https://www.buzzfeednews.com/article/zoetillman/trump-medicare-cuts-hospitals-coronavirus-lawsuits?mkt_tok=eyJpIjoiTVRRd00yUmpZbUV3TVRVeiIsInQiOiJTZ0piR2wyRnBZOU5jR3N2TTNzd3Vrb040dHA5K0hVT0lQRm82YnFkVlNVVko4QlVRU0Z0SVVTQWxZUXJmWTZFTVBqaVh0N1JRWHFJTmg2dkNDb0hQTjBYYmxyUnphMEVGSmhwN0NJWUE3V0FFa2FIenJRZTJjWmliSWZKRVwvcU8ifQ%253D%253D

The Trump administration has been fighting in court with public and nonprofit hospitals since 2017 over a plan to slash the reimbursement rates for drugs prescribed to Medicare patients.
In 2018, Park Ridge Health, a not-for-profit healthcare network in western North Carolina that serves a large population of lower-income patients, delayed plans to buy a new CT scanner for stroke patients.
The Trump administration had drastically scaled back a federal drug reimbursement program that benefitted public and not-for-profit hospitals. Park Ridge, now called AdventHealth Hendersonville, stood to lose $3.3 million per year, the hospital’s chief financial officer wrote in a court affidavit, and it wasn’t just the CT scanner on the line — that money went toward a variety of services for elderly and poor patients, including new cancer treatment facilities, women’s healthcare, and partnerships with nonprofits on issues like prescription drug abuse.
Park Ridge and other hospitals have been battling with the administration in court for three years over a plan to slash by nearly 30% the reimbursement rate that hospitals get for certain drugs prescribed to Medicare patients. The hospitals won the first round. The US Court of Appeals for the DC Circuit heard arguments in November and has yet to rule, and for now the cut is still in effect. In the meantime, the Centers for Medicare & Medicaid Services (CMS) is exploring another way to make the cut if they lose the case, over the objection of hospitals.
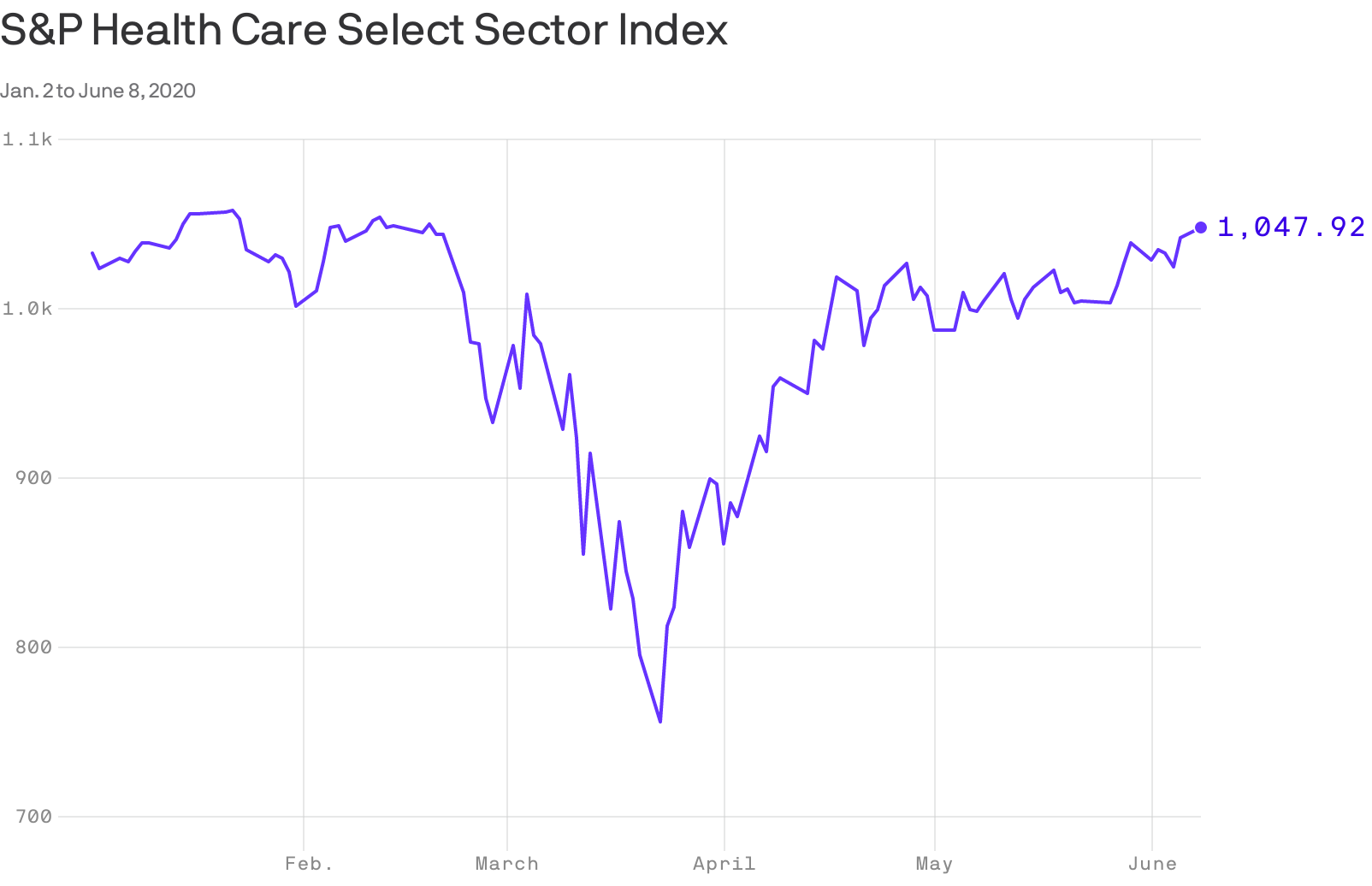
The litigation predates the coronavirus pandemic, but the stakes are higher as hospitals nationwide lose tens of billions of dollars weekly while nonessential services and elective surgeries are on hold because of the ongoing crisis.
“If [hospitals] lost that money now, it would make an already dire financial situation worse,” Lindsay Wiley, director of the Health Law and Policy Program at American University Washington College of Law, wrote in an email to BuzzFeed News.
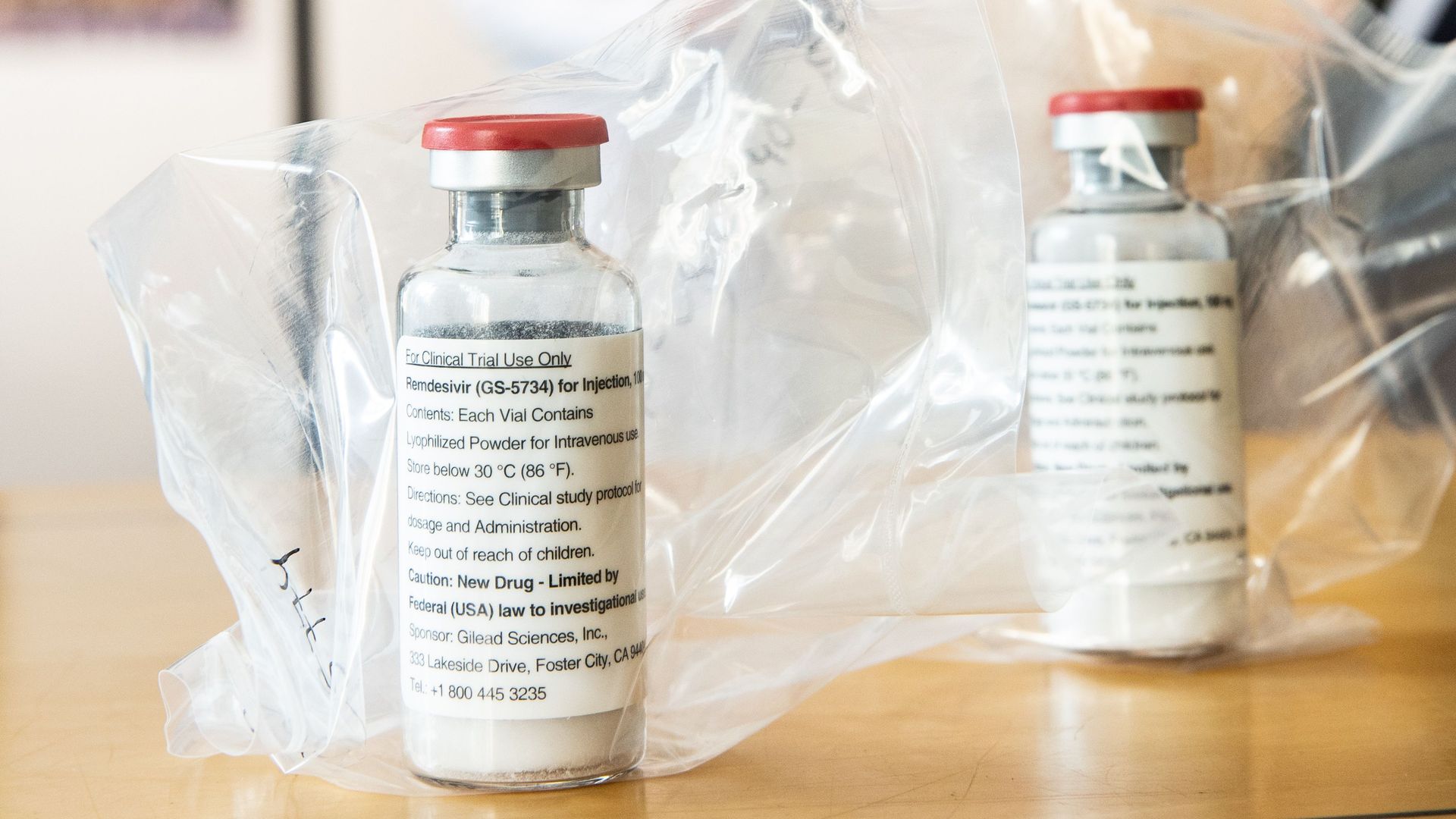
Hospitals that serve a high proportion of lower-income patients can buy outpatient drugs at a discounted price through what’s known as the 340B program. Until 2017, these hospitals were reimbursed by the federal government for drugs prescribed to Medicare patients at a higher rate than the discounted price the hospitals paid.
The CMS announced in 2017 that it was slashing the reimbursement rate from 6% above the average price of the drugs to 22.5% below the average cost. The agency said the program gave hospitals an incentive to overprescribe drugs and cost patients more money, and shouldn’t provide a windfall to subsidize other services.
Hospitals that opposed the change argued that they had put money earned through the program — which can run in the millions of dollars for a hospital each year — into services for poor and underserved communities, as Congress intended.
The CMS estimated that cutting the reimbursement rate for the drugs would reduce the amount of money paid to hospitals by $1.6 billion in 2018 alone. Scaling back that funding would actually increase the rates paid by the government for other services for Medicare patients — the payment system has to be “budget neutral” — but Park Ridge and other hospitals that took the administration to court said they still expected net losses of millions of dollars.
Many hospitals that participate in the 340B program “are in the red to begin with,” said Maureen Testoni, president and CEO of 340B Health, a membership group for hospitals and health systems that participate.
“So on top of that, you add this pandemic and all the financial turmoil that this has caused,” Testoni said. The pandemic has highlighted “how critical [hospitals] are … and what an important role they play. And, financially, they’re not in a situation where they can play that role when they have this big financial reduction.”
While waiting for the DC Circuit to rule, the CMS is exploring ways to move forward with the rate cut even if it loses. Last month, the agency launched a survey to collect data from 340B hospitals that the CMS says would address the issues that led the lower court judge to rule against the government. Hospitals opposed the survey and asked the agency to at least delay it, saying they’d have to divert resources that are already stretched thin during the pandemic to respond.
“Now is not the time to distract hospitals’ attention from the vital job at hand to complete a CMS survey on drug acquisition costs. By launching the survey with no notice on April 24 and providing less than three weeks to respond, CMS is creating an unnecessary burden on hospitals at the worst possible moment,” Testoni wrote in a May 4 letter to the agency. The agency didn’t respond.
Representatives of hospitals involved in the lawsuits declined interview requests, citing the pending litigation. The American Hospital Association, a lead plaintiff, declined an interview request but sent a statement:
“The COVID-19 pandemic has created the greatest financial crisis in history for America’s hospitals and health systems, with our field losing over $50 billion each month. While it is too soon to have precise data on the full impact of this pandemic, the unlawful Medicare cuts that we are contesting in federal court have added significantly to the financial pressure all hospitals face,” the group said.
A spokesperson for the Department of Health and Human Services did not return a request for comment. In court, the Justice Department has argued that the district court judge lacked authority to review the rate cut at all, and that even if he could, the government had the power to bring the rate in line with what the available data showed hospitals were paying for the drugs.
“[O]vercompensation for some drugs or treatments means reduced payments for other drugs and treatments, and correcting overcompensation permits more equitable distribution of limited funds,” Justice Department lawyers argued in the government’s brief to the DC Circuit. “The result of bringing the Medicare payment amount for 340B drugs into alignment with average acquisition cost was therefore the redistribution of the anticipated $1.6 billion in savings, resulting in a 3.2% increase in the Medicare payment rates for non-drug items and services.”
Congress created the 340B program in 1992. Healthcare providers eligible for the program can buy outpatient drugs at discounted rates from pharmaceutical companies. When hospitals prescribe those drugs to patients covered by Medicare — the federal insurance program for people who are over the age of 65 or have disabilities — they submit claims to the government for reimbursement.
Starting in 2006, Congress gave the CMS two options to set the drug reimbursement rate. It could rely on what hospitals were actually paying to buy drugs if it had “statistically sound survey data” or, if that wasn’t available, the average sales price of the drugs. If the agency used the second, alternative option, Congress set a default rate: the average sales price plus 6%.
In the summer of 2017, the Trump administration announced a plan to change the rate. Under the new rule, the Medicare agency said it would pay the average sales price of drugs minus 22.5%. That rate would come closer to matching the discounted rate hospitals were paying through the 340B program, the agency said.
Hospitals don’t have to track or disclose how they use money saved through the program. Kelly Cleary, who spent three years as the chief legal officer for the CMS, said hospitals had provided examples of how they were using the funds to expand services into underserved areas and provide free or low-cost care.
“The money was going toward a purpose that was consistent with their mission,” said Cleary, who was involved in the CMS’s effort to change the rate and defend it in court. She returned to private practice last month as a partner at the law firm Akin Gump Strauss Hauer & Feld.
The chief financial officer for the Henry Ford Health System, which serves patients in Detroit and Jackson, Michigan, wrote in a court affidavit that even if the cut meant that reimbursement rates increased for other Medicare services, the hospital network still expected to lose around $8.5 million by the end of 2018 — money that had gone toward services for patients with low incomes, such as free and low-cost medications, a free community clinic, and mobile health units.
The margin between what the Henry Ford Health System paid for drugs through the 340B program and what it received back from Medicare helped hospitals in that network provide care for “underserved and indigent populations … that would otherwise be financially unsustainable,” the officer wrote.
In support of the rate cut, the CMS pointed to a 2015 report by the Government Accountability Office that showed hospitals participating in the program had an incentive to prescribe more drugs than hospitals that weren’t in the program, and that meant higher copayments for Medicare patients who were prescribed more drugs or higher-priced drugs. The agency concluded hospitals were receiving too much of a net financial benefit.
“While we recognize the intent of the 340B Program,” the agency wrote in a November 2017 notice in the Federal Register, “we believe it is inappropriate for Medicare to subsidize other activities.”
It’s a position that aligned the government with the pharmaceutical industry, which argued that some hospitals had abused the program. Drugmakers pointed out that even with a cut to the reimbursement rate, the healthcare providers would still get the benefit of discounted drugs. A representative of PhRMA, a membership group for the pharmaceutical industry, declined an interview request, but sent BuzzFeed News a copy of comments the group submitted in support of the cut.
“PhRMA is concerned that the 340B program continues to grow rapidly and without patient benefits, thus increasingly departing from its purpose and statutory boundaries,” the group wrote. “This growth in the 340B program creates market-distorting incentives that affect consumer prices for medicines, shift care to more expensive hospital settings, and accelerate provider market consolidation.”
Hospitals that supported the program, meanwhile, said the proposal punished providers who work with vulnerable patients, and they urged the CMS to focus its efforts instead on bringing down drug costs.
The agency disputed that the plan was punitive and said that “lowering the price of pharmaceuticals is a top priority” but was outside the scope of what it was considering at the time.
Hospitals and hospital associations began suing the administration shortly after the rule became final in November 2017. They argued that the CMS had come up with the new rate using a process that Congress hadn’t approved. The agency admitted that it didn’t have the “statistically sound” survey data on what hospitals were actually paying for the drugs — the first method Congress had laid out — so instead it used an estimate of average purchase costs compiled by the Medicare Payment Advisory Commission, an agency that advises Congress.
The problem with the government’s approach, the hospitals argued, was that Congress had said the CMS could either use survey data on purchase costs or the average sales price of the drugs, but not a hybrid of the two. Congress had given the CMS authority to “adjust” rates, but cutting the reimbursement rate by nearly 30% was more than just an adjustment, the hospitals said.
US District Judge Rudolph Contreras in Washington, DC, sided with the hospitals. In a December 2018 opinion, he wrote that the rate cut’s “magnitude and its wide applicability inexorably lead to the conclusion” that the agency had “fundamentally altered” what Congress had spelled out.
The judge stopped short of blocking the rule and ordering the government to reimburse hospitals for the difference between the previous rate and the CMS’s new, lower rate, however, writing that it was “likely to be highly disruptive.” He noted that the payment system had to stay budget neutral, which meant the money would need to come from another source, a “quagmire that may be impossible to navigate” given how much money the government paid out of Medicare each year. He asked for more briefing on what the agency should do to fix the problem, but that issue was put on hold as the administration took the case to the DC Circuit.
A three-judge DC Circuit panel heard arguments on Nov. 8 and has yet to release a decision. In the meantime, hospitals have continued to file lawsuits as their claims for reimbursement at the previous, higher rate are rejected; earlier this month, a hospital system in Jacksonville, Florida, which is part of the University of Florida, filed a new suit in federal court in Washington. And the CMS is going ahead with its survey over the objections from hospitals.
“The pandemic amplifies the significance of this policy, but the fact remains that there were winners and losers with the policy and it’s always going to be a zero-sum game,” Cleary said. “If the court rules against the agency and the agency is forced to walk back the policy, that stands to negatively impact thousands of hospitals.”
Wiley, of American University, told BuzzFeed News that even before the pandemic, the fight over the 340B program highlighted how hospitals and drugmakers were “actively throwing each other under the bus” in the broader debate about who was to blame for the high cost of prescription drugs and what the federal government should do about it.
“Which stakeholders voters perceive to be the heroes of the pandemic response could affect health reform and reimbursement politics for years to come,” she wrote.