A new perspective on how technology, transformation efforts, and other changes have affected payers, health systems, healthcare services and technology, and pharmacy services.
The acute strain from labor shortages, inflation, and endemic COVID-19 on the healthcare industry’s financial health in 2022 is easing. Much of the improvement is the result of transformation efforts undertaken over the last year or two by healthcare delivery players, with healthcare payers acting more recently. Even so, health-system margins are lagging behind their financial performance relative to prepandemic levels. Skilled nursing and long-term-care profit pools continue to weaken. Eligibility redeterminations in a strong employment economy have hurt payers’ financial performance in the Medicaid segment. But Medicare Advantage and individual segment economics have held up well for payers.
As we look to 2027, the growth of the managed care duals population (individuals who qualify for both Medicaid and Medicare) presents one of the most substantial opportunities for payers. On the healthcare delivery side, financial performance will continue to rebound as transformation efforts, M&A, and revenue diversification bear fruit. Powered by adoption of technology, healthcare services and technology (HST) businesses, particularly those that offer measurable near-term improvements for their customers, will continue to grow, as will pharmacy services players, especially those with a focus on specialty pharmacy.
Below, we provide a perspective on how these changes have affected payers, health systems, healthcare services and technology, and pharmacy services, and what to expect in 2024 and beyond.
The fastest growth in healthcare may occur in several segments
We estimate that healthcare profit pools will grow at a 7 percent CAGR, from $583 billion in 2022 to $819 billion in 2027. Profit pools continued under pressure in 2023 due to high inflation rates and labor shortages; however, we expect a recovery beginning in 2024, spurred by margin and cost optimization and reimbursement-rate increases.
Several segments can expect higher growth in profit pools:
- Within payer, Medicare Advantage, spurred by the rapid increase in the duals population; the group business, due to recovery of margins post-COVID-19 pandemic; and individual
- Within health systems, outpatient care settings such as physician offices and ambulatory surgery centers, driven by site-of-care shifts
- Within HST, the software and platforms businesses (for example, patient engagement and clinical decision support)
- Within pharmacy services, with specialty pharmacy continuing to experience rapid growth
On the other hand, some segments will continue to see slow growth, including general acute care and post-acute care within health systems, and Medicaid within payers (Exhibit 1).
Several factors will likely influence shifts in profit pools. Two of these are:
Change in payer mix. Enrollment in Medicare Advantage, and particularly the duals population, will continue to grow. Medicare Advantage enrollment has grown historically by 9 percent annually from 2019 to 2022; however, we estimate the growth rate will reduce to 5 percent annually from 2022 to 2027, in line with the latest Centers for Medicare & Medicaid Services (CMS) enrollment data.1 Finally, the duals population enrolled in managed care is estimated to grow at more than a 9 percent CAGR from 2022 through 2027.
We also estimate commercial segment profit pools to rebound as EBITDA margins likely return to historical averages by 2027. Growth is likely to be partially offset by enrollment changes in the segment, prompted by a shift from fully insured to self-insured businesses that could accelerate as employers seek to cut costs if the economy slows. Individual segment profit pools are estimated to expand at a 27 percent CAGR from 2022 to 2027 as enrollment rises, propelled by enhanced subsidies, Medicaid redeterminations, and other potential favorable factors (for example, employer conversions through the Individual Coverage Health Reimbursement Arrangement offered by the Affordable Care Act); EBITDA margins are estimated to improve from 2 percent in 2022 to 5 to 7 percent in 2027. On the other hand, Medicaid enrollment could decline by about ten million lives over the next five years based on our estimates, given recent legislation allowing states to begin eligibility redeterminations (which were paused during the federal public health emergency declared at the start of the COVID-19 pandemic2).
Accelerating value-based care (VBC). Based on our estimates, 90 million lives will be in VBC models by 2027, from 43 million in 2022. This expansion will be fueled by an increase in commercial VBC adoption, greater penetration of Medicare Advantage, and the Medicare Shared Savings Program (MSSP) model in Medicare fee-for-service. Also, substantial growth is expected in the specialty VBC model, where penetration in areas like orthopedics and nephrology could more than double in the next five years.
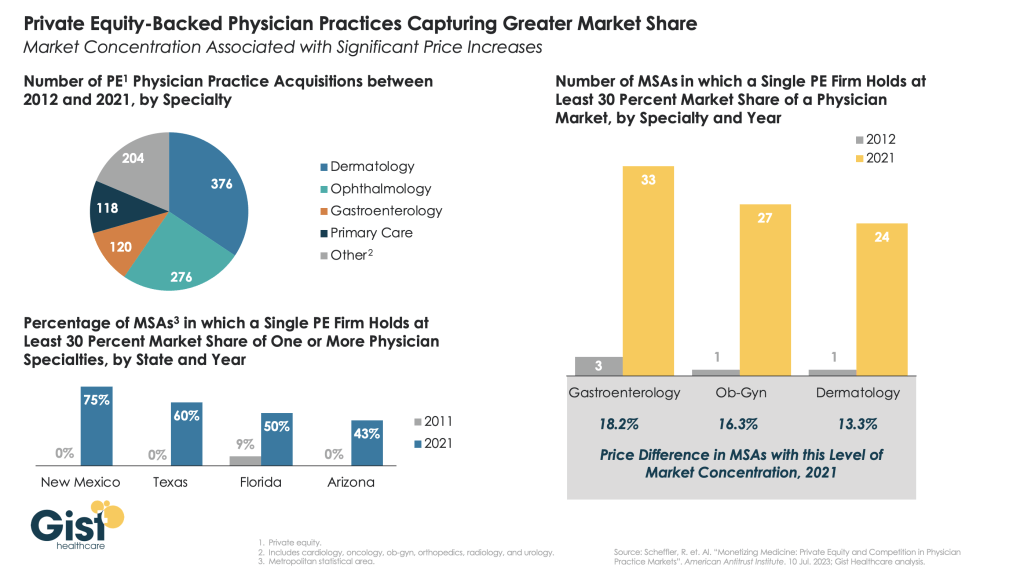
VBC models are undergoing changes as CMS updates its risk adjustment methodology and as models continue to expand beyond primary care to other specialties (for example, nephrology, oncology, and orthopedics). We expect established models that offer improvements in cost and quality to continue to thrive. The transformation of VBC business models in response to pressures from the current changes could likely deliver outsized improvement in cost and quality outcomes. The penetration of VBC business models is likely to lead to shifts in health delivery profit pools, from acute-care settings to other sites of care such as ambulatory surgical centers, physician offices, and home settings.
Payers: Government segments are expected to be 65 percent larger than commercial segments by 2027
In 2022, overall payer profit pools were $60 billion. Looking ahead, we estimate EBITDA to grow to $78 billion by 2027, a 5 percent CAGR, as the market recovers and approaches historical trends. Drivers are likely to be margin recovery of the commercial segment, inflation-driven incremental premium rate rises, and increased participation in managed care by the duals population. This is likely to be partially offset by margin compression in Medicare Advantage due to regulatory pressures (for example, risk adjustment, decline in the Stars bonus, and technical updates) and membership decline in Medicaid resulting from the expiration of the public health emergency.
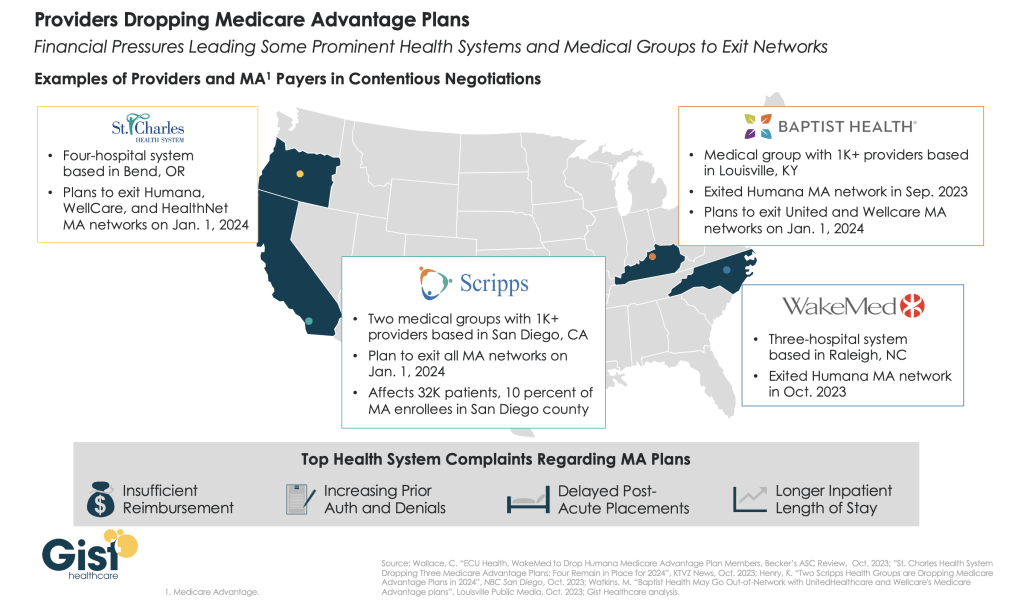
We estimate increased labor costs and administrative expenses to reduce payer EBITDA by about 60 basis points in 2023. In addition, health systems are likely to push for reimbursement rate increases (up to about 350 to 400 basis-point incremental rate increases from 2023 to 2027 for the commercial segment and about 200 to 250 basis points for the government segment), according to McKinsey analysis and interviews with external experts.3
Our estimates also suggest that the mix of payer profit pools is likely to shift further toward the government segment (Exhibit 2). Overall, the profit pools for this segment are estimated to be about 65 percent greater than the commercial segment by 2027 ($36 billion compared with $21 billion). This shift would be a result of increasing Medicare Advantage penetration, estimated to reach 52 percent in 2027, and likely continued growth in the duals segment, expanding EBITDA from $7 billion in 2022 to $12 billion in 2027.
Profit pools for the commercial segment declined from $18 billion in 2019 to $15 billion in 2022. We now estimate the commercial segment’s EBITDA margins to regain historical levels by 2027, and profit pools to reach $21 billion, growing at a 7 percent CAGR from 2022 to 2027. Within this segment, a shift from fully insured to self-insured businesses could accelerate in the event of an economic slowdown, which prompts employers to pay greater attention to costs. The fully insured group enrollment could drop from 50 million in 2022 to 46 million in 2027, while the self-insured segment could increase from 108 million to 113 million during the same period.
Health systems: Transformation efforts help accelerate EBITDA recovery
In 2023, health-system profit pools continued to face substantial pressure due to inflation and labor shortages. Estimated growth was less than 5 percent from 2022 to 2023, remaining below prepandemic levels. Health systems have undertaken major transformation and cost containment efforts, particularly within the labor force, helping EBITDA margins recover by up to 100 basis points; some of this recovery was also volume-driven.
Looking ahead, we estimate an 11 percent CAGR from 2023 to 2027, or total EBITDA of $366 billion by 2027 (Exhibit 3). This reflects a rebound from below the long-term historical average in 2023, spurred by transformation efforts and potentially higher reimbursement rates. We anticipate that health systems will likely seek reimbursement increases in the high single digits or higher upon contract renewals (or more than 300 basis points above previous levels) in response to cost inflation in recent years.
Measures to tackle rising costs include improving labor productivity and the application of technological innovation across both administration and care delivery workflows (for example, further process standardization and outsourcing, increased use of digital care, and early adoption of AI within administrative workflows such as revenue cycle management). Despite these measures, 2027 industry EBITDA margins are estimated to be 50 to 100 basis points lower than in 2019, unless there is material acceleration in performance transformation efforts.
There are some meaningful exceptions to this overall outlook for health systems. Although post-acute-care profit pools could be severely affected by labor shortages (particularly nurses), other sites of care might grow (for example, non-acute and outpatient sites such as physician offices and ambulatory surgery centers). We expect accelerated adoption of VBC to drive growth.
HST profit pools will grow in technology-based segments
HST is estimated to be the fastest-growing sector in healthcare. In 2021, we estimated HST profit pools to be $51 billion. In 2022, according to our estimates, the HST profit pool shrank to $49 billion, reflecting a contracting market, wage inflation pressure, and the drag of fixed-technology investment that had not yet fulfilled its potential. Looking ahead, we estimate a 12 percent CAGR in 2022–27 due to the long-term underlying growth trend and rebound from the pandemic-related decline (Exhibit 4). With the continuing technology adoption in healthcare, the greatest acceleration is likely to happen in software and platforms as well as data and analytics, with 15 percent and 22 percent CAGRs, respectively.
In 2023, we observed an initial recovery in the HST market, supported by lower HST wage pressure and continued adoption of technology by payers and health systems searching for ways to become more efficient (for example, through automation and outsourcing).
Three factors account for the anticipated recovery and growth in HST. First, we expect continued demand from payers and health systems searching to improve efficiency, address labor challenges, and implement new technologies (for example, generative AI). Second, payers and health systems are likely to accept vendor price increases for solutions delivering measurable improvements. Third, we expect HST companies to make operational changes that will improve HST efficiency through better technology deployment and automation across services.
Pharmacy services will continue to grow
The pharmacy market has undergone major changes in recent years, including the impact of the COVID-19 pandemic, the establishment of partnerships across the value chain, and an evolving regulatory environment. Total pharmacy dispensing revenue continues to increase, growing by 9 percent to $550 billion in 2022,4 with projections of a 5 percent CAGR, reaching $700 billion in 2027.5 Specialty pharmacy is one of the fastest growing subsegments within pharmacy services and accounts for 40 percent of prescription revenue6; this subsegment is expected to reach nearly 50 percent of prescription revenue in 2027 (Exhibit 5). We attribute its 8 percent CAGR in revenue growth to increases in utilization and pricing as well as the continued expansion of pipeline therapies (for example, cell and gene therapies and oncology and rare disease therapies) and expect that the revenue growth will be partially offset by reimbursement pressures, specialty generics, and increased adoption of biosimilars. Specialty pharmacy dispensers are also facing an evolving landscape with increased manufacturer contract pharmacy pressures related to the 340B Drug Pricing Program. With restrictions related to size and location of contract pharmacies that covered entities can use, the specialty pharmacy subsegment has seen accelerated investment in hospital-owned pharmacies.
Retail and mail pharmacies continue to face margin pressure and a contraction of profit pools due to reimbursement pressure, labor shortages, inflation, and a plateauing of generic dispensing rates.7 Many chains have recently announced8 efforts to rationalize store footprints while continuing to augment additional services, including the provision of healthcare services.
Over the past year, there has also been increased attention to broad-population drugs such as GLP-1s (indicated for diabetes and obesity). The number of patients meeting clinical eligibility criteria for these drugs is among the largest of any new drug class in the past 20 to 30 years. The increased focus on these drugs has amplified conversations about care and coverage decisions, including considerations around demonstrated adherence to therapy, utilization management measures, and prescriber access points (for example, digital and telehealth services). As we look ahead, patient affordability, cost containment, and predictability of spending will likely remain key themes in the sector. The Inflation Reduction Act is poised to change the Medicare prescription Part D benefit, with a focus on reducing beneficiary out-of-pocket spending, negotiating prices for select drugs, and incentivizing better management of high-cost drugs. These changes, coupled with increased attention to broad-population drugs and the potential of high-cost therapies (such as cell and gene therapies), have set the stage for a shift in care and financing models.
The US healthcare industry faced demanding conditions in 2023, including continuing high inflation rates, labor shortages, and endemic COVID-19. However, the industry has adapted. We expect accelerated improvement efforts to help the industry address its challenges in 2024 and beyond, leading to an eventual return to historical-average profit margins.