July 2025 will be the month U.S. healthcare leaders recognize as the industry’s modern turning point. Consider…
- On July 4, the One Big Beautiful Bill Act was signed into law setting in motion $960 billion in Medicaid cuts over the decade and massive uncertainty among those most adversely impacted—low income and under-served populations dependent on public programs, 8 to 11 million who used now-suspended marketplace subsidies to buy insurance coverage, and hundreds of state and local health agencies left in funding limbo.
- On July 15, the Bureau of Labor Statistics reported the June Consumer Price Index rose .3% bumping the LTM to 2.7% (lower than LTM of 3.4% for medical services). Prices have edged up.
- On July 31, President Trump issued an Executive Order to 17 drug companies ordering them to reduce prices on their drugs by September 29 or else. And CMS issued final rules for FY2026 Medicare payments to hospitals, rehab and other providers reflecting increases ranging from 2.5-3.3% effective October 1.
- And on the same day, the Bureau of Labor issued its July 2025 jobs report that showed a disappointing net gain of 73,000 jobs plus downward revisions for May and June of 258,000 sparking Wall Street anxiety and President Trump to call the results “rigged” before firing BLS head Erika McEntarfer. Note: healthcare added 55,000 in July—the biggest of any sector and more than its 42,000 average monthly increase.
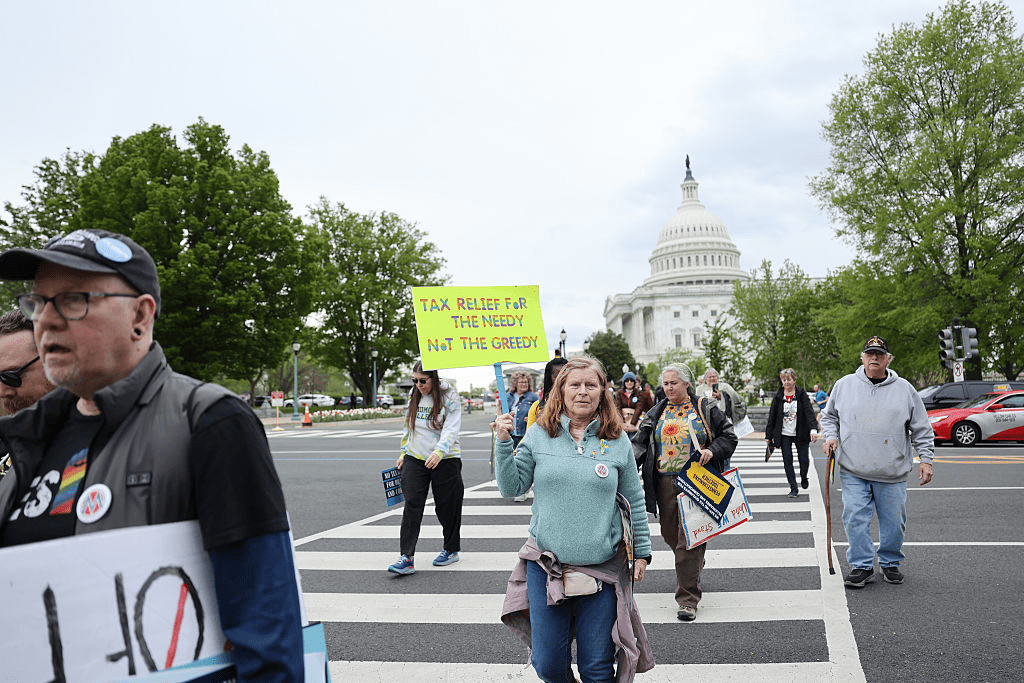
Collectively, these actions reflect rejection of the health industry by the GOP-led Congress.
It follows 15 years of support vis a vis the Affordable Care Act (2010) and pandemic recovery emergency funding (2020-2021). In that 15-year period, the bigger players got bigger in each sector, investment of private equity in each sector became more prevalent, costs increased, affordability for consumers and employers decreased, and the public’s overall satisfaction with the health system declined precipitously.
For the four major players in the system, the passage of the “big, beautiful bill” was a disappointment. Their primary concerns were not addressed:
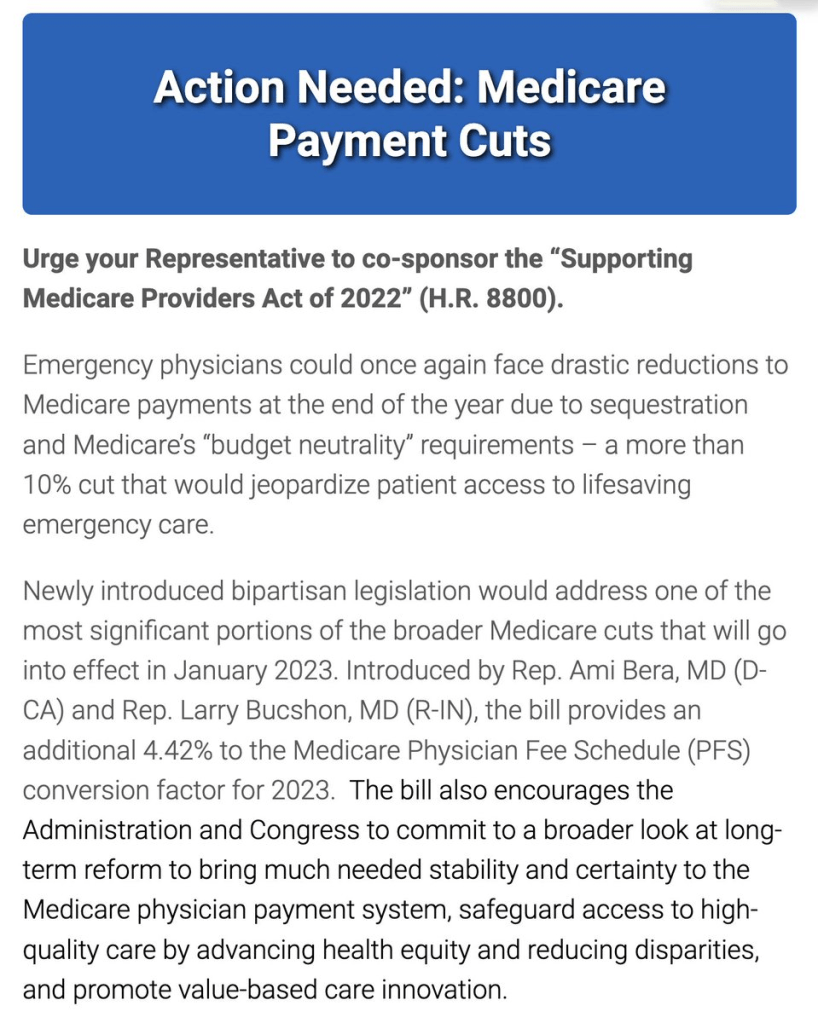
- Physicians wanted relief from annual payment cuts by Medicare preferring reimbursement tied directly to medical inflation. And insurer’ prior authorization and provider reimbursement was a top issue. Status: Not much has changed though adjustments are promised.
- Hospitals wanted continuation of federal Medicaid funding, protection of the 340B drug purchasing program, rejection of site-neutral payment policies, higher Medicare reimbursement and relief from insurer prior authorization frustrations. Status: Medicaid funding is being cut forcing the issue for states. CMS payment increases for 2026 are lower than operating cost increases. Insurers have promised prior-auth relief but details about how and when are unknown. And Congress posture toward hospitals seems harsh: price transparency compliance, safety event reporting, and cost concerns are bipartisan issues.
- Insurers wanted sustained funding for state Medicaid and Medicare Advantage programs and federal pushback against drug prices and hospital consolidation. Status: Congress appears sympathetic to enrollee complaints and anxious to address insurer “waste, fraud and abuse” including overpayments in Medicare Advantage.
- Drug companies oppose “Most Favored Nation” pricing and want protections of their patents and limits on how much insurers, pharmacy benefits managers, wholesalers, online distributors and other “middlemen” earn at their expense. Status: to date, little action despite sympathetic rhetoric by lawmakers. Status: to date, Congress has taken nominal action beyond the Inflation Reduction Act (2022) though 23 states have passed legislation requiring PBMs, insurers and manufacturers to disclose drug prices and 12 states have established Prescription Drug Affordability Boards to monitor prices.
My take:
The landscape for U.S. healthcare is fundamentally changed as a result of the July actions noted above. It is compounded by public anxiety about the economy at home and global tensions abroad.
These July actions were a turning point for the industry: responding appropriately will require fresh ideas and statesmanship. Transparency about prices, costs, incentives and performance is table stakes. Leaders dedicated to the greater good will be the difference.