Trump faces criticism over lack of national plan on coronavirus

The Trump administration is facing intense criticism for the lack of a national plan to handle the coronavirus pandemic as some states begin to reopen.
Public health experts, business leaders and current administration officials say the scattershot approach puts states at risk and leaves the U.S. vulnerable to a potentially open-ended wave of infections this fall.
The White House has in recent days sought to cast itself as in control of the pandemic response, with President Trump touring a distribution center to tout the availability of personal protective equipment and press secretary Kayleigh McEnany detailing for the first time that the administration did have its own pandemic preparedness plan.
Still, the White House lacks a national testing strategy that experts say will be key to preventing future outbreaks and has largely left states to their own devices on how to loosen restrictions meant to slow the spread of the virus. Trump this week even suggested widespread testing may be “overrated” as he encouraged states to reopen businesses.
The Centers for Disease Control and Prevention (CDC) on Thursday night issued long-awaited guidance intended to aid restaurants, bars and workplaces as they allow employees and customers to return, but they appeared watered down compared to previously leaked versions.
Some experts said the lack of clear federal guidance on reopening could hamper the economic recovery.
“A necessary condition for a healthy economy is a healthy population. This kind of piecemeal reopening with everyone using different criteria for opening, we’re taking a big risk,” said Mark Zandi, chief economist at Moody’s Analytics.
The lack of coherent direction from the White House was driven home this week by damaging testimony by a former top U.S. vaccine official who claims he was ousted from his post improperly.
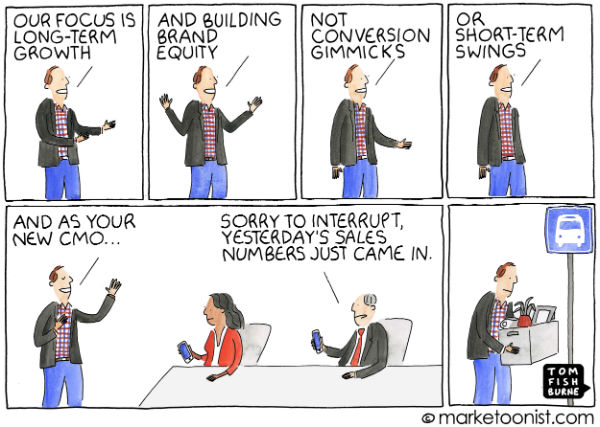
“We don’t have a single point of leadership right now for this response, and we don’t have a master plan for this response. So those two things are absolutely critical,” said Rick Bright, who led the Biomedical Advanced Research and Development Authority until he was demoted in late April.
The U.S. faces the “darkest winter in modern history” if it does not develop a more coordinated national response, Bright said. “Our window of opportunity is closing.”
From the start, the White House has let states chart their own responses to the pandemic.
The administration did not issue a nationwide stay-at-home order, resulting in a hodgepodge of state orders at different times, with varying levels of restrictions.
Facing a widespread shortage, states were left to procure their own personal protective equipment, ventilators and testing supplies. Trump resisted using federal authority to force companies to manufacture and sell equipment to the U.S. government.
Without clear federal guidance, state officials were competing against each other and the federal government, turning the medical supply chain into a free-for-all as they sought scarce and expensive supplies from private vendors on the commercial market.
“The fact that we had questions about our ability to have enough mechanical ventilators, and you had states basically bidding against each other, trying to secure personal protective equipment … it shouldn’t be happening during a pandemic,” said Amesh Adalja, a senior scholar at the Johns Hopkins University Center for Health Security.
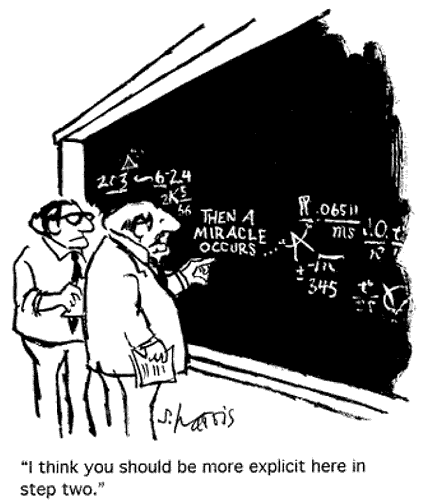
Internally, the administration struggled to mount a unified front as various agencies jockeyed for control. Multiple agencies have been providing contradictory instructions.
At first, Department of Health and Human Services (HHS) Secretary Alex Azar led the White House coronavirus task force.
Roughly a month, later he was replaced by Vice President Pence. The Federal Emergency Management Agency (FEMA) was later tasked with leading the response to get supplies to states, while senior White House adviser Jared Kushner led what has been dubbed a “shadow task force” to engage the private sector. Now, FEMA is reportedly winding down its role, and turning its mission back over to HHS.
The CDC has been largely absent throughout the pandemic. Director Robert Redfield has drawn the ire of President Trump as well as outside experts, and he has been seen infrequently at White House briefings.
“I think seeing the nation’s public health agency hobbled at a time like this and looking over its shoulder at its political bosses is something I hoped I would never see, and I’ve been working with the CDC for over 30 years,” said Lawrence Gostin, a professor of public health at Georgetown University.
“I think that people will die because the public health agency has lost its visibility and its credibility and that it’s being politically interfered with,” he added.
The administration recently has taken some steps to improve on the initial response to the pandemic.
Ventilator production has increased, and the U.S. is no longer seeing a shortage of the devices.
Testing has improved dramatically as well, though experts think the U.S. needs to be testing thousands of more people per day before the country can reopen.
The administration also unveiled plans to expand the Strategic National Stockpile’s supply of gowns, respirators, testing supplies and other equipment, after running out of supplies early in the pandemic.
Adalja said the administration’s positive steps are coming way too late.
“It’s May 15, we should have been in this position January 15,” he said.
McEnany on Friday for the first time detailed the White House’s preparedness plan that replaced the Obama-era pandemic playbook, an acknowledgement that Trump’s predecessor did leave a road map, despite claims to the contrary from some of the president’s allies.
She did not give many specifics on the previously unknown plan. Instead, McEnany declared the Trump administration’s handling of the virus had been “one of the best responses we’ve seen in our country’s history.”
Yet as states look to reopen businesses and get people back to work, the White House is taking a back seat as governors set their own guidelines for easing stay-at-home orders and restrictions on social activities.
The White House in April issued a three-step plan for states to reopen their economies, but it has largely been ignored by states and by the president.
Dozens of governors have begun easing restrictions on businesses and social activities without meeting the White House guidelines. Trump has been urging them to move even faster, backing anti-lockdown protesters in Michigan, Virginia, Minnesota and Pennsylvania.
Even scaled-down guidance from federal agencies is critical for providing a road map for state and local leaders, and for businesses considering how best to resume operations, said Neil Bradley, chief policy officer with the U.S. Chamber of Commerce.
“We need guidance because it helps instill confidence about the right types of approaches to take, but when you begin to move away from guidance and into either regulations or very strict approach, then that’s increasingly going to be unworkable in lots of different locations,” Bradley said.