
Category Archives: Medicaid Block Grants
What Trump and the GOP have planned for healthcare

Health systems are rightly concerned about Republican plans to cut Medicaid spending, end ACA subsidies and enact site neutral payments, says consultant Michael Abrams, managing partner of Numerof, a consulting firm.
“Health systems have reason to worry,” Abrams said shortly after President Donald Trump was inaugurated on Monday.
While Trump mentioned little about healthcare in his inauguration speech, the GOP trifecta means spending cuts outlined in a one-page document released by Politico and another 50-pager could get a majority vote for passage.
Of the insurers, pharmaceutical manufacturers and health systems that Abrams consults with, healthcare systems are the ones that are most concerned, Abrams said.
At the top of the Republican list targeting $4 trillion in healthcare spending is eliminating an estimated $2.5 billion from Medicaid.
“There’s no question Republicans will find savings in Medicaid,” Abrams said.
Medicaid has doubled its enrollment in the last couple of years due to extended benefits made possible by the Affordable Care Act, despite disenrolling 25 million people during the redetermination process at the end of the public health emergency, according to Abrams.
Upward of 44 million people, or 16.4% of the non-elderly U.S. population are covered by an Affordable Care Act initiative, including a record high of 24 million people in ACA health plans and another 21.3 million in Medicaid expansion enrollment, according to a KFF report. Medicaid expansion enrollment is 41% higher than in 2020.
The enhanced subsidies that expanded eligibility for Medicaid and doubled the number of enrollees are set to expire at the end of 2025 and Republicans are likely to let that happen, Abrams said. Eliminating enhanced federal payments to states that expanded Medicaid under the ACA are estimated to cut the program by $561 billion.
If enhanced subsidies end, the Congressional Budget Office has estimated that the number of people who will become uninsured will increase by 3.8 million each year between 2026 and 2034.
The enhanced tax subsidies for the ACA are set to expire at the end of 2025. This could result in another 2.2 million people losing coverage in 2026, and 3.7 million in 2027, according to the CBO.
WHY THIS MATTERS
For hospitals, loss of health insurance coverage means an increase in sicker, uninsured patients visiting the emergency department and more uncompensated care.
“Health systems are nervous about people coming to them who are uninsured,” Abrams said. “There will be people disenrolled.”
The federal government allowed more people to be added to the Medicaid rolls during the public health emergency to help those who lost their jobs during the COVID-19 pandemic, Numerof said. Medicaid became an open-ended liability which the government wants to end now that the unemployment rate is around 4.2% and jobs are available.
An idea floating around Congress is the idea of converting Medicaid to a per capita cap and providing these funds to the states as a block grant, Abrams said. The cost of those programs would be borne 70% by the federal government and 30% by states.
This fixed amount based on a per person amount would save money over the current system of letting states report what they spent.
Another potential change under the new administration includes site neutral Medicare payments to hospitals for outpatient services.
The HFMA reported the site neutral policy as a concern in a list it published Monday of preliminary federal program cuts totaling more than $5 trillion over 10 years. The 50-page federal list is essentially a menu of options, the HFMA said, not an indication that programs will actually be targeted leading up to the March 14 deadline to pass legislation before federal funding expires.
Other financial concerns for hospitals based on that list include: the elimination of the tax exemption for nonprofit hospitals, bringing in up to $260 billion in estimated 10-year savings; and phasing out Medicare payments for bad debt, resulting in savings of up to $42 billion over a decade.
Healthcare systems are the ones most concerned over GOP spending cuts, according to Abrams. Pharmacy benefit managers and pharmaceutical manufacturers also remain on edge as to what might be coming at them next.
THE LARGER TREND
President Donald Trump mentioned little about healthcare during his inauguration speech on Monday.
Trump said the public health system does not deliver in times of disaster, referring to the hurricanes in North Carolina and other areas and to the fires in Los Angeles.
Trump also mentioned giving back pay to service members who objected to getting the COVID-19 vaccine.
He also talked about ending the chronic disease epidemic, without giving specifics.
“He didn’t really talk about healthcare even in the campaign,” Abrams said.
However, in his consulting work, Abrams said, “The common thread is the environment is changing quickly,” and that healthcare organizations need to do the same “in order to survive.”
Advocates roll out efforts to shield Medicaid
https://nxslink.thehill.com/view/6230d94bc22ca34bdd8447c8msmrk.ngi/32c5cdf6
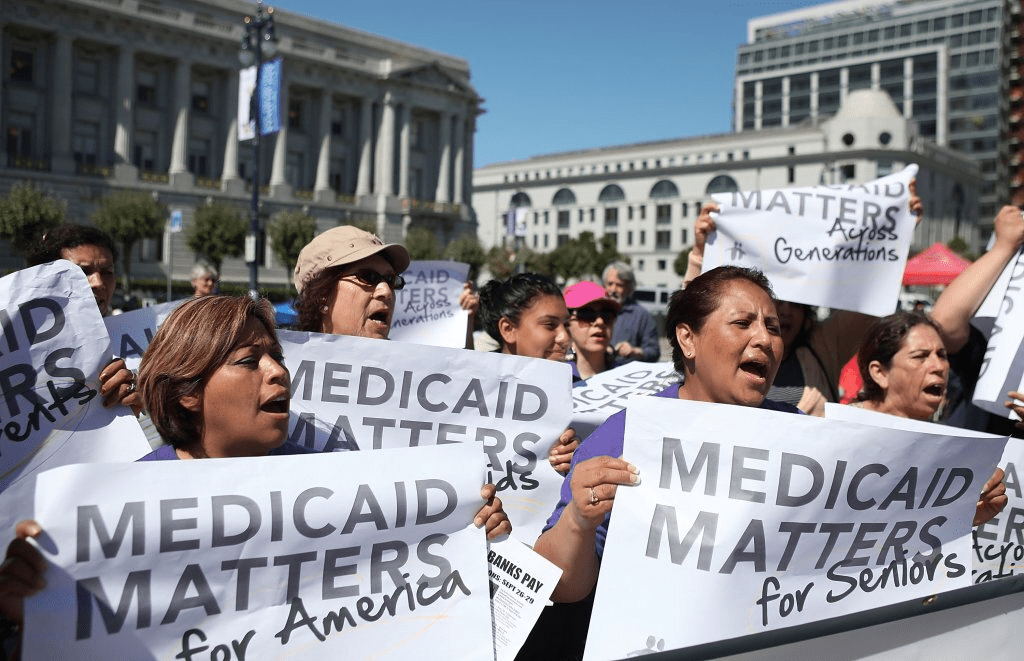
Liberal advocacy groups are ramping up efforts to protect the Medicaid program from potential cuts by Republican lawmakers and the new Trump administration.
The Democratic group Protect Our Care launched Tuesday an eight-figure “Hands off Medicaid” ad campaign targeting key Republicans in the House and Senate, warning of health care being “ripped away” from vulnerable Americans.
The lawmakers include GOP Sens. Bill Cassidy (La.), Chuck Grassley (Iowa), Lisa Murkowski (Alaska) and Susan Collins (Maine), as well as Reps. David Schweikert (Ariz.), Mike Lawler (N.Y.) and David Valadao (Calif.).
The campaign will also include digital advertising across platforms targeting the Medicaid population in areas around nursing homes and rural hospitals, ads on streaming platforms as well as billboards and bus stop wraps.
Medicaid covers 1 in 5 Americans, and the group wants to highlight that includes “kids, moms, seniors, people of color, rural Americans, and people with disabilities.”
“The American people didn’t vote in November to have their grandparents kicked out of nursing homes or health care ripped away from kids with disabilities or expectant moms in order to give Elon Musk another tax cut,” Protect Our Care chair Leslie Dach said in a statement.
House Republicans have expressed openness to making some drastic changes in the Medicaid program to pay for extending President Trump’s signature tax cuts, including instituting work requirements and capping how much federal money is spent per person. The ideas have been conservative mainstays since they were included as part of the 2017 Obamacare repeal effort.
Separately, advocacy group Families USA led a letter with more than 425 national, state and local organizations calling on Trump to protect Medicaid.
The groups noted that if the Trump administration wants to trim health costs, “there are many well-vetted, commonsense and bipartisan proposals” that don’t involve slashing Medicaid.
“In 2017, millions upon millions of Americans rose up against proposed cuts and caps and made clear how much they valued Medicaid as a critical health and economic lifeline for themselves, their families, and their communities. The American people are watching once again, and we urge you to take this opportunity to choose a different path,” they wrote.
Musk’s DOGE could leave millions uninsured
As Donald Trump begins his second term, America’s healthcare system is in crisis: medical costs are skyrocketing, life expectancy has stagnated, and burnout runs rampant among healthcare workers.
These problems are likely to become worse now that Trump has handed the federal budget over to Elon Musk. The world’s richest man now co-heads the Department of Government Efficiency (DOGE), a non-government entity tasked with slashing $500 billion in “wasteful” spending.
The harsh reality is that Musk’s mission can’t succeed without gutting healthcare access and coverage for millions of Americans.
Deleting dollars from American healthcare
Since Trump’s first term, the country’s economic outlook has worsened significantly. In 2016, the national debt was $19 trillion, with $430 billion allocated to annual interest payments. By 2024, the debt had nearly doubled to $36 trillion, requiring $882 billion in debt service—12% of federal spending that is legally untouchable.
Add to that another 50% of government expenditures that Trump has deemed politically off-limits: Social Security ($1.35 trillion), Medicare ($848 billion) and Defense ($1.13 trillion). That leaves just $2.6 trillion—less than 40% of the $6.75 trillion federal budget—available for cuts.
In a recent op-ed, Musk and DOGE co-chair Vivek Ramaswamy proposed eliminating expired or misused funds for programs like Public Broadcasting and Planned Parenthood, but these examples account for less than $3 billion total—not even 1% of their target.
This shortfall will require Musk to cut billions in government healthcare spending. But where will he find it?
With Medicare off limits to DOGE, the options for major reductions are extremely limited. Big-ticket healthcare items like the $300 billion in tax-deductibility for employer-sponsored health insurance and $120 billion in expired health programs for veterans will prove politically untouchable. One will raise taxes for 160 million working families and the latter will leave veterans without essential medical care.
This means DOGE will have to attack Medicaid and the ACA health exchanges. Here’s how 20 million people will likely lose coverage as a result.
1. Reduced ACA exchange funding
Since its enactment in 2010, the Affordable Care Act (ACA) has provided premium subsidies to Americans earning 100% to 400% of the federal poverty level. For lower-income families, the ACA also offers Cost Sharing Reductions, which help offset deductibles and co-payments that fund 30% of total medical costs per enrollee. Without CSRs, a family of four earning $40,000 could face deductibles as high as $5,000 before their insurance benefits apply.
If Congress allows CSR payments to expire in 2026, federal spending would decrease by approximately $35 billion annually. If that happens, the Congressional Budget Office expects 7 million individuals to drop out of the exchanges. Worse, without affordable coverage alternatives, 4 million families would lose their health insurance altogether.
2. Slashing Medicaid coverage and tightening eligibility
Medicaid currently provides healthcare for over 90 million low-income Americans, including children, seniors and individuals with disabilities. To meet DOGE’s $500 billion goal, several cost-cutting strategies appear likely:
- Reversing Medicaid expansion: The ACA expanded Medicaid eligibility to those earning up to 138% of the federal poverty level, reducing the uninsured rate from 16% to 8%. Undoing this expansion would strip coverage from millions in the 40 states that adopted the program.
- Imposing work requirements: Proponents argue this could encourage employment, but most Medicaid recipients already work for employers that don’t provide insurance. In reality, work requirements primarily create bureaucratic barriers that disqualify millions of eligible individuals, reducing program costs at the expense of coverage.
- Switching to block grants: Unlike the current Medicaid system, which adjusts funding based on need, less-expensive block grants would provide states with fixed allocations. This will, however, force them to cut services and reduce enrollment.
Medicaid currently costs $800 billion annually, with the federal government covering 70%. Reducing enrollment by 10% (9 million people) could save over $50 billion annually, while a 20% reduction (18 million people) could save $100 billion.
Either outcome would devastate families by eliminating access to vital services including prenatal care, vaccinations, chronic disease management and nursing home care. As states are forced to absorb the financial burden, they’ll likely cut education budgets and reduce infrastructure investments.
The first 100 days
The numbers don’t lie: Musk and DOGE could slash Medicaid funding and ACA subsidies to achieve much of their $500 billion target. But the human cost of this approach would be staggering.
Fortunately, there are alternative solutions that would reduce spending without sacrificing quality. Shifting provider payments in ways that reward better outcomes rather than higher volumes, capping drug prices at levels comparable to peer nations, and leveraging generative AI to improve chronic disease management could all drive down costs while preserving access to care.
These strategies address the root causes of high medical spending, including chronic diseases that, if better managed, could prevent 30-50% of heart attacks, strokes, cancers, and kidney failures according to CDC estimates.
Yet, in their pursuit of immediate budgetary cuts, Musk and DOGE have omitted these kinds of reform options. As a result, the health of millions of Americans is at major risk.
GOP allies drawing up health plans for a Republican administration
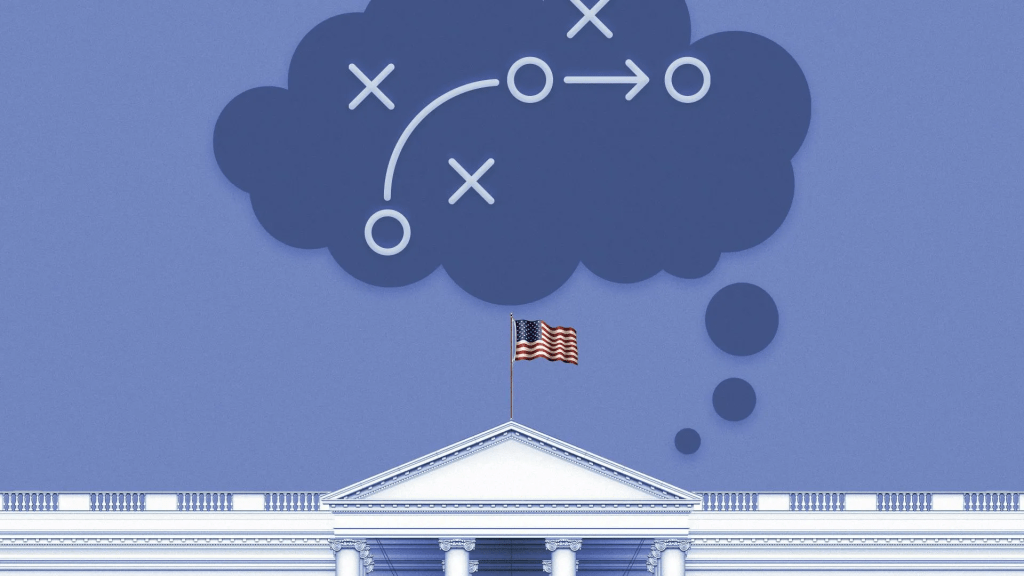
Influential conservative policy groups are sketching out health care plans for a potential Republican administration over a year before the election.
Why it matters:
Republicans have moved on from the “repeal and replace” — the Affordable Care Act didn’t even get a mention in the first GOP presidential debate last week — but still haven’t settled on new health care agenda.
- Republican-aligned groups are stepping in to build out ideas for a party platform that may not be as ambitious as an ACA replacement but could still shift health care policy in a conservative direction on everything from Medicaid to abortion to public health.
Context:
The early push to define the next GOP health agenda partly stems from Republicans’ inability to agree on an ACA alternative after former President Trump was elected, despite years of promises to overhaul the 2010 health care law. The GOP policy experts also said they want to avoid repeating the Trump administration’s failure to plan health care executive actions and key staffing decisions before taking office.
- “A large part of it comes from the experience of 2017. There wasn’t a clear agenda that was ready to go,” said Brian Blase, a former Trump administration health official who’s now president of the right-leaning Paragon Health Institute.
Details:
Conservative think tanks are looking to advance some long-held conservative goals like transforming Medicaid’s open-ended entitlement into block grants, but there’s also a new generation of Trump alumni who hope to revive some of his administration’s policies.
- These include initiatives like encouraging businesses to form association health plans, and pushing even further on price transparency and curbing higher payments to hospitals’ outpatient departments.
- Some are also drawing up plans for limiting the CDC’s power over public health policy in reaction to what they view as the agency’s failed response to the COVID-19 pandemic.
Zoom in:
Paragon Health, as well as the Heritage Foundation and America First Policy Institute, are the primary conservative think tanks now drafting health regulations, policy plans and recruiting personnel who could serve in a Republican administration.
- A roadmap from Paragon envisions a burst of rulemaking at the beginning of a new administration, mostly through the Department of Health and Human Services.
Meanwhile, the America First Policy Institute, founded by Trump administration alumni in 2021, has put forward a 12-part health policy agenda it describes as “radical incrementalism.”
- That’s an acknowledgement that they’re not planning a major health care overhaul, but a belief that significant changes are possible in the current structure, said former Louisiana Gov. Bobby Jindal, who chairs the group’s health policy division.
- “We are advocating specific policies that try to reform our health care system in a very specific direction that empowers patients … that makes health care more affordable, accessible, that improves outcomes by giving control back to individual patients working with their providers, not government agencies and programs. But, we’re not trying to write the next 3,000-page bill,” Jindal said.
- Some of those incremental ideas they hope could get bipartisan support, such as broadening health savings accounts for those with chronic conditions, expanding telehealth flexibilities for providers across state lines, implementing transparency for pharmacy benefit managers and speeding up deployment of biosimilars.
The Heritage Foundation has also detailed policy proposals and recently joined more than 70 other conservative groups to launch an initiative called Project 2025 to develop a governing agenda.
- One of those Heritage policy proposals laid out earlier this year illustrates how a future GOP president could overhaul HHS.
- Heritage’s plan contains the most detailed ideas for how the next GOP president — who would be the first since the demise of Roe v. Wade — could implement anti-abortion policies, cut off Medicaid funding to Planned Parenthood, and roll back Biden administration initiatives aimed at increasing access to abortion.
- The group also envisions splitting CDC into two agencies — one for research and data collection and another for making public health recommendations with “severely confined ability” to influence policy.
What we’re watching: The GOP presidential candidates themselves have said relatively little so far about their plans for the health care system. That could eventually change, given Americans’ concern over health care costs.
If Economists Chose the Health Care System

Health economists study the economic determinants of health. They also analyze how health care resources are utilized and allocated, and how health care policies and quality of care can be improved. In this episode, we discuss what exactly a healthcare system would look like if these professionals were calling all the shots.
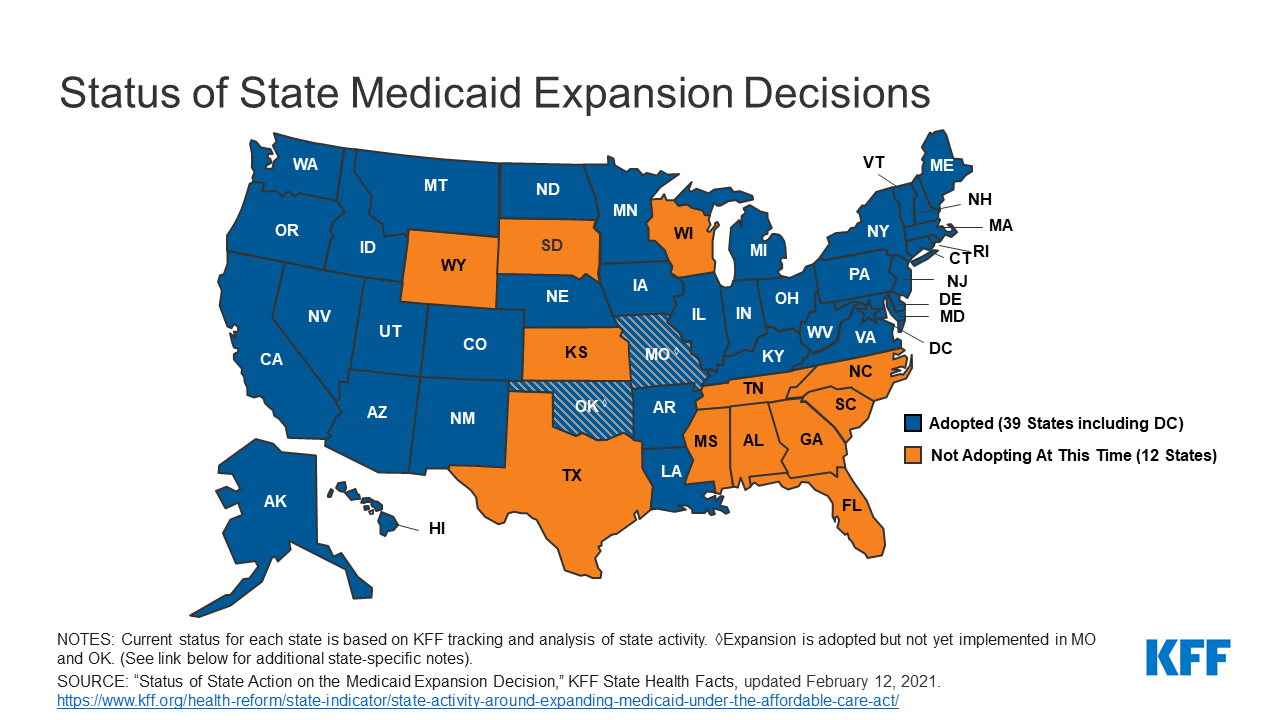
Why Biden Has a Chance to Cut Deals With Red State Holdouts on Medicaid
President Joe Biden has an unexpected opening to cut deals with red states to expand Medicaid, raising the prospect that the new administration could extend health protections to millions of uninsured Americans and reach a goal that has eluded Democrats for a decade.
The opportunity emerges as the covid-19 pandemic saps state budgets and strains safety nets. That may help break the Medicaid deadlock in some of the 12 states that have rejected federal funding made available by the Affordable Care Act, health officials, patient advocates and political observers say.
Any breakthrough will require a delicate political balancing act. New Medicaid compromises could leave some states with safety-net programs that, while covering more people, don’t insure as many as Democrats would like. Any expansion deals would also need to allow Republican state officials to tell their constituents they didn’t simply accept the 2010 health law, often called Obamacare.
“Getting all the remaining states to embrace the Medicaid expansion is not going to happen overnight,” said Matt Salo, executive director of the nonpartisan National Association of Medicaid Directors. “But there are significant opportunities for the Biden administration to meet many of them halfway.”
Key to these potential compromises will likely be federal signoff on conservative versions of Medicaid expansion, such as limits on who qualifies for the program or more federal funding, which congressional Democrats have proposed in the latest covid relief bill.
But any deals would bring the country closer to fulfilling the promise of the 2010 law, a pillar of Biden’s agenda, and begin to reverse Trump administration efforts to weaken public programs, which swelled the ranks of the uninsured.
“A new administration with a focus on coverage can make a difference in how these states proceed,” said Cindy Mann, who oversaw Medicaid in the Obama administration and now consults extensively with states at the law firm Manatt, Phelps & Phillips.
Medicaid, the half-century-old health insurance program for the poor and people with disabilities, and the related Children’s Health Insurance Program cover more than 70 million Americans, including nearly half the nation’s children.
Enrollment surged following enactment of the health law, which provides hundreds of billions of dollars to states to expand eligibility to low-income, working-age adults.
However, enlarging the government safety net has long been anathema to most Republicans, many of whom fear that federal programs will inevitably impose higher costs on states.
And although the GOP’s decade-long campaign to “repeal and replace” the health law has largely collapsed, hostility toward it remains high among Republican voters.
That makes it perilous for politicians to embrace any part of it, said Republican pollster Bill McInturff, a partner at Public Opinion Strategies. “A lot of Republican state legislators are sitting in core red districts, looking over their shoulders at a primary challenge,” he said.
Many conservatives have called instead for federal Medicaid block grants that cap how much federal money goes to states in exchange for giving states more leeway to decide whom they cover and what benefits their programs offer.
Many Democrats and patient advocates fear block grants will restrict access to care. But just before leaving office, the Trump administration gave Tennessee permission to experiment with such an approach.
“It’s a frustrating place to be,” said Tom Banning, the longtime head of the Texas Academy of Family Physicians, which has labored to persuade the state’s Republican leaders to drop their opposition to expanding Medicaid. “Despite covid and despite all the attention on health and disparities, we see almost no movement on this issue.”
Some 1.5 million low-income Texans are shut out of Medicaid because the state has resisted expansion, according to estimates by KFF. (KHN is an editorially independent program of KFF.)
An additional 800,000 people are locked out in Florida, which has also blocked expansion.
Two million more are caught in the 10 remaining holdouts: Alabama, Georgia, Kansas, Mississippi, North Carolina, South Carolina, South Dakota, Tennessee, Wisconsin and Wyoming.
Advocates of Medicaid expansion, which is broadly popular with voters, believe they may be able to break through in a handful of these states that allow ballot initiatives, including Mississippi and South Dakota.
Since 2018, voters in Idaho, Nebraska, Utah, Oklahoma and Missouri have backed initiatives to expand Medicaid eligibility, effectively circumventing Republican political leaders.
“The work that we’ve done around the country shows that no matter where people live — red state or blue state — there is overwhelming support for expanding access to health care,” said Kelly Hall, policy director of the Fairness Project, a nonprofit advocacy group that has helped organize the Medicaid measures.
But most of the holdout states, including Texas, don’t allow citizens to put initiatives on the ballot without legislative approval.
And although Florida has an initiative process, mounting a ballot campaign there is challenging, as political advertising is expensive. Unlike in many states, Florida’s leading hospital association hasn’t backed expansion.
Another route for expansion: compromises that could win over skeptical Republican state leaders and still get the green light from the Biden administration.
The Obama administration approved conservative Medicaid expansion in Arkansas, which funneled enrollees into the commercial insurance market, and in Indiana, which forced enrollees to pay more for their medical care.
Money is a major focus of current talks in several states, according to health officials, advocates and others involved in efforts across the country.
The health law at first fully funded Medicaid expansion with federal money, but after the first three years, states had to begin paying part of the tab. Now, states must come up with 10% of the cost of expansion.
Even that small share is a challenge for states, many of which are reeling from the economic downturn caused by the pandemic, said David Becker, a health economist at the University of Alabama-Birmingham who has assisted efforts to expand Medicaid in that state.
“The question is: Where do we get the money?” Becker said, noting that some Republicans may be open to expanding Medicaid if the federal government pays the full cost of the expansion, at least for a year or two.
Other efforts to find ways to offset state costs are underway in Kansas and North Carolina, which have Democratic governors whose expansion plans have been blocked by Republican state legislators. Kansas Gov. Laura Kelly this month proposed using money from the sale and taxation of medical marijuana.
Some Democrats in Congress are pushing to revise the health law to provide full federal funding to states that expand Medicaid now. Separately, in the stimulus bill unveiled last week, House Democrats proposed an additional boost in total Medicaid aid to states that expand.
Other Republicans have signaled interest in partly expanding Medicaid, opening the program to people making up to 100% of the federal poverty level, or about $12,900, rather than 138%, or $17,800, as the law stipulated.
The Obama administration rejected this approach, but the idea has gained traction in several states, including Georgia.
It’s unclear what kind of compromises the new administration may consider, as Biden has yet to even nominate someone to oversee the Medicaid program.
Some Democrats say it’s time to give up the search for middle ground with Republicans on Medicaid.
A better strategy, they say, is a new government insurance plan, or public option, for people in non-expansion states, a strategy Biden endorsed on the campaign trail.
“Democrats can no longer countenance millions of Americans living in poverty without insurance,” said Chris Jennings, a Democratic health care strategist who worked in the White House under Presidents Bill Clinton and Barack Obama and served on Biden’s transition team.
“This is why the Biden public option or other new ways to secure affordable, meaningful care should become the order of the day for people living in states like Florida and Texas.”
Biden to reopen ACA insurance marketplaces as pandemic has cost millions of Americans their coverage

President Biden is scheduled to take executive actions as early as Thursday to reopen federal marketplaces selling Affordable Care Act health plans and to lower recent barriers to joining Medicaid.
The orders will be Biden’s first steps since taking office to help Americans gain health insurance, a prominent campaign goal that has assumed escalating significance as the pandemic has dramatized the need for affordable health care — and deprived millions of Americans coverage as they have lost jobs in the economic fallout.
Under one order, HealthCare.gov, the online insurance marketplace for Americans who cannot get affordable coverage through their jobs, will swiftly reopen for at least a few months, according to several individuals inside and outside the administration familiar with the plans. Ordinarily, signing up for such coverage is tightly restricted outside a six-week period late each year.
Another part of Biden’s scheduled actions, the individuals said, is intended to reverse Trump-era changes to Medicaid that critics say damaged Americans’ access to the safety-net insurance. It is unclear whether Biden’s order will undo a Trump-era rule allowing states to impose work requirements, or simply direct federal health officials to review rules to make sure they expand coverage to the program that insures about 70 million low-income people in the United States.
The actions are part of a series of rapid executive orders the president is issuing in his initial days in office to demonstrate he intends to steer the machinery of government in a direction far different from that of his predecessor.
Biden has been saying for many months that helping people get insurance is a crucial federal responsibility. Yet until the actions planned for this week, he has not yet focused on this broader objective, shining a spotlight instead on trying to expand vaccinations and other federal responses to the pandemic.
The most ambitious parts of Biden’s campaign health-care platform would require Congress to provide consent and money. Those include creating a government insurance option alongside the ACA health plans sold by private insurers, and helping poor residents afford ACA coverage if they live in about a dozen states that have not expanded their Medicaid programs under the decade-old health law.
A White House spokesman declined to discuss the plans. Two HHS officials, speaking on the condition of anonymity about an event the White House has not announced, said Monday they were anticipating that the event would be held on Thursday.
According to a document obtained by The Washington Post, the president also intends to sign an order rescinding the so-called Mexico City rule, which compels nonprofits in other countries that receive federal family planning aid to promise not to perform or encourage abortions. Biden advisers last week previewed an end to this rule, which for decades has reappeared when Republicans occupied the White House and vanished under Democratic presidents.
The document also says Biden will disavow a multinational antiabortion declaration that the Trump administration signed three months ago.
The actions to expand insurance through the ACA and Medicaid come as the Supreme Court is considering two cases that could shape the outcome. One case is an effort to overturn rulings by lower federal courts, which have held that state rules, requiring some residents to work or prepare for jobs to qualify for Medicaid, are illegal. The other case involves an attempt to overturn the entire ACA.
According to the individuals inside and outside the administration, the order to reopen the federal insurance marketplaces will be framed in the context of the pandemic, essentially saying that anyone eligible for ACA coverage who has been harmed by the coronavirus will be allowed to sign up.
“This is absolutely in the covid age and the recession caused by covid,” said a health-care policy leader who has been in discussions with the administration. “There is financial displacement we need to address,” said this person, who spoke on the condition of anonymity to describe plans the White House has not announced.
The reopening of HealthCare.gov will be accompanied by an infusion of federal support to draw attention to the opportunity through advertising and other outreach efforts. This, too, reverses the Trump administration’s stance that supporting such outreach was wasteful. During its first two years, it slashed money for advertising and for community groups known as navigators that helped people enroll.
It is not clear whether restoring outreach will be part of Biden’s order or will be done more quietly within federal health-care agencies.
Federal rules already allow people to qualify for a special enrollment period to buy ACA health plans if their circumstances change in important ways, including losing a job. But such exceptions require people to seek permission individually, and many are unaware they can do so. Trump health officials also tightened the rules for qualifying for special enrollment.
In contrast, Biden is expected to open enrollment without anyone needing to seek permission, said Eliot Fishman, senior director of health policy for Families USA, a consumer health-advocacy group.
In the early days of the pandemic, the health insurance industry and congressional Democrats urged the Trump administration to reopen HealthCare.gov, the online federal ACA enrollment system on which three dozen states rely, to give more people the opportunity to sign up. At the end of March, Trump health officials decided against that.
During the most recent enrollment period, ending the middle of last month, nearly 8.3 million people signed up for health plans in the states using HealthCare.gov. The figure is about the same as the previous year, even though it includes two fewer states, which began operating their own marketplaces.
Leaders of groups helping with enrollment around the country said they were approached for help this last time by many people who had lost jobs or income because of the pandemic.
The order involving Medicaid is designed to alter course on experiments — known as “waivers” — that allow states to get federal permission to run their Medicaid programs in nontraditional ways. The work requirements, blocked so far by federal courts, are one of those experiments. Another was an announcement a year ago by Seema Verma, the Trump administration’s administrator of the Centers for Medicare and Medicaid Services, that states could apply for a fundamental change to the program, favored by conservatives, that would cap its funding, rather than operating as an entitlement program with federal money rising and falling with the number of people covered.
“You could think about it as announcing a war against the war on Medicaid,” said Katherine Hempstead, a senior policy adviser at the Robert Wood Johnson Foundation.
Dan Mendelson, founder of Avalere Health, a consulting firm, said Biden’s initial steps to broaden insurance match his campaign position that the United States does not need to switch to a system of single-payer insurance favored by more liberal Democrats.
The orders the president will sign “are going to do it through the existing programs,” Mendelson said.
The new administration unveils a national COVID strategy
https://mailchi.mp/128c649c0cb4/the-weekly-gist-january-22-2021?e=d1e747d2d8

As one of his first official actions upon taking office Wednesday, President Biden signed an executive order implementing a federal mask mandate, requiring masks to be worn by all federal employees and on all federal properties, as well as on all forms of interstate transportation. Yesterday Biden followed that action by officially naming his COVID response team, and issuing a detailed national plan for dealing with the pandemic. Describing the plan as a “full-scale wartime effort”, Biden highlighted the key components of the plan in an appearance with Dr. Anthony Fauci and COVID response coordinator Jeffrey Zients.
The plan instructs federal agencies to invoke the Defense Production Act to ensure adequate supplies of critical equipment, including masks, testing equipment, and vaccine-related supplies; calls for new national guidelines to help employers make workplaces safe for workers to return to their jobs, and to make schools safe for students to return; and promises to fully fund the states’ mobilization of the National Guard to assist in the vaccine rollout.
Also included in the plan is a new Pandemic Testing Board, charged with ramping up multiple forms of COVID testing; more investment in data gathering and reporting on the impact of the pandemic; and the establishment of a health equity task force, to ensure that vulnerable populations are an area of priority in pandemic response.
But Biden can only do so much by executive order. Funding for much of his ambitious COVID plan will require quick legislative action by Congress, meaning that the administration will either need to garner bipartisan support for its proposed “American Rescue Plan” legislation, or use the Senate’s budget reconciliation process to pass the bill with a simple majority (with Vice President Harris casting the tie-breaking vote). Even that may prove challenging, given skepticism among Republican (and some moderate Democratic) senators about the $1.9T price tag for the legislation.
We’d anticipate intense bargaining over the relief package—with broad agreement over the approximately $415B in spending on direct COVID response, but more haggling over the size of the economic stimulus component, including the promised $1,400 per person in direct financial assistance, expanded unemployment insurance, and raising the federal minimum wage to $15 per hour.
Some of the broader economic measures, along with the rest of Biden’s healthcare agenda and his larger proposals to invest in rebuilding critical infrastructure, may have to wait for future legislation, as the administration prioritizes COVID relief as its first—and most important—order of business.

Trump Administration Approves First Medicaid Block Grant, in Tennessee
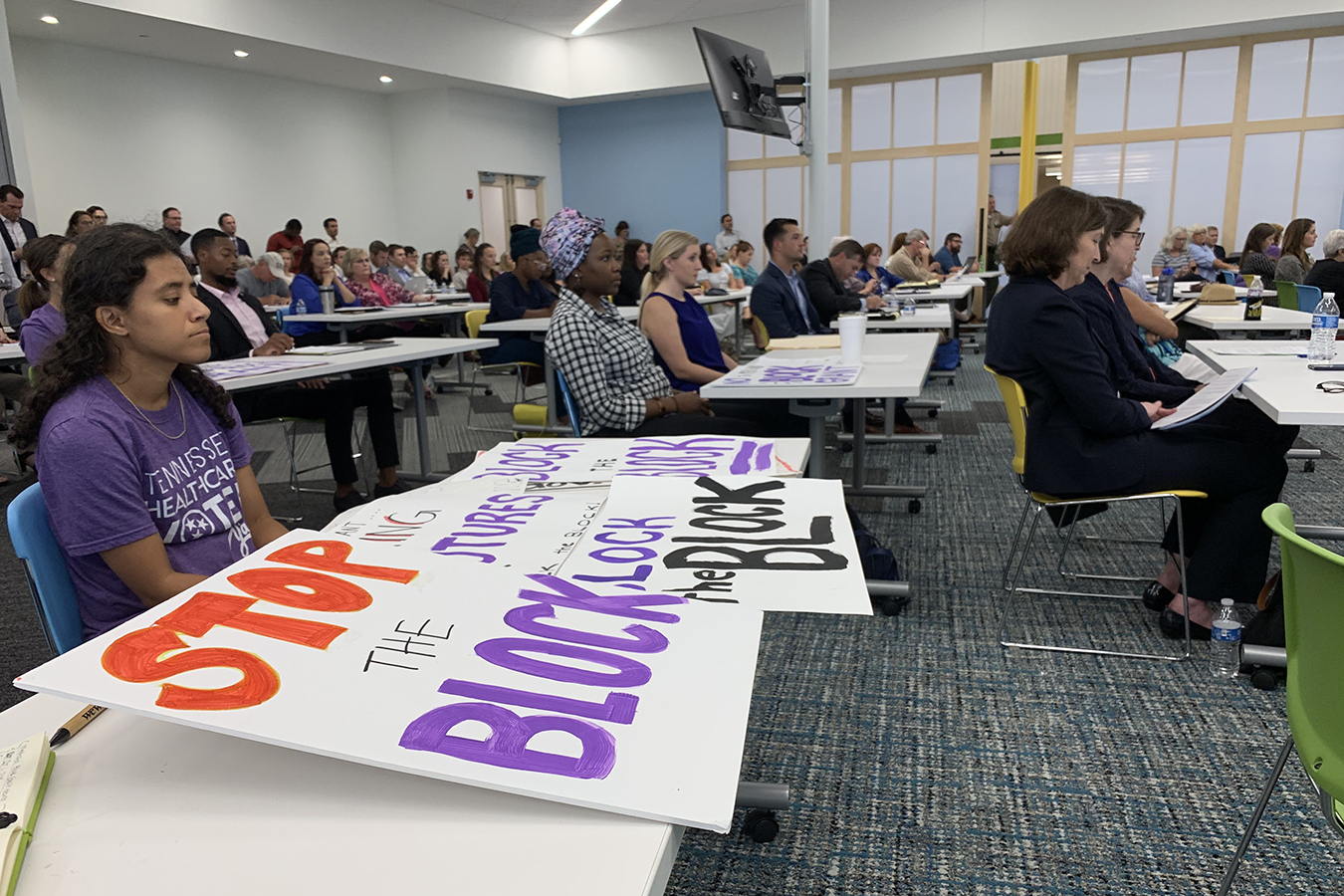
With just a dozen days left in power, the Trump administration on Friday approved a radically different Medicaid financing system in Tennessee that for the first time would give the state broader authority in running the health insurance program for the poor in exchange for capping its annual federal funding.
The approval is a 10-year “experiment.” Instead of the open-ended federal funding that rises with higher enrollment and health costs, Tennessee will instead get an annual block grant. The approach has been pushed for decades by conservatives who say states too often chafe under strict federal guidelines about enrollment and coverage and can find ways to provide care more efficiently.
But under the agreement, Tennessee’s annual funding cap will increase if enrollment grows. What’s different is that unlike other states, federal Medicaid funding in Tennessee won’t automatically keep up with rising per -person Medicaid expenses.
The approval, however, faces an uncertain future because the incoming Biden administration is likely to oppose such a move. But to unravel it, officials would need to set up a review that includes a public hearing.
Meanwhile, the changes in Tennessee will take months to implement because they need final legislative approval, and state officials must negotiate quality of care targets with the administration.
TennCare, the state’s Medicaid program, said the block grant system would give it unprecedented flexibility to decide who is covered and what services it will pay for.
Under the agreement, TennCare will have a specified spending cap based on historical spending, inflation and predicted future enrollment changes. If the state can operate the program at a lower cost than the cap and maintain or improve quality, the state then shares in the savings.
Trump administration officials said the approach adds incentive for the state to save money, unlike the current system, in which increased state spending is matched with more federal dollars. If Medicaid enrollment grows, the state can secure additional federal funding. If enrollment drops, it will get less money.
“This groundbreaking waiver puts guardrails in place to ensure appropriate oversight and protections for beneficiaries, while also creating incentives for states to manage costs while holding them accountable for improving access, quality and health outcomes,” said Seema Verma, administrator of the Centers for Medicare & Medicaid Services. “It’s no exaggeration to say that this carefully crafted demonstration could be a national model moving forward.”
Opponents, including most advocates for low-income Americans, say the approach will threaten care for the 1.4 million people in TennCare, who include children, pregnant women and the disabled. Federal funding covers two-thirds of the cost of the program.
Michele Johnson, executive director of the Tennessee Justice Center, said the block grant approval is a step backward for the state’s Medicaid program.
“No other state has sought a block grant, and for good reason. It gives state officials a blank check and creates financial incentives to cut health care to vulnerable families,” she said.
The agreement is different from traditional block grants championed by conservatives since it allows Tennessee to get more federal funding to keep up with enrollment growth. In addition, while the state is given flexibility to increase benefits, it can’t cut them on its own.
Democrats have fought back block grant Medicaid proposals since the Reagan administration and most recently in 2018 as part of Republicans’ failed effort to repeal and replace major parts of the Affordable Care Act. Even some key Republicans opposed the idea because it would cut billions in funding to states, making it harder to help the poor.
Implementing block grants via an executive branch action rather than getting Congress to amend Medicaid law is also likely to be met with court challenges.
“This is an illegal move that could threaten access to health care for vulnerable people in the middle of a pandemic,” Rep. Frank Pallone (D-N.J.), chair of the House Energy and Commerce Committee, posted on his Twitter account. “I’m hopeful the Biden Administration will move quickly to rollback this harmful policy as soon as possible.”
The block grant approval comes as Medicaid enrollment is at its highest-ever level.
More than 76 million Americans are covered by the state-federal health program, a million more than when the Trump administration took charge in 2017. Enrollment has jumped by more than 5 million in the past year as the economy slumped with the pandemic.
Medicaid, part of President Lyndon B. Johnson’s “Great Society” initiative of the 1960s, is an entitlement program in which the government pays each state a certain percentage of the cost of care for anyone eligible for the health coverage. As a result, the more money states spend on Medicaid, the more they get from Washington.
Under the approved demonstration, CMS will work with Tennessee to set spending targets that will increase at a fixed amount each year.
The plan includes a “safety valve” to increase federal funding due to unexpected increases in enrollment.
“The safety valve will maintain Tennessee’s commitment to enroll all eligible Tennesseans with no reduction in today’s benefits for beneficiaries,” CMS said in a statement.
Tennessee has committed to maintaining coverage for eligible beneficiaries and existing services.
In exchange for taking on this financing approach, the state will receive a range of operating flexibilities from the federal government, as well as up to 55% of the savings generated on an annual basis when spending falls below the aggregate spending cap and the state meets certain quality targets, yet to be determined.
The state can spend that money on various health programs for residents, including areas that Medicaid funding typically doesn’t cover, such as improving transportation and education and employment services for enrollees.
The 10-year waiver is unusual, but the Trump administration has approved such long-term experiments in recent years to give states more flexibility.
Tennessee is one of 12 states that have not approved expanding Medicaid under the Affordable Care Act, leaving tens of thousands of working adults without health insurance.
“The block grant is just another example of putting politics ahead of health care during this pandemic,” said Johnson of the Tennessee Justice Center. “Now is absolutely not the time to waste our energy and resources limiting who can access health care.”
State officials applauded the approval.
“It’s a legacy accomplishment,” said Tennessee Gov. Bill Lee, a Republican. “This new flexibility means we can work toward improving maternal health coverage and clearing the waiting list for developmentally disabled.”
“This means we will be able to make additional investments in TennCare without reduction in services and provider cuts.”

