Nearly every country has struggled to contain the coronavirus and made mistakes along the way.
China committed the first major failure, silencing doctors who tried to raise alarms about the virus and allowing it to escape from Wuhan. Much of Europe went next, failing to avoid enormous outbreaks. Today, many countries — Japan, Canada, France, Australia and more — are coping with new increases in cases after reopening parts of society.
Yet even with all of these problems, one country stands alone, as the only affluent nation to have suffered a severe, sustained outbreak for more than four months: the United States.
Over the past month, about 1.9 million Americans have tested positive for the virus.
That’s more than five times as many as in all of Europe, Canada, Japan, South Korea and Australia, combined.
Even though some of these countries saw worrying new outbreaks over the past month, including 50,000 new cases in Spain …
… the outbreaks still pale in comparison to those in the United States. Florida, with a population less than half of Spain, has reported nearly 300,000 cases in the same period.
When it comes to the virus, the United States has come to resemble not the wealthy and powerful countries to which it is often compared but instead far poorer countries, like Brazil, Peru and South Africa, or those with large migrant populations, like Bahrain and Oman.
As in several of those other countries, the toll of the virus in the United States has fallen disproportionately on poorer people and groups that have long suffered discrimination. Black and Latino residents of the United States have contracted the virus at roughly three times as high of a rate as white residents.
How did this happen? The New York Times set out to reconstruct the unique failure of the United States, through numerous interviews with scientists and public health experts around the world. The reporting points to two central themes.
First, the United States faced longstanding challenges in confronting a major pandemic. It is a large country at the nexus of the global economy, with a tradition of prioritizing individualism over government restrictions. That tradition is one reason the United States suffers from an unequal health care system that has long produced worse medical outcomes — including higher infant mortality and diabetes rates and lower life expectancy — than in most other rich countries.
“As an American, I think there is a lot of good to be said about our libertarian tradition,” Dr. Jared Baeten, an epidemiologist and vice dean at the University of Washington School of Public Health, said. “But this is the consequence — we don’t succeed as well as a collective.”
The second major theme is one that public health experts often find uncomfortable to discuss because many try to steer clear of partisan politics. But many agree that the poor results in the United States stem in substantial measure from the performance of the Trump administration.
In no other high-income country — and in only a few countries, period — have political leaders departed from expert advice as frequently and significantly as the Trump administration. President Trump has said the virus was not serious; predicted it would disappear; spent weeks questioning the need for masks; encouraged states to reopen even with large and growing caseloads; and promoted medical disinformation.
In recent days, Mr. Trump has continued the theme, offering a torrent of misleading statistics in his public appearances that make the situation sound less dire than it is.
Some Republican governors have followed his lead and also played down the virus, while others have largely followed the science. Democratic governors have more reliably heeded scientific advice, but their performance in containing the virus has been uneven.
“In many of the countries that have been very successful they had a much crisper strategic direction and really had a vision,” said Caitlin Rivers, an epidemiologist at the Johns Hopkins Center for Health Security, who wrote a guide to reopening safely for the American Enterprise Institute, a conservative research group. “I’m not sure we ever really had a plan or a strategy — or at least it wasn’t public.”
Together, the national skepticism toward collective action and the Trump administration’s scattered response to the virus have contributed to several specific failures and missed opportunities, Times reporting shows:
-
a lack of effective travel restrictions;
-
repeated breakdowns in testing;
-
confusing advice about masks;
-
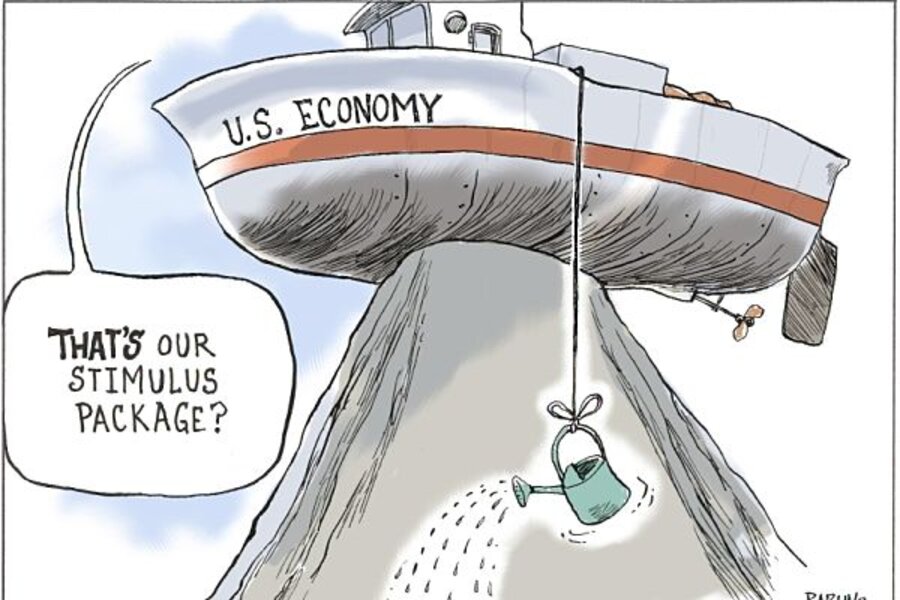
a misunderstanding of the relationship between the virus and the economy;
-
and inconsistent messages from public officials.
Already, the American death toll is of a different order of magnitude than in most other countries. With only 4 percent of the world’s population, the United States has accounted for 22 percent of coronavirus deaths. Canada, a rich country that neighbors the United States, has a per capita death rate about half as large. And these gaps may worsen in coming weeks, given the lag between new cases and deaths.
For many Americans who survive the virus or do not contract it, the future will bring other problems. Many schools will struggle to open. And the normal activities of life — family visits, social gatherings, restaurant meals, sporting events — may be more difficult in the United States than in any other affluent country.
A travel policy that fell short
In retrospect, one of Mr. Trump’s first policy responses to the virus appears to have been one of his most promising.
On Jan. 31, his administration announced that it was restricting entry to the United States from China: Many foreign nationals — be they citizens of China or other countries — would not be allowed into the United States if they had been to China in the previous two weeks.
It was still early in the spread of the virus. The first cases in Wuhan, China, had been diagnosed about a month before, and the first announced case in the United States had come on Jan. 21. In announcing the new travel policy, Alex M. Azar II, the secretary of health and human services, declared that the virus posed “a public health emergency.” Mr. Trump described the policy as his “China ban.”
After the Trump administration acted, several other countries quickly announced their own restrictions on travel from China, including Japan, Vietnam and Australia.
But it quickly became clear that the United States’ policy was full of holes. It did not apply to immediate family members of American citizens and permanent residents returning from China, for example. In the two months after the policy went into place, almost 40,000 people arrived in the United States on direct flights from China.
Even more important, the policy failed to take into account that the virus had spread well beyond China by early February. Later data would show that many infected people arriving in the United States came from Europe. (The Trump administration did not restrict travel from Europe until March and exempted Britain from that ban despite a high infection rate there.)
The administration’s policy also did little to create quarantines for people who entered the United States and may have had the virus.
Authorities in some other places took a far more rigorous approach to travel restrictions.
South Korea, Hong Kong and Taiwan largely restricted entry to residents returning home. Those residents then had to quarantine for two weeks upon arrival, with the government keeping close tabs to ensure they did not leave their home or hotel. South Korea and Hong Kong also tested for the virus at the airport and transferred anyone who was positive to a government facility.
Australia offers a telling comparison. Like the United States, it is separated from China by an ocean and is run by a conservative leader — Scott Morrison, the prime minister. Unlike the United States, it put travel restrictions at the center of its virus response.
Australian officials noticed in March that the travel restrictions they had announced on Feb. 1 were not preventing the virus from spreading. So they went further.
On March 27, Mr. Morrison announced that Australia would no longer trust travelers to isolate themselves voluntarily. The country would instead mandate that everyone arriving from overseas, including Australian citizens, spend two weeks quarantined in a hotel.
The protocols were strict. As people arrived at an airport, the authorities transported them directly to hotels nearby. People were not even allowed to leave their hotel to exercise. The Australian military helped enforce the rules.
Around the same time, several Australian states with minor outbreaks shut their own borders to keep out Australians from regions with higher rates of infection. That hardening of internal boundaries had not happened since the 1918 flu pandemic, said Ian Mackay, a virologist in Queensland, one of the first states to block entry from other areas.
The United States, by comparison, imposed few travel restrictions, either for foreigners or American citizens. Individual states did little to enforce the rules they did impose.
“People need a bit more than a suggestion to look after their own health,” said Dr. Mackay, who has been working with Australian officials on their pandemic response. “They need guidelines, they need rules — and they need to be enforced.”
Travel restrictions and quarantines were central to the success in controlling the virus in South Korea, Hong Kong, Taiwan and Australia, as well as New Zealand, many epidemiologists believe. In Australia, the number of new cases per day fell more than 90 percent in April. It remained near zero through May and early June, even as the virus surged across much of the United States.
In the past six weeks, Australia has begun to have a resurgence — which itself points to the importance of travel rules. The latest outbreak stems in large part from problems with the quarantine in the city of Melbourne. Compared with other parts of Australia, Melbourne relied more on private security contractors who employed temporary workers — some of whom lacked training and failed to follow guidelines — to enforce quarantines at local hotels. Officials have responded by banning out-of-state travel again and imposing new lockdowns.
Still, the tolls in Australia and the United States remain vastly different. Fewer than 300 Australians have died of complications from Covid-19, the illness caused by the virus. If the United States had the same per capita death rate, about 3,300 Americans would have died, rather than 158,000.
Enacting tough travel restrictions in the United States would not have been easy. It is more integrated into the global economy than Australia is, has a tradition of local policy decisions and borders two other large countries. But there is a good chance that a different version of Mr. Trump’s restrictions — one with fewer holes and stronger quarantines — would have meaningfully slowed the virus’s spread.
Traditionally, public health experts had not seen travel restrictions as central to fighting a pandemic, given their economic costs and the availability of other options, like testing, quarantining and contact tracing, Dr. Baeten, the University of Washington epidemiologist, said. But he added that travel restrictions had been successful enough in fighting the coronavirus around the world that those views may need to be revisited.
“Travel,” he said, “is the hallmark of the spread of this virus around the world.”
The double testing failure
On Jan. 16, nearly a week before the first announced case of the coronavirus in the United States, a German hospital made an announcement. Its researchers had developed a test for the virus, which they described as the world’s first.
The researchers posted the formula for the test online and said they expected that countries with strong public health systems would soon be able to produce their own tests. “We’re more concerned about labs in countries where it’s not that easy to transport samples, or staff aren’t trained that thoroughly, or if there is a large number of patients who have to be tested,” Dr. Christian Drosten, the director of the Institute for Virology at the hospital, known as Charité, in Berlin.
It turned out, however, that the testing problems would not be limited to less-developed countries.
In the United States, the Centers for Disease Control and Prevention developed their own test four days after the German lab did. C.D.C. officials claimed that the American test would be more accurate than the German one, by using three genetic sequences to detect the virus rather than two. The federal government quickly began distributing the American test to state officials.
But the test had a flaw. The third genetic sequence produced inconclusive results, so the C.D.C. told state labs to pause their work. In meetings of the White House’s coronavirus task force, Dr. Robert R. Redfield, the C.D.C. director, played down the problem and said it would soon be solved.
Instead, it took weeks to fix. During that time, the United States had to restrict testing to people who had clear reason to think they had the virus. All the while, the virus was quietly spreading.
By early March, with the testing delays still unresolved, the New York region became a global center of the virus — without people realizing it until weeks later. More widespread testing could have made a major difference, experts said, leading to earlier lockdowns and social distancing and ultimately less sickness and death.
“You can’t stop it if you can’t see it,” Dr. Bruce Aylward, a senior adviser to the director general at the World Health Organization, said.
While the C.D.C. was struggling to solve its testing flaws, Germany was rapidly building up its ability to test. Chancellor Angela Merkel, a chemist by training, and other political leaders were watching the virus sweep across northern Italy, not far from southern Germany, and pushed for a big expansion of testing.
By the time the virus became a problem in Germany, labs around the country had thousands of test kits ready to use. From the beginning, the government covered the cost of the tests. American laboratories often charge patients about $100 for a test.
Without free tests, Dr. Hendrik Streeck, director of the Institute of Virology at the University Hospital Bonn, said at the time, “a young person with no health insurance and an itchy throat is unlikely to go to the doctor and therefore risks infecting more people.”
Germany was soon far ahead of other countries in testing. It was able to diagnose asymptomatic cases, trace the contacts of new patients and isolate people before they could spread the virus. The country has still suffered a significant outbreak. But it has had many fewer cases per capita than Italy, Spain, France, Britain or Canada — and about one-fifth the rate of the United States.
The United States eventually made up ground on tests. In recent weeks, it has been conducting more per capita than any other country, according to Johns Hopkins researchers.
But now there is a new problem: The virus has grown even more rapidly than testing capacity. In recent weeks, Americans have often had to wait in long lines, sometimes in scorching heat, to be tested.
One measure of the continuing troubles with testing is the percentage of tests that come back positive. In a country that has the virus under control, fewer than 5 percent of tests come back positive, according to World Health Organization guidelines. Many countries have reached that benchmark. The United States, even with the large recent volume of tests, has not.
“We do have a lot of testing,” Ms. Rivers, the Johns Hopkins epidemiologist, said. “The problem is we also have a lot of cases.”
The huge demand for tests has overwhelmed medical laboratories, and many need days — or even up to two weeks — to produce results. “That really is not useful for public health and medical management,” Ms. Rivers added. While people are waiting for their results, many are also spreading the virus.
In Belgium recently, test results have typically come back in 48 to 72 hours. In Germany and Greece, it is two days. In France, the wait is often 24 hours.
The double mask failure
For the first few months of the pandemic, public health experts could not agree on a consistent message about masks. Some said masks reduced the spread of the virus. Many experts, however, discouraged the use of masks, saying — somewhat contradictorily — that their benefits were modest and that they should be reserved for medical workers.
“We don’t generally recommend the wearing of masks in public by otherwise well individuals because it has not been up to now associated with any particular benefit,” Dr. Michael Ryan, a World Health Organization official, said at a March 30 news conference.
His colleague Dr. Maria Van Kerkhove explained that it was important to “prioritize the use of masks for those who need them most.”
The conflicting advice, echoed by the C.D.C. and others, led to relatively little mask wearing in many countries early in the pandemic. But several Asian countries were exceptions, partly because they had a tradition of mask wearing to avoid sickness or minimize the effects of pollution.
By January, mask wearing in Japan was widespread, as it often had been during a typical flu season. Masks also quickly became the norm in much of South Korea, Thailand, Vietnam, Taiwan and China.
In the following months, scientists around the world began to report two strands of evidence that both pointed to the importance of masks: Research showed that the virus could be transmitted through droplets that hang in the air, and several studies found that the virus spread less frequently in places where people were wearing masks.
On one cruise ship that gave passengers masks after somebody got sick, for example, many fewer people became ill than on a different cruise where people did not wear masks.
Consistent with that evidence was Asia’s success in holding down the number of cases (after China’s initial failure to do so). In South Korea, the per capita death rate is about one-eightieth as large as in the United States; Japan, despite being slow to enact social distancing, has a death rate about one-sixtieth as large.
“We should have told people to wear cloth masks right off the bat,” Dr. George Rutherford of the University of California, San Francisco, said.
In many countries, officials reacted to the emerging evidence with a clear message: Wear a mask.
Prime Minister Justin Trudeau of Canada began wearing one in May. During a visit to an elementary school, President Emmanuel Macron of France wore a French-made blue mask that complemented his suit and tie. Zuzana Caputova, the president of Slovakia, created a social media sensation by wearing a fuchsia-colored mask that matched her dress.
In the United States, however, masks did not become a fashion symbol. They became a political symbol.
Mr. Trump avoided wearing one in public for months. He poked fun at a reporter who wore one to a news conference, asking the reporter to take it off and saying that wearing one was “politically correct.” He described former Vice President Joseph R. Biden Jr.’s decision to wear one outdoors as “very unusual.”
Many other Republicans and conservative news outlets, like Fox News, echoed his position. Mask wearing, as a result, became yet another partisan divide in a highly polarized country.
Throughout much of the Northeast and the West Coast, more than 80 percent of people wore masks when within six feet of someone else. In more conservative areas, like the Southeast, the share was closer to 50 percent.
A March survey found that partisanship was the biggest predictor of whether Americans regularly wore masks — bigger than their age or whether they lived in a region with a high number of virus cases. In many of the places where people adopted a hostile view of masks, including Texas and the Southeast, the number of virus cases began to soar this spring.
The first rule of virus economics
Throughout March and April, Gov. Brian Kemp of Georgia and staff members held long meetings inside a conference room at the State Capitol in Atlanta. They ordered takeout lunches from local restaurants like the Varsity and held two daily conference calls with the public health department, the National Guard and other officials.
One of the main subjects of the meetings was when to end Georgia’s lockdown and reopen the state’s economy. By late April, Mr. Kemp decided that it was time.
Georgia had not met the reopening criteria laid out by the Trump administration (and many outside health experts considered those criteria too lax). The state was reporting about 700 new cases a day, more than when it shut down on April 3.
Nonetheless, Mr. Kemp went ahead. He said that Georgia’s economy could not wait any longer, and it became one of the first states to reopen.
“I don’t give a damn about politics right now,” he said at an April 20 news conference announcing the reopening. He went on to describe business owners with employees at home who were “going broke, worried about whether they can feed their children, make the mortgage payment.”
Four days later, across Georgia, barbers returned to their chairs, wearing face masks and latex gloves. Gyms and bowling alleys were allowed to reopen, followed by restaurants on April 27. The stay-at-home order expired at 11:59 p.m. on April 30.
Mr. Kemp’s decision was part of a pattern: Across the United States, caseloads were typically much higher when the economy reopened than in other countries.
As the United States endured weeks of closed stores and rising unemployment this spring, many politicians — particularly Republicans, like Mr. Kemp — argued that there was an unavoidable trade-off between public health and economic health. And if crushing the virus meant ruining the economy, maybe the side effects of the treatment were worse than the disease.
Dan Patrick, the Republican lieutenant governor of Texas, put the case most bluntly, and became an object of scorn, especially from the political left, for doing so. “There are more important things than living,” Mr. Patrick said in a television interview the same week that Mr. Kemp reopened Georgia.
It may have been an inartful line, but Mr. Patrick’s full argument was not wholly dismissive of human life. He was instead suggesting that the human costs of shutting down the economy — the losses of jobs and income and the associated damages to living standards and people’s health — were greater than the costs of a virus that kills only a small percentage of people who get it.
“We are crushing the economy,” he said, citing the damage to his own children and grandchildren. “We’ve got to take some risks and get back in the game and get this country back up and running.”
The trouble with the argument, epidemiologists and economists agree, was that public health and the economy’s health were not really in conflict.
Early in the pandemic, Austan Goolsbee, a University of Chicago economist and former Obama administration official, proposed what he called the first rule of virus economics: “The best way to fix the economy is to get control of the virus,” he said. Until the virus was under control, many people would be afraid to resume normal life and the economy would not function normally.
The events of the last few months have borne out Mr. Goolsbee’s prediction. Even before states announced shutdown orders in the spring, many families began sharply reducing their spending. They were responding to their own worries about the virus, not any official government policy.
And the end of lockdowns, like Georgia’s, did not fix the economy’s problems. It instead led to a brief increase in spending and hiring that soon faded.
In the weeks after states reopened, the virus began surging. Those that opened earliest tended to have worse outbreaks, according to a Times analysis. The Southeast fared especially badly.
In June and July, Georgia reported more than 125,000 new virus cases, turning it into one of the globe’s new hot spots. That was more new cases than Canada, France, Germany, Italy, Japan and Australia combined during that time frame.
Americans, frightened by the virus’s resurgence, responded by visiting restaurants and stores less often. The number of Americans filing new claims for unemployment benefits has stopped falling. The economy’s brief recovery in April and May seems to have petered out in June and July.
In large parts of the United States, officials chose to reopen before medical experts thought it wise, in an attempt to put people back to work and spark the economy. Instead, the United States sparked a huge new virus outbreak — and the economy did not seem to benefit.
“Politicians are not in control,” Mr. Goolsbee said. “They got all the illness and still didn’t fix their economies.”
The situation is different in the European Union and other regions that have had more success reducing new virus cases. Their economies have begun showing some promising signs, albeit tentative ones. In Germany, retail sales and industrial production have risen, and the most recent unemployment rate was 6.4 percent. In the United States, it was 11.1 percent.
The message is the response
The United States has not performed uniquely poorly on every measure of the virus response.
Mask wearing is more common than throughout much of Scandinavia and Australia, according to surveys by YouGov and Imperial College London. The total death rate is still higher in Spain, Italy and Britain.
But there is one way — in addition to the scale of the continuing outbreaks and deaths — that the United States stands apart: In no other high-income country have the messages from political leaders been nearly so mixed and confusing.
These messages, in turn, have been amplified by television stations and websites friendly to the Republican Party, especially Fox News and the Sinclair Broadcast Group, which operates almost 200 local stations. To anybody listening to the country’s politicians or watching these television stations, it would have been difficult to know how to respond to the virus.
Mr. Trump’s comments, in particular, have regularly contradicted the views of scientists and medical experts.
The day after the first American case was diagnosed, he said, “We have it totally under control.” In late February, he said: “It’s going to disappear. One day — it’s like a miracle — it will disappear.” Later, he incorrectly stated that any American who wanted a test could get one. On July 28, he falsely proclaimed that “large portions of our country” were “corona-free.”
He has also promoted medical misinformation about the virus. In March, Mr. Trump called it “very mild” and suggested it was less deadly than the common flu. He has encouraged Americans to treat it with the antimalarial drug hydroxychloroquine, despite a lack of evidence about its effectiveness and concerns about its safety. At one White House briefing, he mused aloud about injecting people with disinfectant to treat the virus.
These comments have helped create a large partisan divide in the country, with Republican-leaning voters less willing to wear masks or remain socially distant. Some Democratic-leaning voters and less political Americans, in turn, have decided that if everybody is not taking the virus seriously, they will not either. State leaders from both parties have sometimes created so many exceptions about which workplaces can continue operating normally that their stay-at-home orders have had only modest effects.
“It doesn’t seem we have had the same unity of purpose that I would have expected,” Ms. Rivers, the Johns Hopkins epidemiologist, said. “You need everyone to come together to accomplish something big.”
Across much of Europe and Asia, as well as in Canada, Australia and elsewhere, leaders have delivered a consistent message: The world is facing a deadly virus, and only careful, consistent action will protect people.
Many of those leaders have then pursued aggressive action. Mr. Trump and his top aides, by contrast, persuaded themselves in April that the virus was fading. They have also declined to design a national strategy for testing or other virus responses, leading to a chaotic mix of state policies.
“If you had to summarize our approach, it’s really poor federal leadership — disorganization and denial,” said Andy Slavitt, who ran Medicare and Medicaid from 2015 to 2017. “Watch Angela Merkel. Watch how she communicates with the public. Watch how Jacinda Ardern in New Zealand does it. They’re very clear. They’re very consistent about what the most important priorities are.”
New York — both the city and the state — offers a useful case study. Like much of Europe, New York responded too slowly to the first wave of the virus. As late as March 15, Mayor Bill de Blasio encouraged people to go to their neighborhood bar.
Soon, the city and state were overwhelmed. Ambulances wailed day and night. Hospitals filled to the breaking point. Gov. Andrew M. Cuomo — a Democrat, like Mr. de Blasio — was slow to protect nursing home residents, and thousands died. Earlier action in New York could have saved a significant number of lives, epidemiologists say.
By late March, however, New York’s leaders understood the threat, and they reversed course.
They insisted that people stay home. They repeated the message every day, often on television. When other states began reopening, New York did not. “You look at the states that opened fast without metrics, without guardrails, it’s a boomerang,” Mr. Cuomo said on June 4.
The lockdowns and the consistent messages had a big effect. By June, New York and surrounding states had some of the lowest rates of virus spread in the country. Across much of the Southeast, Southwest and West Coast, on the other hand, the pandemic was raging.
Many experts now say that the most disappointing part of the country’s failure is that the outcome was avoidable.
What may not have been avoidable was the initial surge of the virus: The world’s success in containing previous viruses, like SARS, had lulled many people into thinking a devastating pandemic was unlikely. That complacency helps explains China’s early mistakes, as well as the terrible death tolls in the New York region, Italy, Spain, Belgium, Britain and other parts of Europe.
But these countries and dozens more — as well as New York — have since shown that keeping the virus in check is feasible.
For all of the continuing uncertainty about how this new coronavirus is transmitted and how it affects the human body, much has become clear. It often spreads indoors, with close human contact. Talking, singing, sneezing and coughing play a major role in transmission. Masks reduce the risk. Restarting normal activity almost always leads to new cases that require quick action — testing, tracing of patients and quarantining — to keep the virus in check.
When countries and cities have heeded these lessons, they have rapidly reduced the spread of the virus and been able to move back, gingerly, toward normal life. In South Korea, fans have been able to attend baseball games in recent weeks. In Denmark, Italy and other parts of Europe, children have returned to school.
In the United States, the virus continues to overwhelm daily life.
“This isn’t actually rocket science,” said Dr. Thomas R. Frieden, who ran the New York City health department and the C.D.C. for a combined 15 years. “We know what to do, and we’re not doing it.”