The Memo: Scale of economic crisis sends shudders through nation

New data released Thursday revealed the scale of the economic devastation wrought by the coronavirus crisis — and experts say there is no end in sight.
More than 6.6 million new unemployment claims were filed during the week ending March 28, according to the Department of Labor. The figure was double that of the previous week, which had itself been by far the highest since records began.
The stark reality is that roughly 10 million people have been dumped from their jobs in two weeks. A previously robust economy has been scythed down by the virus. A nation that had been enjoying its lowest unemployment rate for decades is now virtually certain to see jobless totals surpass those of the Great Recession a decade ago.
“The present economic situation is awful,” said Jason Furman, a Harvard University professor who served as chairman of President Obama’s Council of Economic Advisers. “The data is just telling us what we can see with our own eyes — there is very little business happening.”
Economists who had already been deeply worried about the immediate outlook are now wondering if their earlier projections were in fact too rosy.
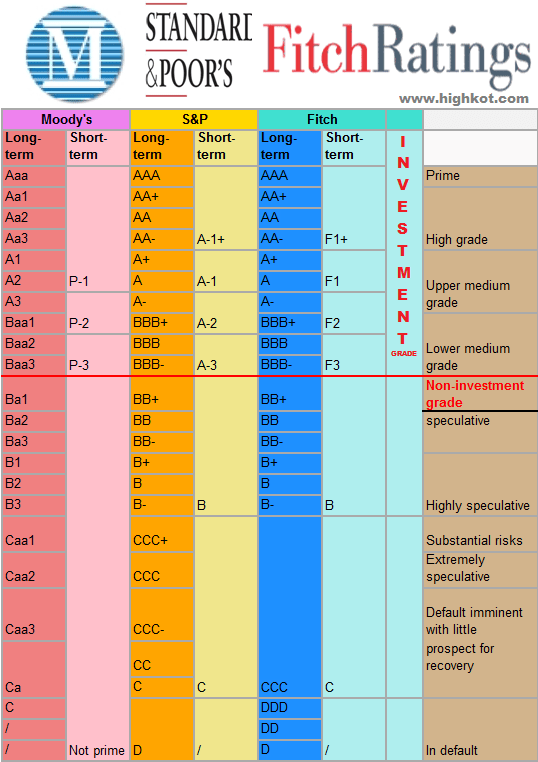
“In our earlier scenario, we had expected 6.5 million job losses by May,” said Beth Ann Bovino, the chief U.S. economist at Standard & Poor’s. That figure will be exceeded, she now believes, given that there were “more lockdowns, more business closures and more businesses just trying to keep themselves alive” by laying off workers.
Heidi Shierholz, senior economist and director of policy at the Economic Policy Institute, said that even the 10 million figure for new unemployment claims was “likely a massive undercount” of actual losses because, during that period, self-employed people and workers in the so-called “gig economy” were generally not eligible to apply. This is changing as a consequence of the package recently passed by Congress that extends eligibility for unemployment benefits, as well as providing other aid for businesses and individuals.
“Our estimate is that by the end of June, 20 million people will have lost their jobs — and I am wondering if even that is optimistic,” Shierholz said.
The political ramifications of such a huge economic shock are unknowable.
President Trump had been looking forward to using the economy as his strongest card as he seeks a second term in November. That card has been shredded.
Trump has promised repeatedly during his White House briefings on the crisis that the nation can bounce back very fast once the public health dangers have receded.
Trump’s approval ratings have also ticked up modestly since the crisis began in many polls. He may be benefitting from the traditional “rallying around the flag” effect that has occurred in previous moments of crisis.
President George W. Bush, for example, hit 90 percent approval in a Gallup poll — the highest result for any president in the polling organization’s history — right after the terrorist attacks of Sept. 11, 2001.
In a statement on Thursday, probable Democratic nominee Joe Biden hit Trump for “failing to prepare our nation” for the ramifications of the coronavirus crisis. Biden called on Trump to allow open enrollment in the Affordable Care Act and also jabbed at Treasury Secretary Steven Mnuchin for having referred to previous unemployment figures as “not relevant.”
In response, Trump campaign communications director Tim Murtaugh blasted back at Biden for “ineffectively sniping from the sidelines, stumbling through television interviews, and hoping for relevance and political gain.”
Economic experts caution that Trump’s promises of a v-shaped recovery, in which the nation jolts itself back into strong economic shape quickly, are almost certainly unrealistic. It will not be a matter of the nation simply rolling the shutters back up and returning to business as usual.
“The economy is not symmetrical,” said Furman. “It is easier to separate someone from a job than to connect someone to a job. In recessions, the unemployment rate can go up very quickly and it comes down very slowly. The worry is that this will be like that.”
Several economic experts who spoke with The Hill made similar points, unprompted, as to the ways the federal government could ease the crisis.
One refrain was that huge assistance needs to be made available to states. States are generally required to balance their budgets. In a situation like the current one, where their tax revenue is cratering, this means they are obligated to severely cut spending — something that most economists believe would deepen and prolong the recession.
Another theme was the need to tie together financial assistance for businesses and the retention of employees.
The recently passed stimulus package makes some effort to do that, particularly in the case of small businesses. The Paycheck Protection Program extends loans to small businesses based upon eight weeks of payroll costs plus an additional 25 percent of the total.
The payroll portion of the loans would be forgiven — rendering them in effect a grant, not a loan — so long as the workforce was maintained at existing levels.
Economic experts praise the principle but worry that the total amount of money in the pot for these loans — $349 billion — may not be enough.
“The small business subsidies will be critical,” said Steven Hamilton, an assistant professor of economics at The George Washington University. “The government needs to get the word out on those, and Congress will likely need to pass an expansion both to adequately fund the existing scheme and to make the scheme more generous to businesses to keep them from laying off workers.”
The public seems to share the view that the aid package, which also includes checks of up to $1,200 for individuals, is a move in the right direction — but unlikely to suffice.
A CBS News poll released late Thursday afternoon indicated 81 percent of Americans support the recent legislation but 57 percent also say it likely won’t be enough.
The same trepidation is shared by the experts, given the unprecedented nature of the coronavirus and the economic crisis it has created.
“It’s like nothing we have ever seen before,” said Shierholz.