform the project. And KHN and NPR reporters conducted hundreds of interviews with patients, physicians, health industry leaders, consumer advocates, and researchers.
The picture is bleak.
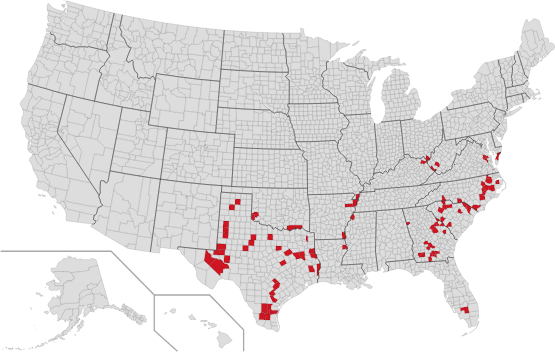
Where medical debt hits the hardest in the U.S.
The share of people with medical or dental bills in collections varies widely from one county to another
In the past five years, more than half of U.S. adults report they’ve gone into debt because of medical or dental bills, the KFF poll found.
A quarter of adults with health care debt owe more than $5,000. And about 1 in 5 with any amount of debt said they don’t expect to ever pay it off.
“Debt is no longer just a bug in our system. It is one of the main products,” said Dr. Rishi Manchanda, who has worked with low-income patients in California for more than a decade and served on the board of the nonprofit RIP Medical Debt. “We have a health care system almost perfectly designed to create debt.”
The burden is forcing families to cut spending on food and other essentials. Millions are being driven from their homes or into bankruptcy, the poll found.
Medical debt is piling additional hardships on people with cancer and other chronic illnesses. Debt levels in U.S. counties with the highest rates of disease can be three or four times what they are in the healthiest counties, according to an Urban Institute analysis.
The debt is also deepening racial disparities.
And it is preventing Americans from saving for retirement, investing in their children’s educations, or laying the traditional building blocks for a secure future, such as borrowing for college or buying a home. Debt from health care is nearly twice as common for adults under 30 as for those 65 and older, the KFF poll found.

Perhaps most perversely, medical debt is blocking patients from care.
About 1 in 7 people with debt said they’ve been denied access to a hospital, doctor, or other provider because of unpaid bills, according to the poll. An even greater share ― about two-thirds ― have put off care they or a family member need because of cost.
“It’s barbaric,” said Dr. Miriam Atkins, a Georgia oncologist who, like many physicians, said she’s had patients give up treatment for fear of debt.
Patient debt is piling up despite the landmark 2010 Affordable Care Act.
The law expanded insurance coverage to tens of millions of Americans. Yet it also ushered in years of robust profits for the medical industry, which has steadily raised prices over the past decade.
Hospitals recorded their most profitable year on record in 2019, notching an aggregate profit margin of 7.6%, according to the federal Medicare Payment Advisory Committee. Many hospitals thrived even through the pandemic.
But for many Americans, the law failed to live up to its promise of more affordable care. Instead, they’ve faced thousands of dollars in bills as health insurers shifted costs onto patients through higher deductibles.
Now, a highly lucrative industry is capitalizing on patients’ inability to pay. Hospitals and other medical providers are pushing millions into credit cards and other loans. These stick patients with high interest rates while generating profits for the lenders that top 29%, according to research firm IBISWorld.
Patient debt is also sustaining a shadowy collections business fed by hospitals ― including public university systems and nonprofits granted tax breaks to serve their communities ― that sell debt in private deals to collections companies that, in turn, pursue patients.
“People are getting harassed at all hours of the day. Many come to us with no idea where the debt came from,” said Eric Zell, a supervising attorney at the Legal Aid Society of Cleveland. “It seems to be an epidemic.”
In debt to hospitals, credit cards, and relatives
America’s debt crisis is driven by a simple reality: Half of U.S. adults don’t have the cash to cover an unexpected $500 health care bill, according to the KFF poll.
As a result, many simply don’t pay. The flood of unpaid bills has made medical debt the most common form of debt on consumer credit records.
As of last year, 58% of debts recorded in collections were for a medical bill, according to the Consumer Financial Protection Bureau. That’s nearly four times as many debts attributable to telecom bills, the next most common form of debt on credit records.
But the medical debt on credit reports represents only a fraction of the money that Americans owe for health care, the KHN-NPR investigation shows.
- About 50 million adults ― roughly 1 in 5 ― are paying off bills for their own care or a family member’s through an installment plan with a hospital or other provider, the KFF poll found. Such debt arrangements don’t appear on credit reports unless a patient stops paying.
- One in 10 owe money to a friend or family member who covered their medical or dental bills, another form of borrowing not customarily measured.
- Still more debt ends up on credit cards, as patients charge their bills and run up balances, piling high interest rates on top of what they owe for care. About 1 in 6 adults are paying off a medical or dental bill they put on a card.
How much medical debt Americans have in total is hard to know because so much isn’t recorded. But an earlier KFF analysis of federal data estimated that collective medical debt totaled at least $195 billion in 2019, larger than the economy of Greece.
The credit card balances, which also aren’t recorded as medical debt, can be substantial, according to an analysis of credit card records by the JPMorgan Chase Institute. The financial research group found that the typical cardholder’s monthly balance jumped 34% after a major medical expense.
Monthly balances then declined as people paid down their bills. But for a year, they remained about 10% above where they had been before the medical expense. Balances for a comparable group of cardholders without a major medical expense stayed relatively flat.
It’s unclear how much of the higher balances ended up as debt, as the institute’s data doesn’t distinguish between cardholders who pay off their balance every month from those who don’t. But about half of cardholders nationwide carry a balance on their cards, which usually adds interest and fees.
Bearing the burden of debts large and small
For many Americans, debt from medical or dental care may be relatively low. About a third owe less than $1,000, the KFF poll found.
Even small debts can take a toll.
Edy Adams, a 31-year-old medical student in Texas, was pursued by debt collectors for years for a medical exam she received after she was sexually assaulted.
Adams had recently graduated from college and was living in Chicago.
Police never found the perpetrator. But two years after the attack, Adams started getting calls from collectors saying she owed $130.58.
Illinois law prohibits billing victims for such tests. But no matter how many times Adams explained the error, the calls kept coming, each forcing her, she said, to relive the worst day of her life.
Sometimes when the collectors called, Adams would break down in tears on the phone. “I was frantic,” she recalled. “I was being haunted by this zombie bill. I couldn’t make it stop.”
Health care debt can also be catastrophic.
Sherrie Foy, 63, and her husband, Michael, saw their carefully planned retirement upended when Foy’s colon had to be removed.
After Michael retired from Consolidated Edison in New York, the couple moved to rural southwestern Virginia. Sherrie had the space to care for rescued horses.
The couple had diligently saved. And they had retiree health insurance through Con Edison. But Sherrie’s surgery led to numerous complications, months in the hospital, and medical bills that passed the $1 million cap on the couple’s health plan.
When Foy couldn’t pay more than $775,000 she owed the University of Virginia Health System, the medical center sued, a once common practice that the university said it has reined in. The couple declared bankruptcy.
Illinois law prohibits billing victims for such tests. But no matter how many times Adams explained the error, the calls kept coming, each forcing her, she said, to relive the worst day of her life.
Sometimes when the collectors called, Adams would break down in tears on the phone. “I was frantic,” she recalled. “I was being haunted by this zombie bill. I couldn’t make it stop.”
Nearly half of Americans in households making more than $90,000 a year have incurred health care debt in the past five years, the KFF poll found.
Women are more likely than men to be in debt. And parents more commonly have health care debt than people without children.
But the crisis has landed hardest on the poorest and uninsured.
Debt is most widespread in the South, an analysis of credit records by the Urban Institute shows. Insurance protections there are weaker, many of the states haven’t expanded Medicaid, and chronic illness is more widespread.
Nationwide, according to the poll, Black adults are 50% more likely and Hispanic adults 35% more likely than whites to owe money for care. (Hispanics can be of any race or combination of races.)
In some places, such as the nation’s capital, disparities are even larger, Urban Institute data shows: Medical debt in Washington, D.C.’s predominantly minority neighborhoods is nearly four times as common as in white neighborhoods.
In minority communities already struggling with fewer educational and economic opportunities, the debt can be crippling, said Joseph Leitmann-Santa Cruz, chief executive of Capital Area Asset Builders, a nonprofit that provides financial counseling to low-income Washington residents. “It’s like having another arm tied behind their backs,” he said.
Medical debt can also keep young people from building savings, finishing their education, or getting a job. One analysis of credit data found that debt from health care peaks for typical Americans in their late 20s and early 30s, then declines as they get older.
Cheyenne Dantona’s medical debt derailed her career before it began.
Dantona, 31, was diagnosed with blood cancer while in college. The cancer went into remission, but when Dantona changed health plans, she was hit with thousands of dollars of medical bills because one of her primary providers was out of network.
She enrolled in a medical credit card, only to get stuck paying even more in interest. Other bills went to collections, dragging down her credit score. Dantona still dreams of working with injured and orphaned wild animals, but she’s been forced to move back in with her mother outside Minneapolis.
“She’s been trapped,” said Dantona’s sister, Desiree. “Her life is on pause.”
The strongest predictor of medical debt
Desiree Dantona said the debt has also made her sister hesitant to seek care to ensure her cancer remains in remission.
Medical providers say this is one of the most pernicious effects of America’s debt crisis, keeping the sick away from care and piling toxic stress on patients when they are most vulnerable.
The financial strain can slow patients’ recovery and even increase their chances of death, cancer researchers have found.
Yet the link between sickness and debt is a defining feature of American health care, according to the Urban Institute, which analyzed credit records and other demographic data on poverty, race, and health status.
U.S. counties with the highest share of residents with multiple chronic conditions, such as diabetes and heart disease, also tend to have the most medical debt. That makes illness a stronger predictor of medical debt than either poverty or insurance.
In the 100 U.S. counties with the highest levels of chronic disease, nearly a quarter of adults have medical debt on their credit records, compared with fewer than 1 in 10 in the healthiest counties.
The problem is so pervasive that even many physicians and business leaders concede debt has become a black mark on American health care.
“There is no reason in this country that people should have medical debt that destroys them,” said George Halvorson, former chief executive of Kaiser Permanente, the nation’s largest integrated medical system and health plan. KP has a relatively generous financial assistance policy but does sometimes sue patients. (The health system is not affiliated with KHN.)
Halvorson cited the growth of high-deductible health insurance as a key driver of the debt crisis. “People are getting bankrupted when they get care,” he said, “even if they have insurance.”
What the federal government can do
The Affordable Care Act bolstered financial protections for millions of Americans, not only increasing health coverage but also setting insurance standards that were supposed to limit how much patients must pay out of their own pockets.
By some measures, the law worked, research shows. In California, there was an 11% decline in the monthly use of payday loans after the state expanded coverage through the law.
But the law’s caps on out-of-pocket costs have proven too high for most Americans. Federal regulations allow out-of-pocket maximums on individual plans up to $8,700.
Additionally, the law did not stop the growth of high-deductible plans, which have become standard over the past decade. That has forced growing numbers of Americans to pay thousands of dollars out of their own pockets before their coverage kicks in.
Last year the average annual deductible for a single worker with job-based coverage topped $1,400, almost four times what it was in 2006, according to an annual employer survey by KFF. Family deductibles can top $10,000.
While health plans are requiring patients to pay more, hospitals, drugmakers, and other medical providers are raising prices.
From 2012 to 2016, prices for medical care surged 16%, almost four times the rate of overall inflation, a report by the nonprofit Health Care Cost Institute found.
For many Americans, the combination of high prices and high out-of-pocket costs almost inevitably means debt. The KFF poll found that 6 in 10 working-age adults with coverage have gone into debt getting care in the past five years, a rate only slightly lower than the uninsured.
Even Medicare coverage can leave patients on the hook for thousands of dollars in charges for drugs and treatment, studies show.
About a third of seniors have owed money for care, the poll found. And 37% of these said they or someone in their household have been forced to cut spending on food, clothing, or other essentials because of what they owe; 12% said they’ve taken on extra work.
The growing toll of the debt has sparked new interest from elected officials, regulators, and industry leaders.
In March, following warnings from the Consumer Financial Protection Bureau, the major credit reporting companies said they would remove medical debts under $500 and those that had been repaid from consumer credit reports.
In April, the Biden administration announced a new CFPB crackdown on debt collectors and an initiative by the Department of Health and Human Services to gather more information on how hospitals provide financial aid.
The actions were applauded by patient advocates. However, the changes likely won’t address the root causes of this national crisis.
“The No. 1 reason, and the No. 2, 3, and 4 reasons, that people go into medical debt is they don’t have the money,” said Alan Cohen, a co-founder of insurer Centivo who has worked in health benefits for more than 30 years. “It’s not complicated.”
Buck, the father in Arizona who was denied care, has seen this firsthand while selling Medicare plans to seniors. “I’ve had old people crying on the phone with me,” he said. “It’s horrifying.”
Now 30, Buck faces his own struggles. He recovered from the intestinal infection, but after being forced to go to a hospital emergency room, he was hit with thousands of dollars in medical bills.
More piled on when Buck’s wife landed in an emergency room for ovarian cysts.
Today the Bucks, who have three children, estimate they owe more than $50,000, including medical bills they put on credit cards that they can’t pay off.
“We’ve all had to cut back on everything,” Buck said. The kids wear hand-me-downs. They scrimp on school supplies and rely on family for Christmas gifts. A dinner out for chili is an extravagance.
“It pains me when my kids ask to go somewhere, and I can’t,” Buck said. “I feel as if I’ve failed as a parent.”
The couple is preparing to file for bankruptcy.
About This Project
Diagnosis: Debt is a reporting partnership between KHN and NPR exploring the scale, impact, and causes of medical debt in America.
The series draws on the “KFF Health Care Debt Survey,” a poll designed and analyzed by public opinion researchers at KFF in collaboration with KHN journalists and editors. The survey was conducted Feb. 25 through March 20, 2022, online and via telephone, in English and Spanish, among a nationally representative sample of 2,375 U.S. adults, including 1,292 adults with current health care debt and 382 adults who had health care debt in the past five years. The margin of sampling error is plus or minus 3 percentage points for the full sample and 3 percentage points for those with current debt. For results based on subgroups, the margin of sampling error may be higher.
Additional research was conducted by the Urban Institute, which analyzed credit bureau and other demographic data on poverty, race, and health status to explore where medical debt is concentrated in the U.S. and what factors are associated with high debt levels.
The JPMorgan Chase Institute analyzed records from a sampling of Chase credit card holders to look at how customers’ balances may be affected by major medical expenses.
Reporters from KHN and NPR also conducted hundreds of interviews with patients across the country; spoke with physicians, health industry leaders, consumer advocates, debt lawyers, and researchers; and reviewed scores of studies and surveys about medical debt.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.