As Steward Ship Was Sinking, CEO Bought $40M Yacht

A peculiar private equity deal screwed over an already struggling hospital system while reaping profits for executives, according to the Wall Street Journalopens in a new tab or window.
Back in 2020, Steward Health Care System needed $400 million to dig it “out of a deep financial hole.” Instead of investing in the struggling health system, Steward’s owner, Cerberus Capital Management, reportedly convinced Steward’s landlord, Medical Properties Trust (MPT), to provide the cash infusion.
Cerberus also sold its majority stake in Steward to a group that included the health system’s CEO Ralph de la Torre, MD, WSJ reported.
MPT had to put up millions of dollars for its tenant over a series of financial deals, and recent Congressional inquiries uncovered more details about how that went down. The first part of the cash infusion came in $205 million from MPT to invest in overseas hospitals in a joint venture with Steward. The second half was covered when MPT forgave the mortgage for a Steward hospital and paid $200 million for two Utah hospitals.
In the end, Cerberus ended up with a whopping $800 million in profit while Steward filed for Chapter 11 bankruptcy this week, WSJ reported.
Oh, and de la Torre bought a $40 million yacht with the proceeds of a 2021 payout related to his ownership of Steward.
Cartoon – Zero Premium Coverage
Hospice remains a blind spot for Medicare Advantage
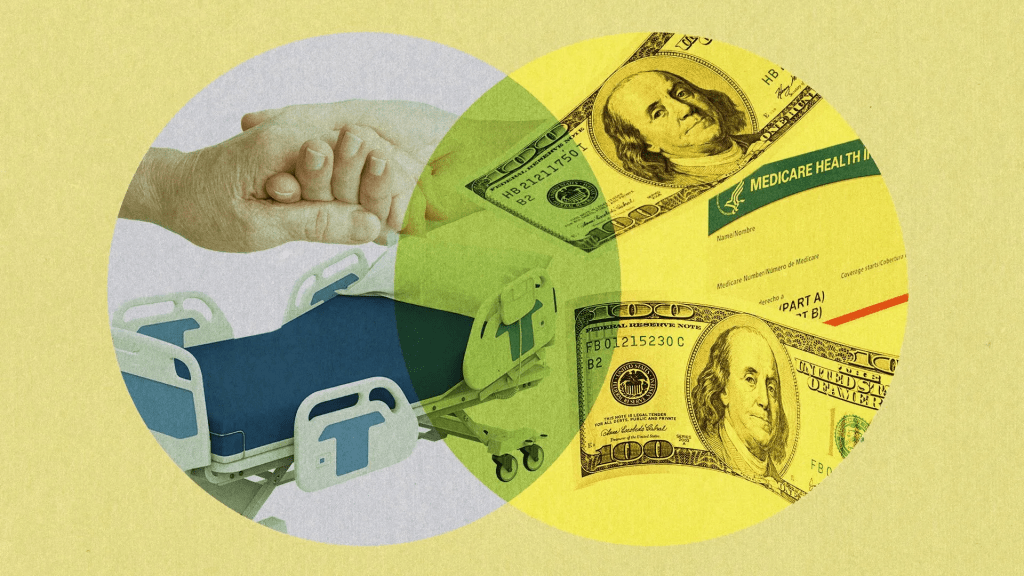
As Medicare Advantage grows bigger and bigger, there’s one area the industry and regulators haven’t figured out how to make work yet: hospice.
Why it matters:
The end-of-life care option is the only Medicare service that can’t be offered in the private-run alternative, which now covers over half of enrollees.
- Medicare is winding down an experiment — years earlier than expected — that let some Medicare Advantage plans offer a hospice benefit, citing operational challenges and limited interest from insurers and hospices.
Catch up quick:
Usually, when a Medicare Advantage beneficiary decides to enter hospice after receiving a terminal diagnosis, traditional Medicare pays for this care while they remain enrolled in their private plan.
- That could make navigating insurance “very, very clunky” for hospice patients, especially when they have health care needs unrelated to their terminal illness, said Lynne Sexten, CEO of Agrace Hospice.
- And this affects a lot of people. Nearly half of the 1.7 million Medicare Advantage beneficiaries who died in 2022 used hospice services, according to the Medicare Payment Advisory Commission (MedPAC).
- Experts say the roots of this awkward arrangement likely goes back about 40 years, when private Medicare first became a permanent offering. At the time, traditional Medicare had just started covering hospice, so officials had limited data on how much it cost.
What they did:
Medicare’s Innovation Center began an experiment in 2021 that allowed Medicare plans to contract directly with hospice providers.
- It aimed to test whether that could make end-of-life care transitions more seamless for Medicare Advantage patients while reducing costs and improving care quality.
- Participating health plans also covered palliative care and transitional care, where patients continued curative treatments like dialysis or chemotherapy temporarily during their hospice stay.
The Innovation Center announced abruptly in March that it would end the program in December, a year after officials said it would run through 2030.
- The news came after two major insurers — UnitedHealth Group and Elevance — pulled out of the model. Only 13 insurers participated this year.
- Hospices largely cheered the decision. Lower reimbursement rates, delayed payment from insurers and burdensome quality reporting made the experiment difficult for hospices that chose to contract with insurers, an independent evaluation of the program found.
- The Centers for Medicare and Medicaid Services stressed that its decision to end the experiment doesn’t mean it failed, and the agency in a statement to Axios said it will continue to evaluate results.
Many insurers also faced a learning curve on how to work with hospice for their Medicare enrollees. Hospice is delivered and paid for differently than other Medicare benefits.
- The experiment tried to do too much too fast, said Kevin Kappel, vice president at SCAN Health Plan, a nonprofit insurer that joined Medicare’s hospice experiment last year.
- “I think people underestimated how complex it was to do. … We’ve learned a lot,” Kappel said.
Yes, but:
Hospices and insurers said they still need to figure out how to make care more seamless for Medicare Advantage beneficiaries.
- “This is by no means the end of the story for end-of-life care providers and MA plans,” said Ethan McChesney, policy director at the National Partnership for Healthcare and Hospice Innovation.
- It’s been a full decade since MedPAC, the congressional advisory committee, recommended including hospice in Medicare Advantage, warning that excluding it “fragments care accountability and financial responsibility for MA enrollees who elect hospice.”
What we’re watching:
Industry leaders say hospice doesn’t necessarily have to become part of Medicare Advantage to improve care integration, or at least not right away.
- Ohio’s Hospice, a nonprofit provider that participated in the Medicare experiment, said it will continue working with Medicare plans to extend palliative care and symptom management to more patients, CEO Kent Anderson said.
- While Anderson said some peers worry about the growth of Medicare Advantage, “the longer we sit outside the managed care world, the less relevant we’ll become.”
Physician productivity up 4% as revenue, expenses rise

Expenses per provider remained considerably higher than revenue generated in the first quarter of 2024, although there are signs the gap could be closing, according to the Kaufman Hall “Physician Flash Report,” released May 2.
Kaufman Hall based their findings on a monthly report from Syntellis Performance Solutions, part of Strata. The report gathered data from more than 200,000 employed providers, including physicians and advanced practice providers.
Net patient revenue per provider full-time equivalent was $383,881 for the first quarter, up 4% from the same period last year. Total direct expenses per provider FTE hit $620,729 for the quarter. Expense growth has slowed over the last three years, with a 5% growth from 2022 to 2023 and just 3% growth from 2023 to 2024.
“Labor expenses are a growing proportion of total expenses, a trend that is unlikely to change significantly. Organizations should shift from optimizing downstream revenue to optimizing downstream margins,” the report authors advised, noting hospitals and physician organizations can evaluate provider specialties by outcomes or other metrics when they aren’t big revenue drivers.
Provider productivity was up 4% as measured by work relative value units. Physician wRVU per FTE was 5,979 for the first quarter, up 6% year over year. Physician compensation jumped 3% to $364,319, down from 6% growth between 2022 to 2023.
Labor expenses continue to rise while support staff decline across specialties. Labor was 84% of total expenses in the first quarter, and support staff per 10k provider wRVUs dropped 6% year over year to 3.14, even after an 8% drop from 2022 to 2023. Report authors recommended organizations find better ways to use APPs for higher physician productivity.
Here are specific data points from the first quarter report.
Median net patient revenue per provider FTE by specialty cohort were:
1. Primary care: $471,000
2. Medical specialty: $377,000
3. Surgical specialty: $393,000
4. Hospital-based specialty: $250,000
Median physician wRVU per physician FTE by specialty cohort was:
5. Primary care: 5,560
6. Medical specialty: 6,742
7. Surgical specialty: 6,626
8. Hospital-based specialty: 5,239
Median physician paid compensation per physician FTE by specialty cohort:
9. Primary care: $297,000
10. Medical specialty: $412,000
11. Surgical specialty: $480.000
12. Hospital-based specialty: $360,000
Median support staff FTEs per 10,000 wRFUs by specialty cohort:
13. Primary care: 4.48
14. Medical specialty: 2.47
15. Surgical specialty: 2.87
Medicare Advantage extras on the chopping block in 2025

Medicare Advantage insurers are planning to pare down their plan offerings in 2025.
Facing lower reimbursement rates from CMS and higher medical costs, many plan executives said they will prioritize margins over growing their membership numbers.
Brian Kane, CEO of Aetna, told investors May 1 that the company will prioritize “margins over membership” in 2025. The company will exit counties where it believes it can’t be profitable, Mr. Kane said.
“It’s hard to say right now that we won’t have a meaningful decrease in membership,” Mr. Kane said. “It’s certainly possible.”
Aetna’s competitors will be faced with the same choices, Mr. Kane said.
Humana executives also said the company is eyeing market exits in 2025. Susan Diamond, Humana’s CFO, said the company is expecting a net decline in its MA membership next year.
“Whether that is incrementally larger or smaller based on the other plans will be very dependent on what we see across the competitive landscape,” Ms. Diamond said April 24.
On first-quarter earnings calls, payer executives told investors they are disappointed in CMS’ 2025 rate notice. The notice will decrease benchmark payments, which insurers say amounts to a cut in funding for the program.
Medical costs are also on the rise in Medicare Advantage. CVS Health told its investors that Medicare Advantage costs keep climbing, partly driven by seasonal inpatient admissions. Outpatient services, including mental health and pharmacy, and dental spending also increased costs, CVS said.
In its final rate notice published April 1, CMS said it was aware Medicare Advantage organizations were reporting rising costs but was “not aware of all of the specific drivers accounting for the experience of these MA organizations. We have reviewed incomplete fourth quarter 2023 Medicare FFS incurred experience and it is consistent with our projections.”
Payers have also said they will cut back on supplemental benefits to account for lower rates.
CVS Health CEO Karen Lynch said it wil adjust plan-level benefits in 2025. The company led the industry in growth in 2024 but was a “notable outlier” compared to its peers in adding on supplemental benefits to entice members, The Wall Street Journal reported May 1.
Some Aetna plans offer a fitness reimbursement, according to The Wall Street Journal. Members could cash in the benefit for pickleball paddles, golf clubs and other sports equipment — but these extras could be a thing of the past in a tougher rate environment.
While every payer criticized CMS’s proposed rates, some executives said they would hold off on discussing their specific strategy until final bids are due. Insurers must send their MA plan proposals for 2025 to CMS by early June.
“It’s too early to provide specifics for the 2025 bid at this stage,” Elevance Health CEO Gail Boudreaux told investors. “I’m going to repeat, we’re looking to really balance growth and margins.”
30 health systems with strong finances

Here are 30 health systems with strong operational metrics and solid financial positions, according to reports from credit rating agencies Fitch Ratings and Moody’s Investors Service released in 2024.
Avera Health has an “AA-” rating and a stable outlook with Fitch. The rating reflects the Sioux Falls, S.D.-based system’s strong operating risk and financial profile assessments, and significant size and scale, Fitch said.
Cedars-Sinai Health System has an “AA-” rating and a stable outlook with Fitch. The rating reflects the Los Angeles-based system’s consistent historical profitability and its strong liquidity metrics, historically supported by significant philanthropy, Fitch said.
Children’s Health has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the Dallas-based system’s continued strong performance from a focus on high margin and tertiary services, as well as a distinctly leading market share, Moody’s said.
Children’s Hospital Medical Center of Akron (Ohio) has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the system’s large primary care physician network, long-term collaborations with regional hospitals and leading market position as its market’s only dedicated pediatric provider, Moody’s said.
Children’s Hospital of Orange County has an “AA-” rating and a stable outlook with Fitch. The rating reflects the Orange, Calif.-based system’s position as the leading provider for pediatric acute care services in Orange County, a position solidified through its adult hospital and regional partnerships, ambulatory presence and pediatric trauma status, Fitch said.
Children’s Minnesota has an “AA” rating and stable outlook with Fitch. The rating reflects the Minneapolis-based system’s strong balance sheet, robust liquidity position and dominant pediatric market position, Fitch said.
Cincinnati Children’s Hospital Medical Center has an “Aa2” rating and stable outlook with Moody’s. The rating is supported by its national and international reputation in clinical services and research, Moody’s said.
Cook Children’s Medical Center has an “Aa2” rating and stable outlook with Moody’s. The ratings agency said the Fort Worth Texas-based system will benefit from revenue diversification through its sizable health plan, large physician group, and an expanding North Texas footprint.
El Camino Health has an “AA” rating and a stable outlook with Fitch. The rating reflects the Mountain View, Calif.-based system’s strong operating profile assessment with a history of generating double-digit operating EBITDA margins anchored by a service area that features strong demographics as well as a healthy payer mix, Fitch said.
Hoag Memorial Hospital Presbyterian has an “AA” rating and stable outlook with Fitch. The Newport Beach, Calif.-based system’s rating is supported by its strong operating risk assessment, leading market position in its immediate service area and strong financial profile,” Fitch said.
Inspira Health has an “AA-” rating and stable outlook with Fitch. The rating reflects Fitch’s expectation that the Mullica Hill, N.J.-based system will return to strong operating cash flows following the operating challenges of 2022 and 2023, as well as the successful integration of Inspira Medical Center of Mannington (formerly Salem Medical Center).
JPS Health Network has an “AA” rating and stable outlook with Fitch. The rating reflects the Fort Worth, Texas-based system’s sound historical and forecast operating margins, the ratings agency said.
Mass General Brigham has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the Somerville, Mass.-based system’s strong reputation for clinical services and research at its namesake academic medical center flagships that drive excellent patient demand and help it maintain a strong market position, Moody’s said.
McLaren Health Care has an “AA-” rating and stable outlook with Fitch. The rating reflects the Grand Blanc, Mich.-based system’s leading market position over a broad service area covering much of Michigan, the ratings agency said.
Med Center Health has an “AA-” rating and stable outlook with Fitch. The rating reflects the Bowling Green, Ky.-based system’s strong operating risk assessment and leading market position in a primary service area with favorable population growth, Fitch said.
Nicklaus Children’s Hospital has an “AA-” rating and stable outlook with Fitch. The rating is supported by the Miami-based system’s position as the “premier pediatric hospital in South Florida with a leading and growing market share,” Fitch said.
Novant Health has an “AA-” rating and stable outlook with Fitch. The ratings agency said the Winston-Salem, N.C.-based system’s recent acquisition of three South Carolina hospitals from Dallas-based Tenet Healthcare will be accretive to its operating performance as the hospitals are highly profited and located in areas with growing populations and good income levels.
Oregon Health & Science University has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the Portland-based system’s top-class academic, research and clinical capabilities, Moody’s said.
Orlando (Fla.) Health has an “AA-” rating and stable outlook with Fitch. The rating reflects the health system’s strong and consistent operating performance and a growing presence in a demographically favorable market, Fitch said.
Presbyterian Healthcare Services has an “AA” rating and stable outlook with Fitch. The Albuquerque, N.M.-based system’s rating is driven by a strong financial profile combined with a leading market position with broad coverage in both acute care services and health plan operations, Fitch said.
Rush University System for Health has an “AA-” rating and stable outlook with Fitch. The rating reflects the Chicago-based system’s strong financial profile and an expectation that operating margins will rebound despite ongoing macro labor pressures, the rating agency said.
Saint Francis Healthcare System has an “AA” rating and stable outlook with Fitch. The rating reflects the Cape Girardeau, Mo.-based system’s strong financial profile, characterized by robust liquidity metrics, Fitch said.
Saint Luke’s Health System has an “Aa2” rating and stable outlook with Moody’s. The Kansas City, Mo.-based system’s rating was upgraded from “A1” after its merger with St. Louis-based BJC HealthCare was completed in January.
Salem (Ore.) Health has an”AA-” rating and stable outlook with Fitch. The rating reflects the system’s dominant marketing positive in a stable service area with good population growth and demand for acute care services, Fitch said.
Seattle Children’s Hospital has an “AA” rating and a stable outlook with Fitch. The rating reflects the system’s strong market position as the only children’s hospital in Seattle and provider of pediatric care to an area that covers four states, Fitch said.
SSM Health has an “AA-” rating and stable outlook with Fitch. The St. Louis-based system’s rating is supported by a strong financial profile, multistate presence and scale with good revenue diversity, Fitch said.
St. Elizabeth Medical Center has an “AA” rating and stable outlook with Fitch. The rating reflects the Edgewood, Ky.-based system’s strong liquidity, leading market position and strong financial management, Fitch said.
Stanford Health Care has an “Aa3” rating and positive outlook with Moody’s. The rating reflects the Palo Alto, Calif.-based system’s clinical prominence, patient demand and its location in an affluent and well insured market, Moody’s said.
University of Colorado Health has an “AA” rating and stable outlook with Fitch. The Aurora-based system’s rating reflects a strong financial profile benefiting from a track record of robust operating margins and the system’s growing share of a growth market anchored by its position as the only academic medical center in the state, Fitch said.
Willis-Knighton Medical Center has an “AA-” rating and positive outlook with Fitch. The outlook reflects the Shreveport, La.-based system’s improving operating performance relative to the past two fiscal years combined with Fitch’s expectation for continued improvement in 2024 and beyond.
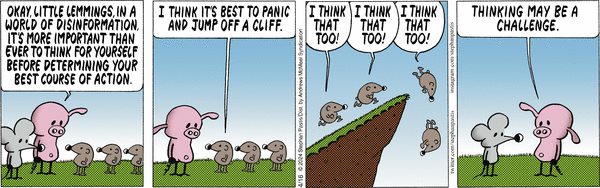
Cartoon – In a World of Disinformation
Cartoon – More Important Ever to Think
Wall Street Yawned as Congress Grilled UnitedHealth’s CEO but Went Ballistic on CVS/Aetna Over Medicare Advantage Claims

After UnitedHealth Group CEO Andrew Witty’s appearances at two congressional committee hearings last week, I had planned to write a story about what the lawmakers had to say. One idea I considered was to publish a compilation of some of the best zingers, and there were plenty, from Democrats and Republicans alike.
I reconsidered that idea because I know from the nearly half-century I have spent on or around Capitol Hill in one capacity or another that those zingers were carefully crafted by staffers who know how to write talking points to make them irresistible to the media. As a young Washington correspondent in the mid-to-late’70s, I included countless talking points in the stories I wrote for Scripps-Howard newspapers. After that, I wrote talking points for a gubernatorial candidate in Tennessee. I would go from there to write scads of them for CEOs and lobbyists to use with politicians and reporters during my 20 years in the health insurance business.
I know the game. And I know that despite all the arrows 40 members of Congress on both sides of the Hill shot at Witty last Wednesday, little if anything that could significantly change how UnitedHealth and the other big insurers do business will be enacted this year.
Some reforms that would force their pharmacy benefit managers to be more “transparent” and that would ban some of the many fees they charge might wind up in a funding bill in the coming months, but you can be sure Big Insurance will spend millions of your premium dollars to keep anything from passing that might shrink profit margins even slightly.
Money in politics is the elephant in any Congressional hearing room or executive branch office you might find yourself in (and it’s why I coauthored Nation on the Take with Nick Penniman).
You will hear plenty of sound and fury in those rooms but don’t hold your breath waiting for relief from ever-increasing premiums and out-of-pocket requirements and the many other barriers Big Insurance has erected to keep you from getting the care you need.
It is those same barriers doctors and nurses cite when they acknowledge the “moral injury” they incur trying to care for their patients under the tightening constraints imposed on them by profit-obsessed insurers, investors and giant hospital-based systems.
Funny not funny
Cartoonist Stephan Pastis captured the consequences of the corporate takeover of our government, accelerated by the Supreme Court’s 2010 landmark Citizens United vs. Federal Election Commission ruling, in his Pearls Before Swine cartoon strip Sunday.

Rat: Where are you going, Pig?
Pig: To a politician’s rally. I’m taking my magic translation box.
Rat: He doesn’t speak English?
Pig: He speaks politicianish. This translates it into the truth. Come see.
Politician: In conclusion, if you send me to Washington, I’ll clean up this corrupt system and fight for you everyday hard-working Americans. God bless you. God bless the troops. And God bless America.
Magic translation box: I am given millions of dollars by the rich and the powerful to keep this rigged system exactly as it is. Until you change that, none of this will ever change and we’ll keep hoping you’re too distracted to notice.
Politician’s campaign goon: We’re gonna need a word with you.
Magic translation box: This is too much truth for one comic strip. Prepare to be disappeared.
Rat: I don’t know him.
Back to Sir Witty’s time on the hot seat. It attracted a fair amount of media coverage, chock full of politicians’ talking points, including in The New York Times and The Washington Post. (You can read this short Reuters story for free.) Witty, of course, came equipped with his own talking points, and he followed his PR and legal teams’ counsel: to be contrite at every opportunity; to extol the supposed benefits of bigness in health care (UnitedHealth being by far the world’s largest health care corporation) all the while stressing that his company is not really all that big because it doesn’t, you know, own hospitals and pharmaceutical companies [yet]; and to assure us all that the fixes to its hacked claims-handling subsidiary Change Healthcare are all but in.
Congress? Meh. Paying for care? WTF!
Wall Street was relieved and impressed that Witty acquitted himself so well. Investors shrugged off the many barbs aimed at him and his vast international empire. By the end of the day Wednesday, the company’s stock price had actually inched up a few cents, to $484.11. A modest 2.7 million shares of UnitedHealth’s stock were traded that day, considerably fewer than usual.
Instead of punishing UnitedHealth, investors inflicted massive pain on its chief rival, CVS, which owns Aetna. On the same day Witty went to Washington, CVS had to disclose that it missed Wall Street financial analyst’s earnings-per-share expectations for the first quarter of 2024 by several cents. Shareholders’ furor sent CVS’ stock price tumbling from $67.71 to a 15-year low of $54 at one point Wednesday before settling at $56.31 by the time the New York Stock Exchange closed. An astonishing 65.7 million shares of CVS stock were traded that day.
The company’s sin: paying too many claims for seniors and disabled people enrolled in its Medicare Advantage plans. CVS’s stock price continued to slide throughout the week, ending at $55.90 on Friday afternoon. UnitedHealth’s stock price kept going up, closing at $492.45 on Friday. CVS gained a bit on Monday, closing at $55.97. UnitedHealth was up to $494.38.
Postscript: I do want to bring to your attention one exchange between Witty and Rep. Buddy Carter (R-Ga.) during the House Energy and Commerce committee hearing. Carter is a pharmacist who has seen firsthand how UnitedHealth’s virtual integration–operating health insurance companies with one hand and racking up physician practices and clinics with the other–and its PBM’s business practices have contributed to the closure of hundreds of independent pharmacies in recent years. He’s also seen patients walk away from the pharmacy counter without their medications because of PBMs’ out-of-pocket demands (often hundreds and thousands of dollars). And he’s seen other patients face life-threatenng delays because of industry prior authorization requirements. Carter was instrumental in persuading the Federal Trade Commission to investigate PBMs’ ownership and business practices. He told Witty:
I’m going to continue to bust this up…This vertical integration in health care in general has got to end.
More power to you, Mr. Carter.