Health insurers and their lobbying arms have spent $476.5 million since 2020 to block reform, protect profits, and mislead the public — and it’s coming straight from our premiums and tax dollars.
AHIP, the big PR and lobbying outfit for most health insurers, undoubtedly believes the praise it got from Trump administration officials and some members of Congress this week – when it announced changes insurers presumably will make voluntarily to alleviate the burden of prior authorization demands on patients and health care providers – has taken the heat off insurers. AHIP’s message to Washington politicos: You don’t need to pass any new laws to make us do the right thing. You can trust us, despite our decades of engaging in untrustworthy behavior to maximize profits.
As former health insurance executive Seth Glickman, M.D., explained yesterday, nobody should believe this hen-house guarding fox.
After all, AHIP is nothing more than a PR and lobbying shop with millions of our dollars to play with. It has zero ability to force insurers to do what AHIP claims they will do. I know this because I worked closely with AHIP during my 20 years in the industry and represented Cigna on its strategic communications committee.
From Fox to “Fixer”?
AHIP pulled off its big show on Monday – and got plenty of generally fawning press coverage – because of all the money it and affiliated insurers throw around Washington every year to protect what has become an incredibly profitable status quo.
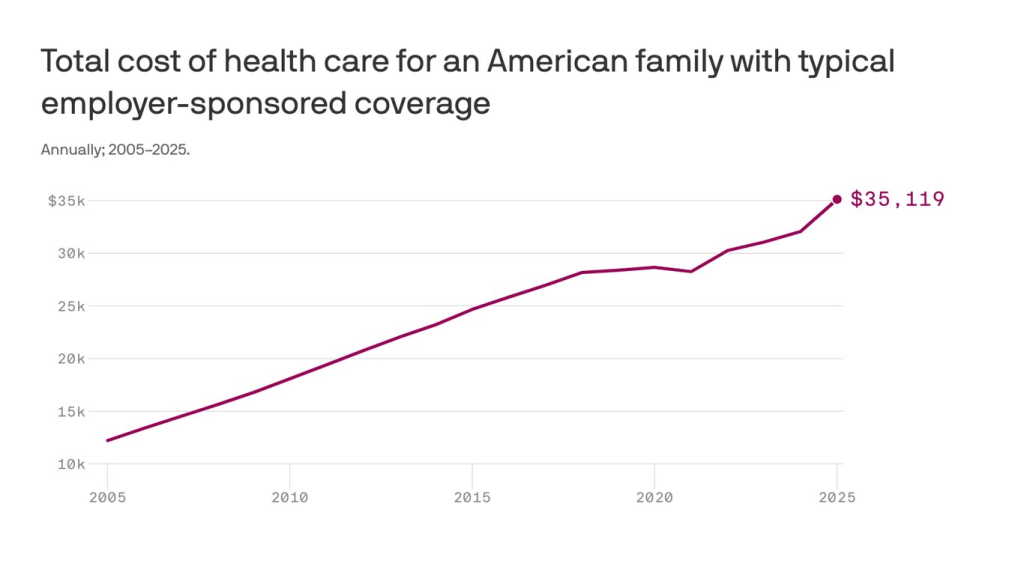
Collectively, the seven biggest for-profit insurers reported $70 billion in profits last year.
(Beleauered UnitedHealth alone reported $34.4 million in operating earnings.) And that’s just seven among dozens. One way they make that kind of dough, for their shareholders and top executives, is by using prior authorization to avoid paying for patients’ medically necessary care. Many people die as a result, while investors get richer. It’s that simple and that cold.
So just how much money does AHIP and the insurance industry spend to bamboozle members of Congress and the White House every year? We’re talking stupid money. And orders of magnitude more than nonprofits that advocate for reforms that would benefit patients instead of shareholders.
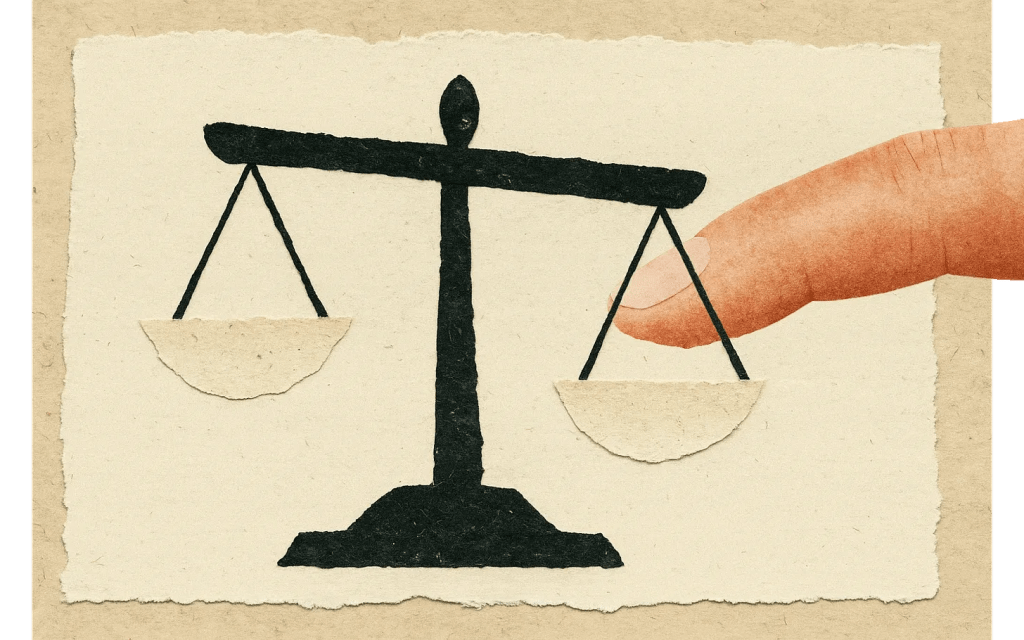
Nearly Half a Billion Ways They Tip the Scale
To find out just how much, I turned to OpenSecrets and did some math. OpenSecrets, as a reminder, is the well-named organization that keeps tabs on campaign contributions and lobbying expenses.
What I discovered is that AHIP has spent almost $65 million lobbying Congress and the Biden and Trump administrations since 2020. Its cousin, the Blue Cross Blue Shield Association, has spent even more. More than twice as much more.
And that, folks, is just the tip of the iceberg, and it doesn’t even include the tens of millions the industry spends on massive advertising campaigns inside the DC beltway that it’s not required to report. Or the dark money ads and advocacy the industry bankrolls.
But just the lobbying totals are mind-blowing. When you factor in the money spent by the big seven insurers and the other PR and lobbying groups that insurers funnel money to, the total grows to almost $500 million. You read that right: nearly half a billion dollars.
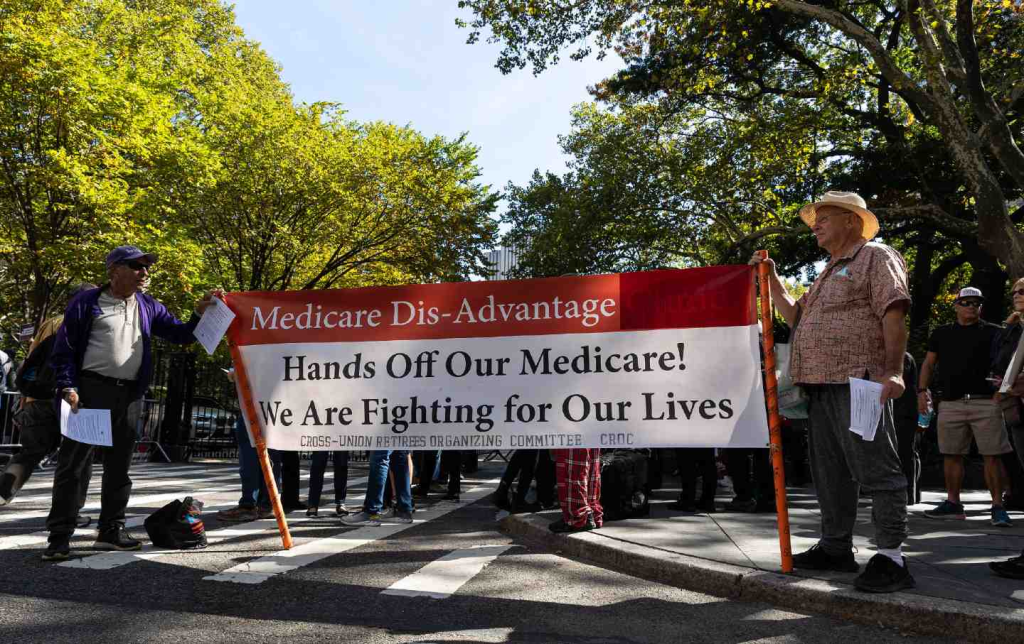
Most of that spending was during the Biden administration, but the industry is on track to break spending records during the first year of the current Trump administration. They are lobbying not only to beat back new laws and regulations that could constrain their prior authorization practices but also to protect their biggest cash cows: Medicare Advantage and their pharmacy benefit managers (PBMs).
Three PBMs – owned by Cigna, CVS/Aetna and UnitedHealth –control 80% of the pharmacy benefit market and determine which drugs we’ll have access to and how much we have to pay out of pocket even with insurance.
The Big Number
$476.5 million – That’s the amount of money health insurance corporations and four of their PR and lobbying groups – AHIP, BCBSA (which includes contributions from Elevance/Anthem as well as numerous other BCBS companies), the Pharmaceutical Care Management Association and the Better Medicare Alliance – have collectively spent on lobbying Congress and federal regulators between January 1, 2020, and March 31, 2025.
The Breakdown

Keep in mind that that money is not coming out of executives’ paychecks. It’s coming out of our pockets. Insurers skim money from our premiums and taxes to finance their propaganda and lobbying efforts to keep the gravy train rolling. And it’s in addition to all the campaign cash they dole out every year, which I tabulated recently.
This is not to say that reform is impossible. Scrappy advocacy groups with a tiny fraction of that total have scored important victories over the years. But it is why progress is so slow and setbacks are so frequent.
But just imagine how all that money could be put to better use to ensure that all Americans, including those with insurance, are able to get the care they need when they need it. It’s clear that in addition to reforming our health care system, we need political reforms that make it more difficult for big corporations and their trade groups to influence elections and public policy.