https://mailchi.mp/31b9e4f5100d/the-weekly-gist-june-03-2022?e=d1e747d2d8

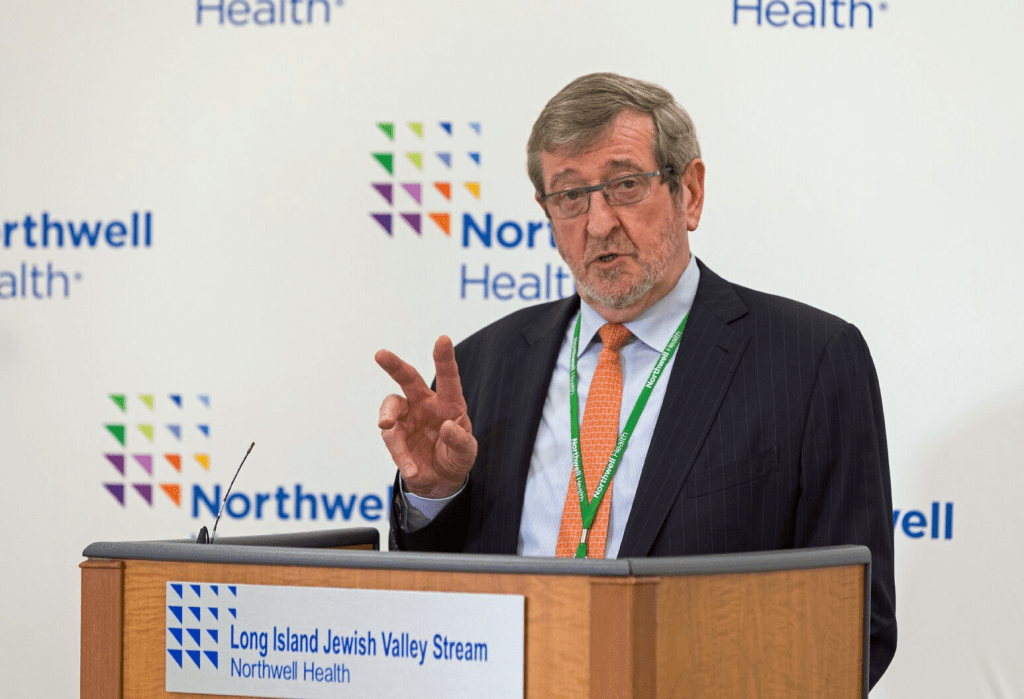
When Congress passed the “No Surprises Act” in 2021, credit rating agencies like Moody’s warned that the bill would hurt physician staffing firms, especially those that provide emergency department (ED) services, which result in a surprise bill in roughly one in five visits. A piece from investigative outlet The Lever highlights how one private equity-backed physician staffing firm, Nashville-based American Physician Partners, is responding to the resultant cash flow challenges by cutting ED physician pay, after already reducing staffing levels. As the article describes, this is possible in an otherwise tight labor market because, unlike many other specialties, there’s an oversupply of ED physicians, due to the rapid growth in emergency medicine residency programs over the last decade.
The Gist: With two-thirds of hospitals outsourcing at least some ED physician labor, the potential insolvency of large physician staffing firms could bring a crisis in access and coverage.
In addition to revenue cuts tied to the surprise billing ban, rising interest rates also mean that PE firms may soon find it more difficult to fund their aggressive growth strategies.
Health systems should proactively evaluate their partnerships with PE-backed physician staffing groups, with an eye toward anticipating potential staffing problems and service quality shortfalls.