https://mailchi.mp/3a7244145206/the-weekly-gist-december-9-2022?e=d1e747d2d8
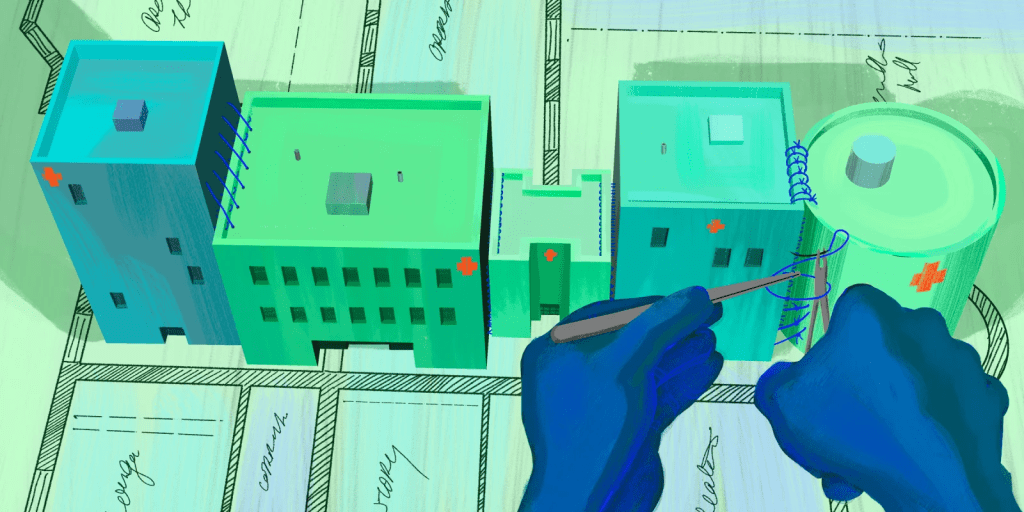
An enlightening piece published this week in Stat News lays out exactly how UnitedHealth Group (UHG) is using its vast network of physicians to generate new streams of profit, a playbook being followed by most other major payers. Already familiar to close observers of the post-Affordable Care Act healthcare landscape, the article highlights how UHG can use “intercompany eliminations”—payments from its UnitedHealthcare payer arm to its Optum provider and pharmacy arms—to achieve profits above the 15 to 20 percent cap placed on health insurance companies.
So far in 2022, 38 percent of UHG’s insurance revenue has flowed into its provider groups, up from 23 percent in 2017. And UHG expects next year’s intercompany eliminations to grow by 20 percent to a total of $130B, which would make up over half of its total projected revenue.
The Gist:
The profit motive behind payer-provider vertical integration is as clear as it is concerning for the state of competition in healthcare.
UHG now employs or affiliates with 70K physicians—10K more than last year—seven percent of the US physician workforce, and the largest of any entity.
Given the weak antitrust framework for regulating vertical integration, the federal government has proven unable to stop the acquisition of providers by payers. Eventually, profit growth for these vertically integrated payers will have to come from tightening provider networks, and not just acquiring more assets. That could prompt regulatory action or consumer backlash, if the government or enrollees determine that access to care is being unfairly restricted.
Until then, the march of consolidation is likely to continue.




