https://www.politico.com/news/2020/06/15/nursing-homes-coronavirus-321220

About half of all facilities have yet to be inspected for procedures to stop the spread of coronavirus.
Thousands of nursing homes across the country have not been checked to see if staff are following proper procedures to prevent coronavirus transmission, a form of community spread that is responsible for more than a quarter of the nation’s Covid-19 fatalities.
Only a little more than half of the nation’s nursing homes had received inspections, according to data released earlier this month, which prompted a fresh mandate from Medicare and Medicaid chief Seema Verma that states complete the checks by July 31 or risk losing federal recovery funds.
A POLITICO survey of state officials, however, suggests that the lack of oversight of nursing homes has many roots. Many states that were hit hard by the virus say they chose to provide protective gear to frontline health workers rather than inspectors, delaying in-person checks for weeks if not months. Some states chose to assess facilities remotely, conducting interviews over the phone and analyzing documentation, a process many experts consider inadequate.
In places where state officials claimed that in-person inspections have taken place, the reports found no issues in the overwhelming majority of cases, even as Covid-19 claimed more than 31,000 deaths in nursing homes. Less than 3 percent of the more than 5,700 inspection surveys the federal government released this month had any infection control deficiencies, according to a report on Thursday by the Center for Medicare Advocacy, a nonprofit patient activist group.
“It is not possible or believable that the infection control surveys accurately portray the extent of infection control deficiencies in U.S. nursing facilities,” the report states.
Noting the vast and unprecedented danger that the coronavirus presents to the elderly and people with disabilities, patient advocates described the lack of inspections as a shocking oversight.
“If you’re not going in, you’re essentially taking the providers’ word that they’re doing a good job,” said Richard Mollot, the executive director of the Long Term Care Community Coalition.
In March, the Trump administration paused routine nursing home inspections, which typically occur about once a year. Instead, the Centers for Medicare and Medicaid Services asked that state agencies focus on inspecting facilities for their infection control practices, such as whether staff wash their hands or properly wear protective clothing before tending to multiple patients.
But for more than two months, state inspectors failed to enter half the country’s homes — a revelation that prompted CMS to crack down.
“We are saying you need to be doing more inspections,” Verma told reporters, explaining her message to states. “We called on states in early March to go into every single nursing home and to do a focused inspection around infection control.”
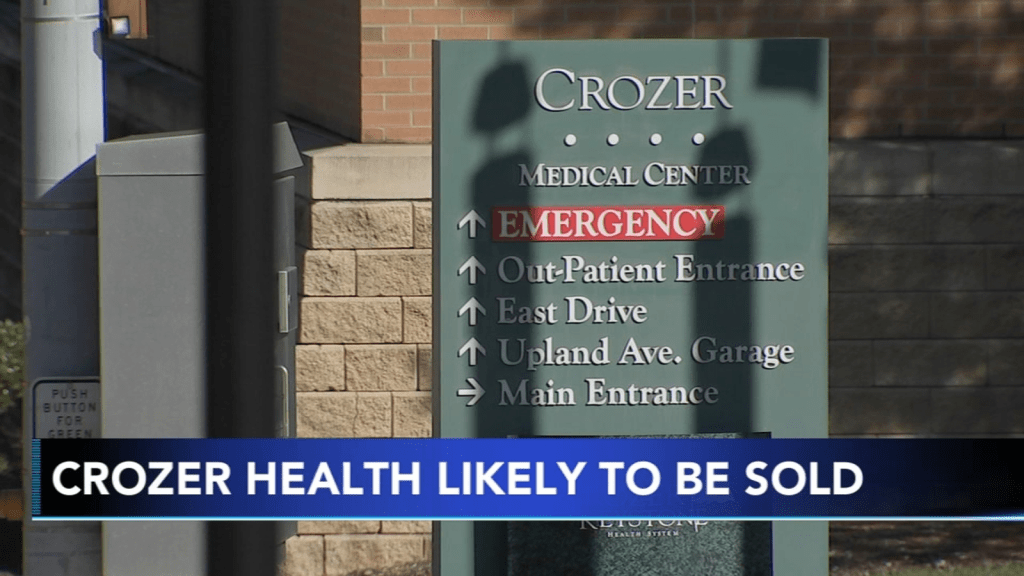
In some hard-hit states, inspectors conducted remote surveys rather than going into nursing homes, a process that involved speaking to staff by phone and reviewing records. In Pennsylvania, for example, inspectors conducted interviews and reviewed documents for 657 facilities from March 13 to May 15 — most of which was done remotely.
But critics say the failure to make in-person checks prevented states from identifying lapses at a crucial time. The fact that family members were blocked from visiting their relatives — a policy intended to prevent the virus from entering the facility — removed another source of accountability in homes, some of which ended up having more than half of their residents stricken with the coronavirus.
Keeping relatives out of nursing homes — a policy that continues — has made it more difficult to advocate on behalf of residents in the state, said Karen Buck, executive director of the Pennsylvania-based SeniorLAW Center. More than 4,000 residents of nursing homes and other personal care facilities have died of coronavirus in the Keystone State.
“The inspections are vital,” said Buck. “I think access to residents is essential, and we are very concerned that Pennsylvanians are behind where we should be. We recognize these are very difficult times for our leaders, but we can’t continue to wait.”
Pennsylvania officials maintained that the remote inspections were beneficial, and said they went into the facilities when they felt there was significant concern over residents’ health.
“We can conduct the same interviews, review the same documentation and do all the same actions we could in person, except for the ability to be on-site,” health department spokesperson Nate Wardle wrote in an email, adding that Verma’s office approved the remote procedures earlier this spring.
Nonetheless, many public health experts say they believe states have erred in choosing not to prioritize nursing home inspectors when handing out protective equipment. While it makes sense to direct resources to front-line workers, nursing home inspectors were only a tiny number of people compared to the hundreds of thousands of hospital employees — and experts contend that the situation in nursing facilities was dire enough to require immediate action.
David Grabowski, an expert in aging and long-term care at Harvard Medical School, said he understands inspectors were put in a tough position in the early days of the pandemic, but that inspections needed to be ramped up within a few weeks.
“I think after those first few weeks we should have had personal protective equipment in place for the inspectors and doing these inspections remotely is really second best,” he said.
And yet state after state waited on inspections or performed them remotely.
In Utah, only a small portion of the state’s nearly 100 facilities received inspections over the first three months of the pandemic. Only now is the state health department ramping up on-site inspections, with the goal of hitting all of its nursing homes by the second week of July. It conducted 14 last week, and received some help from federal inspectors with another four.
The state survey agency said it made a conscious determination not to request protective equipment for state inspectors in the initial phase of the pandemic, fearing they would take supplies away from frontline health providers, said Greg Bateman, the head of long-term care surveys. Instead, the department conducted 43 remote reviews and talked to nursing homes at least twice a week.
In Idaho, state inspectors have only recently received the N95 masks, face shields and gowns necessary to perform inspections.
“The reason we had difficulty is because Idaho, like many other states, was challenged to secure adequate PPE to meet the needs of the various health care entities,” health department spokesperson Niki Forbing-Orr wrote in an email. “The state surveyors had concerns about potentially using PPE that other entities could use that provide direct medical services and care to Idaho residents.”
In New Jersey, which has seen roughly 6,000 deaths in nursing homes and other communal settings, the health department also first chose sending supplies to frontline workers in nursing homes and hospitals. The state began making in-person checks when it received PPE April 16, said Dawn Thomas, a New Jersey health department spokesperson.
But New Jersey still has a long way to go. The state has completed inspections in only about 115 out of more than 360 nursing homes as of June 3, according to Thomas.
While Pennsylvania, Idaho, New Jersey and other states complained of a lack of PPE, other states battling major outbreaks of coronavirus in nursing homes have completed nearly all of their inspections, calling into question the explanations for why others have struggled.
Washington state, where the Life Care Center of Kirkland became an early epicenter of the coronavirus outbreak, has completed 99 percent of its inspections, the state reported this spring to CMS. And Michigan, which has had nearly 2,000 deaths in nursing homes, has completed nearly 85 percent of its inspections.
By contrast, states such as West Virginia and Maryland, with only 11.4 and 16.4 percent of facilities inspected as of the end of May, lagged way behind.
A nursing home in Maryland’s Carroll County served as an early example of just how quickly the coronavirus can ravage nursing homes. On March 26, a resident at a Carroll County, Md., facility tested positive for the coronavirus. Two weeks later, the number of confirmed cases was up to 77 out of 95 residents, along with 24 staff members. At least 28 residents have died.
A Maryland health department spokesperson says the state took “early and aggressive measures” to address the virus in nursing homes, noting that Maryland created the country’s first strike teams — composed of state and local health officials, medical professionals and National Guard members — to help triage seniors and scrutinize facilities.
Nonetheless, state inspectors didn’t have personal protective equipment until late April, according to the health department.
“In April, PPE acquisition was challenging across the nation and in Maryland due to the rapidly evolving Covid-19 pandemic,” the spokesperson wrote in an email, adding that the department sought N95 masks, gowns and other items from “the national stockpile, FEMA and national and international supply chains.”
With many facilities still closed to visitors, the slow pace of inspections lost a key window into the nursing homes during the pandemic.
“I think having more eyes on what’s happening is really important,” Grabowski said.
Last month, the Health and Human Services’ watchdog agency announced plans to review the pace of inspections in nursing homes and barriers to completing them — referring to such checks as a “fundamental safeguard to ensure that nursing home residents are safe and receive high-quality care.”
“There is no substitute for boots on the ground — for going into a facility to assess whether a facility is abiding by long-standing infection control practices,” Verma told reporters this month.