With input from stakeholders across the industry, Modern Healthcare outlines six challenges health care is likely to face in 2023—and what leaders can do about them.
1. Financial difficulties
In 2023, health systems will likely continue to face financial difficulties due to ongoing staffing problems, reduced patient volumes, and rising inflation.
According to Tina Wheeler, U.S. health care leader at Deloitte, hospitals can expect wage growth to continue to increase even as they try to contain labor costs. They can also expect expenses, including for supplies and pharmaceuticals, to remain elevated.
Health systems are also no longer able to rely on federal Covid-19 relief funding to offset some of these rising costs. Cuts to Medicare reimbursement rates could also negatively impact revenue.
“You’re going to have all these forces that are counterproductive that you’re going to have to navigate,” Wheeler said.
In addition, Erik Swanson, SVP of data and analytics at Kaufman Hall, said the continued shift to outpatient care will likely affect hospitals’ profit margins.
“The reality is … those sites of care in many cases tend to be lower-cost ways of delivering care, so ultimately it could be beneficial to health systems as a whole, but only for those systems that are able to offer those services and have that footprint,” he said.
2. Health system mergers
Although hospital transactions have slowed in the last few years, market watchers say mergers are expected to rebound as health systems aim to spread their growing expenses over larger organizations and increase their bargaining leverage with insurers.
“There is going to be some organizational soul-searching for some health systems that might force them to affiliate, even though they prefer not to,” said Patrick Cross, a partner at Faegre Drinker Biddle & Reath. “Health systems are soliciting partners, not because they are on the verge of bankruptcy, but because they are looking at their crystal ball and not seeing an easy road ahead.”
Financial challenges may also lead more physician practices to join health systems, private-equity groups, larger practices, or insurance companies.
“Many independent physicians are really struggling with their ability to maintain their independence,” said Joshua Kaye, chair of U.S. health care practice at DLA Piper. “There will be a fair amount of deal activity. The question will be more about the size and specialty of the practices that will be part of the next consolidation wave.”
3. Recruiting and retaining staff
According to data from Fitch Ratings, health care job openings reached an all-time high of 9.2% in September 2022—more than double the average rate of 4.2% between 2010 and 2019. With this trend likely to continue, organizations will need to find effective ways to recruit and retain workers.
Currently, some organizations are upgrading their processes and technology to hire people more quickly. They are also creating service-level agreements between recruiting and hiring teams to ensure interviews are scheduled within 48 hours or decisions are made within 24 hours.
Eric Burch, executive principal of operations and workforce services at Vizient, also predicted that there will be a continued need for contract labors, so health systems will need to consider travel nurses in their staffing plans.
“It’s really important to approach contract labor vendors as a strategic partner,” Burch said. “So when you need the staff, it’s a partnership and they’re able to help you get to your goals, versus suddenly reaching out to them and they don’t know your needs when you’re in crisis.”
When it comes to retention, Tochi Iroku-Malize, president of the American Academy of Family Physicians (AAFP), said health systems are adequately compensated for their work and have enough staff to alleviate potential burnout.
AAFP also supports legislation to streamline prior authorization in the Medicare Advantage program and avoid additional cuts to Medicare payments, which will help physicians provide care to patients with less stress.
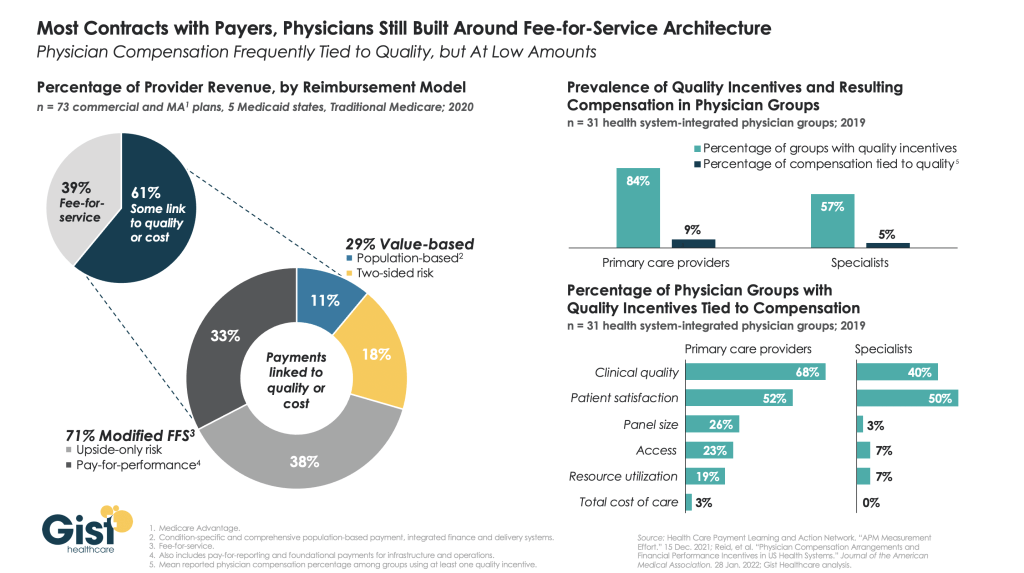
4. Payer-provider contract disputes
A potential recession, along with the ensuing job cuts that typically follow, would limit insurers’ commercial business, which is their most profitable product line. Instead, many people who lose their jobs will likely sign up for Medicaid plans, which is much less profitable.
Because of increased labor, supply, and infrastructure costs, Brad Ellis, senior director at Fitch Ratings, said providers could pressure insurers into increasing the amount they pay for services. This will lead insurers to passing these increased costs onto members’ premiums.
Currently, Ellis said insurers are keeping an eye on how legislators finalize rules to implement the No Surprise Act’s independent resolution process. Regulators will also begin issuing fines for payers who are not in compliance with the law’s price transparency requirement.
5. Investment in digital health
Much like 2022, investment in digital health is likely to remain strong but subdued in 2023.
“You’ll continue to see layoffs, and startup funding is going to be hard to come by,” said Russell Glass, CEO of Headspace Health.
However, investors and health care leaders say they expect a strong market for digital health technology, such as tools for revenue cycle management and hospital-at-home programs.
According to Julian Pham, founding and managing partner at Third Culture Capital, he expects corporations such as CVS Health to continue to invest in health tech companies and for there to be more digital health mergers and acquisitions overall.
In addition, he predicted that investors, pharmaceutical companies, and insurers will show more interest in digital therapeutics, which are software applications prescribed by clinicians.
“As a physician, I’ve always dreamed of a future where I could prescribe an app,” Pham said. “Is it the right time? Time will tell. A lot needs to happen in digital therapeutics and it’s going to be hard.”
6. Health equity efforts
This year, CMS will continue rolling out new health equity initiatives and quality measurements for providers and insurers who serve marketplace, Medicare, and Medicaid beneficiaries. Some new quality measures include maternal health, opioid related adverse events, and social need/risk factor screenings.
CMS, the Joint Commission, and the National Committee for Quality Assurance are also partnering together to establish standards for health equity and data collection.
In addition, HHS is slated to restore a rule under the Affordable Care Act that prohibits discrimination based on a person’s gender identity or sexual orientation. According to experts, this rule may conflict with recently passed state laws that ban gender-affirming care for minors.
“It’s something that’s going to bear out in the courts and will likely lack clarity. We’ll see differences in what different courts decide,” said Lindsey Dawson, associate director of HIV policy and director of LGBTQ health policy at the Kaiser Family Foundation. “The Supreme Court acknowledged that there was this tension. So it’s an important place to watch and understand better moving forward.”