https://www.pwc.com/us/Biden2020healthagenda

President-elect Joe Biden’s healthcare agenda: building on the ACA, value-based care, and bringing down drug prices.
In many ways, Joe Biden is promising a return to the Obama administration’s approach to healthcare:
- Building on the Affordable Care Act (ACA) through incremental expansions in government-subsidized coverage
- Continuing CMS’ progress toward value-based care
- Bringing down drug prices
- Supporting modernization of the FDA
Bolder ideas, such as developing a public option, resolving “surprise billing,” allowing for negotiation of drug prices by Medicare, handing power to a third party to help set prices for some life sciences products, and raising the corporate tax rate, could be more challenging to achieve without overwhelming majorities in both the House and the Senate.
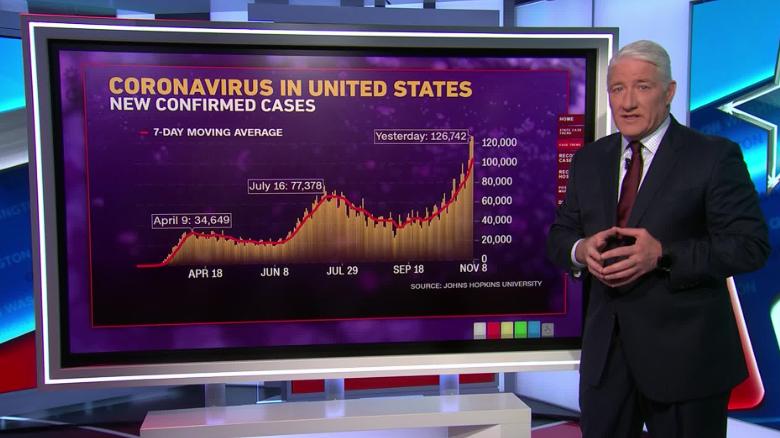
Biden is likely to mount an intensified federal response to the COVID-19 pandemic, enlisting the Defense Production Act to compel companies to produce large quantities of tests and personal protective equipment as well as supporting ongoing deregulation around telehealth. The Biden administration also will likely return to global partnerships and groups such as the World Health Organization, especially in the area of vaccine development, production and distribution.
What can health industry executives expect from Biden’s healthcare proposals?
Broadly, healthcare executives can expect an administration with an expansionary agenda, looking to patch gaps in coverage for Americans, scrutinize proposed healthcare mergers and acquisitions more aggressively and use more of the government’s power to address the pandemic. Executives also can expect, in the event the ACA is struck down, moves by the Biden administration and Democratic lawmakers to develop a replacement. Healthcare executives should scenario plan for this unlikely yet potentially highly disruptive event, and plan for an administration marked by more certainty and continuity with the Obama years.
All healthcare organizations should prepare for the possibility that millions more Americans could gain insurance under Biden. His proposals, if enacted, would mean coverage for 97% of Americans, according to his campaign website. This could mean millions of new ACA customers for payers selling plans on the exchanges, millions of new Medicaid beneficiaries for managed care organizations, millions of newly insured patients for providers, and millions of covered customers for pharmaceutical and life sciences companies. The surge in insured consumers could mirror the swift uptake in the years following the passage of the ACA.
Biden’s plan to address the COVID-19 pandemic
Biden is expected to draw on his experience from H1N1 and the Ebola outbreaks to address the COVID-19 pandemic with a more active role for the federal government, which many Americans support. These actions could shore up the nation’s response in which the federal government largely served in a support role to local, state and private efforts.
Three notable exceptions have been the substantial federal funding for development of vaccines against the SARS-CoV-2 virus, Congress’ aid packages and the rapid deregulatory actions taken by the FDA and CMS to clear a path for medical products to be enlisted for the pandemic and for providers, in particular, to be able to respond to it.
Implications of Biden’s 2020 health agenda on healthcare payers, providers and pharmaceutical and life sciences companies
The US health system has been slowly transforming for years into a New Health Economy that is more consumer-oriented, digital, virtual, open to new players from outside the industry and focused on wellness and prevention. The COVID-19 pandemic has accelerated some of those trends. Once the dust from the election settles, companies that have invested in capabilities for growth and are moving forcefully toward the New Health Economy stand to gain disproportionately.
Shortages of clinicians and foreign medical students may continue to be an issue for a while
The Trump administration made limiting the flow of immigrants to the US a priority. The associated policy changes have the potential to exacerbate shortages of physicians, nurses and other healthcare workers, including medical students. These consequences have been aggravated by the pandemic, which dramatically curtailed travel into the US.
- Healthcare organizations, especially rural ones heavily dependent on foreign-born employees, may find themselves competing fiercely for workers, paying higher salaries and having to rethink the structure of their workforces.
- Providers should consider reengineering primary care teams to reflect the patients’ health status and preferences, along with the realities of the workforce on the ground and new opportunities in remote care.
Focus on modernizing the supply chain
Biden and lawmakers from both parties have been raising questions about life sciences’ supply chains. This focus has only intensified because of the pandemic and resulting shortages of personal protective equipment (PPE), pharmaceuticals, diagnostic tests and other medical products.
- Investment in advanced analytics and cybersecurity could allow manufacturers to avoid disruptive stockouts and shortages, and deliver on the promise of the right treatment to the right patient at the right time in the right place.
Drug pricing needs a long-term strategy
Presidents and lawmakers have been talking about drug prices for decades; few truly meaningful actions have been implemented. Biden has made drug pricing reform a priority.
- Drug manufacturers may need to start looking past the next quarter to create a new pricing strategy that maximizes access in local markets through the use of data and analytics to engage in more value-based pricing arrangements.
- New financing models may help patients get access to drugs, such as subscription models that provide unlimited access to a therapy at a flat rate.
- Companies that prepare now to establish performance metrics and data analytics tools to track patient outcomes will be well prepared to offer payers more sustainable payment models, such as mortgage or payment over time contracts, avoiding the sticker shock that comes with these treatments and improving uptake at launch.
- Pharmaceutical and life sciences companies will likely have to continue to offer tools for consumers like co-pay calculators and use the contracting process where possible to minimize out-of-pocket costs, which can improve adherence rates and health outcomes.
View interoperability as an opportunity to embrace, not a threat to avoid or ignore
While the pandemic delayed many of the federal interoperability rule deadlines, payers and providers should use the extra time to plan strategically for an interoperable future.
- Payers should review business partnerships in this new regulatory environment.
- Digital health companies and new entrants may help organizations take advantage of the opportunities that achieving interoperability may present.
- Companies should consider the legal risks and take steps to protect their reputations and relationships with customers by thinking through issues of consent and data privacy.
Health organizations should review their policies and consider whether they offer protections for customers under the new processes and what data security risks may emerge. They should also consider whether business associate agreements are due in more situations.
Plan for revitalized ACA exchanges and a booming Medicare Advantage market
The pandemic has thrown millions out of work, generating many new customers for ACA plans just as the incoming Biden administration plans to enrich subsidies, making more generous plans within reach of more Americans.
- Payers in this market should consider how and where to expand their membership and appeal to those newly eligible for Medicare. Payers not in this market should consider partnerships or acquisitions as a quick way to enter the market, with the creation of a new Medicare Advantage plan as a slower but possibly less capital-intensive entry into this market.
- Payers and health systems should use this opportunity to design more tailored plan options and consumer experiences to enhance margins and improve health outcomes.
- Payers with cash from deferred care and low utilization due to the pandemic could turn to vertical integration with providers as a means of investing that cash in a manner that helps struggling providers in the short term while positioning payers to improve care and reduce its cost in the long term.
- Under the Trump administration, the FDA has approved historic numbers of generic drugs, with the aim of making more affordable pharmaceuticals available to consumers. Despite increased FDA generics approvals, generics dispensed remain high but flat, according to HRI analysis of FDA data.
- Pharmaceutical company stocks, on average, have climbed under the Trump administration, with a few notable dips due to presidential speeches criticizing the industry and the pandemic.
- Providers have faced some revenue cuts, particularly in the 340B program, and many entered the pandemic in a relatively weak liquidity position. The pandemic has led to layoffs, pay cuts and even closures. HRI expects consolidation as the pandemic continues to curb the flow of patients seeking care in emergency departments, orthopedic surgeons’ offices, dermatology suites and more.
Lawmakers and politicians often use bold language, and propose bold solutions to problems, but the government and the industry itself resists sudden, dramatic change, even in the face of sudden, dramatic events such as a global pandemic. One notable exception to this would be a decision by the US Supreme Court to strike down the ACA, an event that would generate a great deal of uncertainty and disruption for Americans, the US health industry and employers.