With both Republicans and Democrats taking on these Goliaths individually, this could be a watershed moment for bi-partisan action.
The push and pull between providers and insurance companies is as old as our health payment system. Doctors have long argued insurers pay too little and that they too often interfere in patient care.
Dramatic increases in prior authorization, aggressive payment negotiations and less-generous reimbursement to doctors by Medicare Advantage plans show there’s little question the balance of power in this equation has swung toward payers.
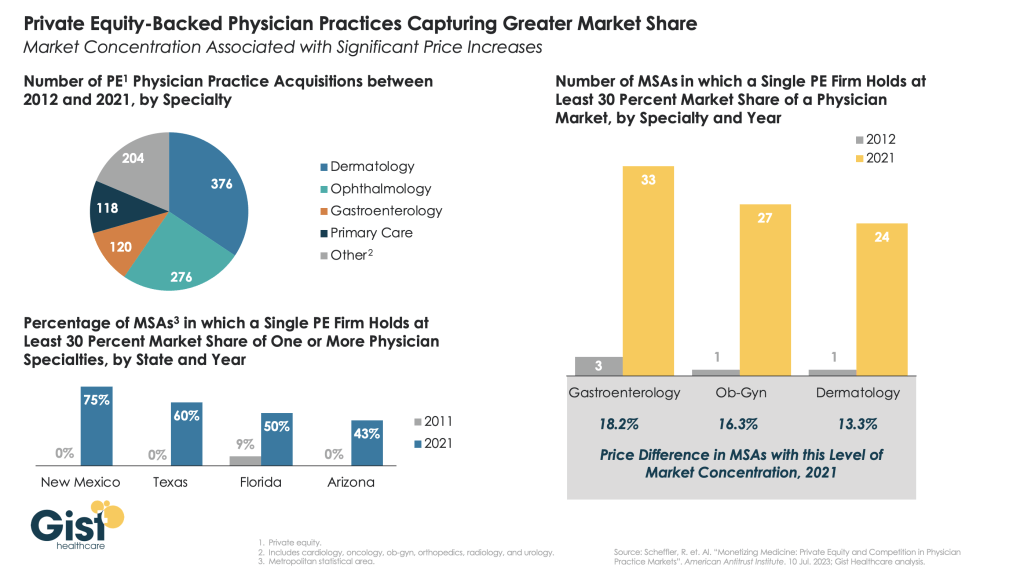
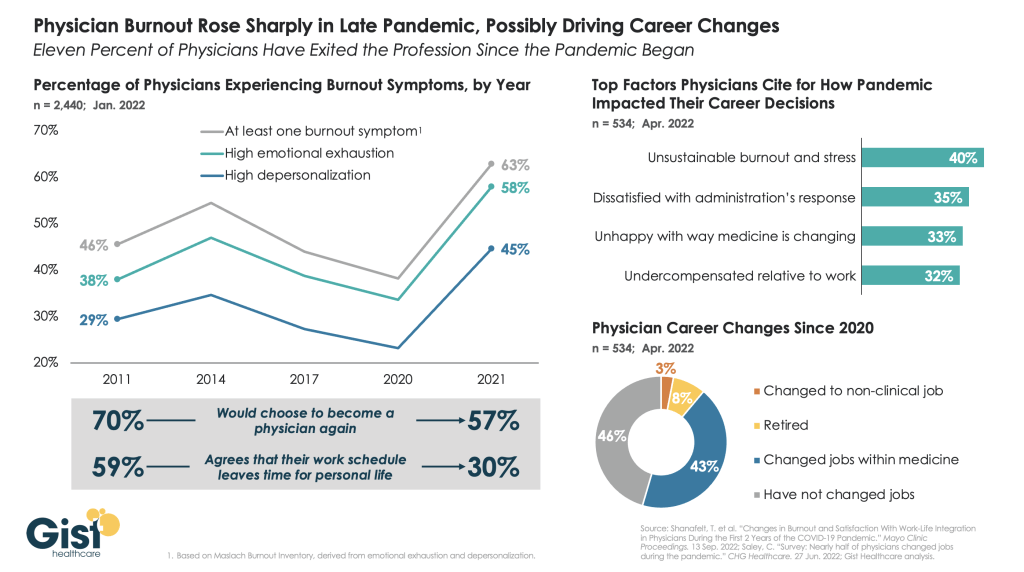
These practices have led some doctors to look for outside investment, namely private equity, to keep their cash flow healthy and their operations functional. The trend of private equity acquisitions of physician practices is worthy of the federal scrutiny it has attracted. Insurers have noticed this trend, too, and appear ready to propose a profitable partnership.
Bloomberg recently reported that CVS/Aetna is looking for a private equity partner to invest in Oak Street Health, the primary care business CVS acquired for $9.5 billion last year. Oak Street is a significant player in primary care delivery, particularly for Americans on Medicare, with more than 100 clinics nationwide. CVS is said to be exploring a joint venture with a private equity firm to significantly expand Oak Street’s footprint and therefore also expand the parent corporation’s direct control over care for millions of seniors and disabled Americans across hundreds of communities.
Republicans have led scrutiny of pharmacy benefit managers on Capitol Hill. And Democratic attacks on private equity in health care have recently intensified. I hope, then, that both parties would find common ground in being watchful of a joint venture between private equity and one of the country’s largest PBMs, Caremark, also owned by CVS/Aetna.
The combination of health insurers and PBMs over the last decade – United Healthcare and Optum; CVS/Aetna and Caremark, and Cigna and Express Scripts – has increasingly handed a few large corporations the ability to approve or deny claims, set payment rates for care, choose what prescriptions to dispense, what prescriptions should cost, and how much patients must pay out-of-pocket for their medications before their coverage kicks in.
As enrollment in Medicare Advantage plans has grown to include a majority of the nation’s elderly and disabled people, we have seen insurers source record profits off the backs of the taxpayer-funded program. But in recent months, insurers have told investors they have had higher than expected Medicare Advantage claims – in particular CVS/Aetna, which took a hammering on Wall Street recently because its Medicare Advantage enrollees were using more health care services than company executives had expected.
It is natural, then, that one of the largest insurer-owned PBMs is looking to expand its hold on primary care for older Americans. Primary care is often the gateway to our health care system, driving referrals to specialists and procedures that lead to the largest claims insurers and their employer customers have to pay. By employing a growing number of primary care providers, CVS/Aetna can increasingly influence referrals to specialists and therefore the care or pharmacy benefit costs those patients may incur.
Control of primary care doctors holds another benefit for insurers: determination of what primary care doctor a patient sees.
People enrolled in an Aetna Medicare Advantage or employer-sponsored plan may find that care is easier to access at Oak Street clinics. Unfortunately, while that feels monopolistic and ethically alarming, this vertical integration has received relatively little scrutiny by lawmakers and regulators.
No law prevents an insurance company or PBM from kicking doctors it does not own out of network while creating preferential treatment for doctors directly employed by or closely affiliated with the corporate mothership.
In fact, the system largely incentivizes this. And shareholders expect insurers to keep up with their peers. As UnitedHealth Group has become increasingly aggressive in its acquisitions of physician practices – now employing or affiliated with about one in ten of the nation’s doctors – it has also become increasingly aggressive in its contract negotiations with physicians it does not control, particularly the specialists who depend on the referrals that come from primary care physicians.
That’s another area where looking to expand Oak Street Health makes smart business sense for CVS/Aetna. Specialist physicians are historically accustomed to higher compensation than primary care doctors and are used to striking hard-fought deals with insurers to stay in-network.
By controlling the flow of primary care referrals to specialists, CVS/Aetna can control what insurers have long-desired greater influence over: patient utilization. As a key driver of referrals to specialists in a specific market, CVS/Aetna will have even more power in contract negotiations with specialists.
As Oak Street’s clinics grow market share in the communities they serve, specialists in that market will feel even more pressured to stay in-network with Aetna and to refer prescriptions to CVS pharmacies. That has the dual benefit for CVS/Aetna of helping to predict what patients will be treated for once they go to a specialist and control over what the insurer will have to pay that specialist.
With different corporate owners, this sort of model could easily run afoul of the federal Anti-Kickback Statute and Stark Law.
No doctor or physician practice is allowed to receive anything of value for the referral of a patient. But that law only applies when there is separate ownership between the referring doctor and the specialist.
CVS/Aetna would clearly be securing value – in the form of lower patient utilization and effective reimbursement rates – under this model. But with Oak Street owned by CVS/Aetna and specialists forced to agree to lower reimbursement rates through negotiations with an insurer that appears separate from Oak Street, there’s no basis for a claim under the Stark Law. There may be antitrust implications, but those are more difficult and take longer to prove – and the fact the federal government cleared CVS/Aetna to acquire Oak Street Health last year wouldn’t help that argument.
This model is already of concern, which is why I continue to urge examination of increasing insurer control of physicians across the country. Their embrace of private equity to accelerate this model is truly alarming. And given Democrats’ recent focus on private equity in health care, they should work with their Republican colleagues who are rightly alarmed about the increasingly anti-competitive, monopolistic health insurance industry.