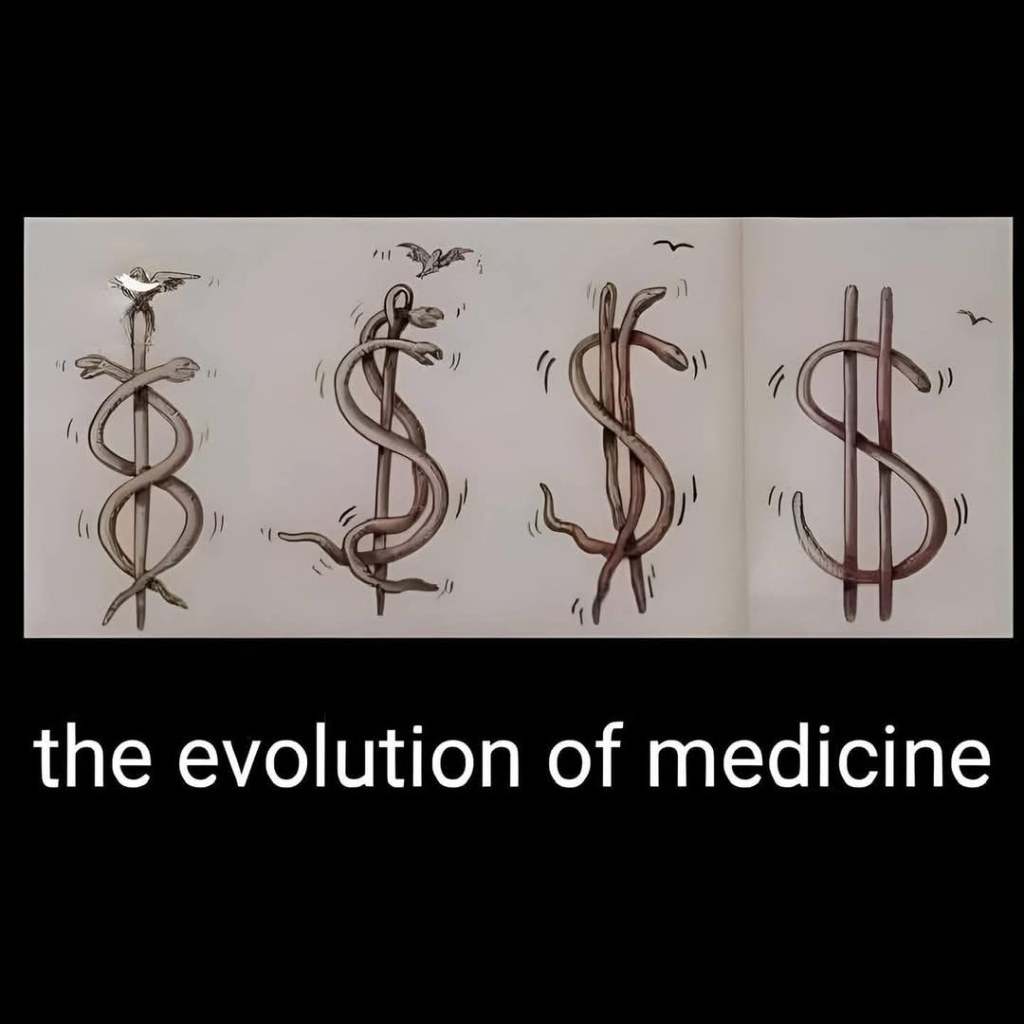
It’s no secret the brand name prescription drug costs are high. The rising costs have been blamed by health care analysts on kickbacks within the drug supply chain demanded by the federal government, drug distributors (wholesalers), health insurance companies and pharmacy benefit managers (PBMs).
This month we got a look at just how bloated brand-name drug prices have become in the United States thanks to an analysis from the Drug Channels Institute (DCI).
How about $356 billion worth of pure glut in the prescription drug supply chain, according to the analysis by DCI. Simply put, the market price established for these drugs by manufacturers has $356 billion worth of markups that mainly accommodate the financial demands (i.e. kickbacks or rebates) of groups that profit off the prescription drug system in the United States, health insurers and their PBMs in particular.
And that’s an all-time record.
Why?
Get ready to choke on your popcorn.
In the 1990s the federal government mandated in the Medicaid program that drug manufacturers offer a minimum rebate of 23% off the purchase price of brand name drugs. The feds also mandated that if drug manufacturers offer a better rebate on those drugs to someone else, the government also gets that same rebate.
The thought was no one gets a better deal than the federal government.
Medicaid then began to expand in the 2000s and the rebates and the demands increased.
Rebates expanded again as PBMs continued to gain more control over the drug supply chain. The PBMs now force drug manufacturers to offer significant concessions in order to get on the list of approved medications – known as a formulary – available to patients with health insurance.
To account for these demands, drug manufacturers set the list price for their brand name drugs with these price concessions baked into the number.
DCI’s analysis found that baking is $356 billion of goodies for health care companies paid for by the government and you.
It’s the same kind of concept as a U.S. popular clothing retailer that displays inflated retail costs on the tags of goods and then right below displaying a lower “sale” price to make the consumer think they got a deal.
Here’s another way of thinking of it: Just like Congress has a lot of “pork” in its spending bills, there’s also a lot of pork in prescription drug costs that have very little to do with anything, other than increase profits for the health care industry.
Though the federal government intended to create a better system for taxpayers back in the 1990s when it demanded rebates in the Medicaid system, it instead created a feeding frenzy for companies in the drug supply chain.
In the year 2000 just a handful of companies in the drug supply chain dotted the Fortune 100 list of most financially successful companies. Today there are four such companies in the top 10.
The Minnesota-based health care conglomerate UnitedHealth leads that pack. The company’s profits have soared in the last two decades largely due to increasing medical costs and prescription drug costs paid by Americans. It has leaped over companies like Exxon Mobile and Apple to become the third largest company in America. Only Walmart and Amazon take in more revenue.
The company employs more than 400,000, including doctors and clinicians and has its own pharmacy benefits manager called Optum Rx.
We reported last month that Americans spent $464 billion last year on prescription drugs. That was also an all-time record, which will likely be set again and again and again until reforms are enacted.