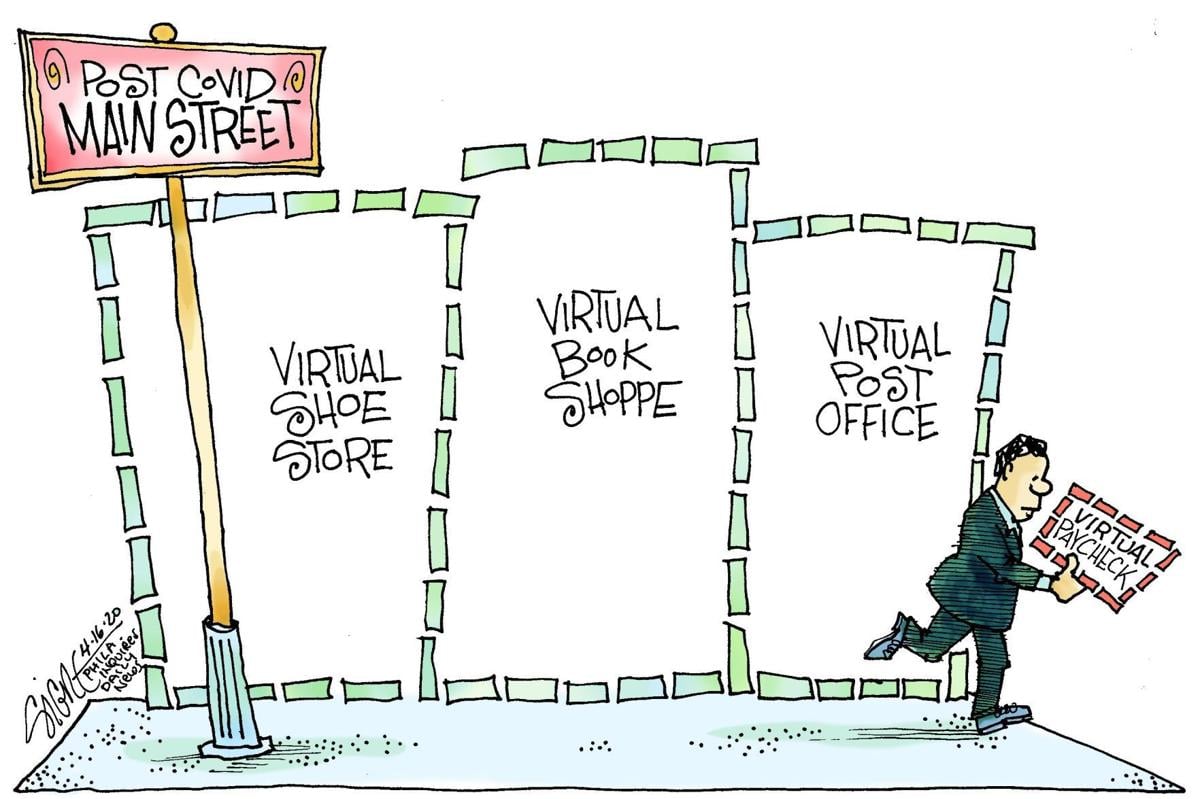
Cartoon – Making Room for New Hires

Advocate Aurora Health is implementing a new work model that will move 12,000 non-clinical employee positions in finance, consumer experience and more departments to remote-first operations, according to a May 21 BizTimes report.
Under the new work model, dubbed WorkForward, the 12,000 non-clinical employees who have been working remotely throughout the COVID-19 pandemic will continue to do so permanently; these employees will “no longer have dedicated workspaces” like cubicles or offices at the health system’s Milwaukee and Downers Grove, Ill.-based offices, the publication reports.
Affected departments include finance and accounting, consumer experience and public affairs, strategy and business development, government relations and administration. Employees will be able to choose to work from home, at a coffee shop or other locations, Advocate Aurora Chief Human Resources Officer Kevin Brady told BizTimes.
“For some departments, remote-first may come to mean monthly team meetings in the office, once-a-week collaboration sessions or a trip to an outside-the-box location that inspires the team,” he said.
Advocate Aurora will “regularly evaluate” its real estate needs with the work model transition; the health system recently vacated non-headquarters office space when its lease ended at the end of 2020. Advocate Aurora is also reconfiguring its remaining facilities to create more “innovative and productive” work areas that employees can use for meetings or temporary office space, according to the report.
Some teachers don’t want to return to the classroom until they’ve been vaccinated — setting up potential clashes with state and local governments pushing to reopen schools.
Why it matters: Extended virtual learning is taking a toll on kids, and the Biden administration is pushing to get them back in the classroom quickly. But that will only be feasible if teachers are on board.
Where it stands: Although the rise of new, more contagious variants has scrambled the calculus on school reopening, for now the expert consensus is that vaccinations aren’t essential to safely reopening schools.
Yes, but: Teachers in some large school districts don’t want to return to the classroom without being vaccinated — which could mean several more months of virtual classes.
What they’re saying: “The issue is that we should be aligning vaccination with school opening. That doesn’t mean every single teacher has to be vaccinated before you open one school, it means there has to be that alignment,” Randi Weingarten, the president of the American Federation of Teachers, told ABC News.
The other side: Ohio Gov. Mike DeWine has said school staff will be prioritized for vaccination, with the goal of having students return to classrooms by March 1.
The bottom line: “It’s challenging to make those decisions about how to prioritize different populations, all of whom are at significant risk,” the Kaiser Family Foundation’s Jennifer Tolbert said.
Go deeper: Schools face an uphill battle to reopen during the pandemic


Hardly one month into 2021, the pressing priorities facing healthcare leaders are abundantly clear.
First, we will be living in a world preoccupied by COVID-19 and vaccination for many months to come. Remember: this is a marathon, not a sprint. And the stark reality is that the vaccination rollout will continue well into the summer, if not longer, while at the same time we continue to care for hundreds of thousands of Americans sickened by the virus. Despite the challenges we face now and in the coming months in treating the disease and vaccinating a U.S. population of 330 million, none of us should doubt that we will prevail. Despite the federal government’s missteps over the past year in managing and responding to this unprecedented public health crisis, historians will recognize the critical role of the nation’s healthcare community in enabling us to conquer this once-in-a-generation pandemic.
While there has been an overwhelming public demand for the vaccine during the past couple of weeks, there remains some skepticism within the communities we serve, including some of the most-vulnerable populations, so healthcare leaders will find themselves spending time and energy communicating the safety and efficacy of vaccines to those who may be hesitant. This is a good thing. It is our responsibility to share facts, further public education and influence public policy. COVID-19 has enhanced public trust in healthcare professionals, and we can maintain that trust if we keep our focus on the right things — namely, how we improve the health of our communities.
And as healthcare leaders diligently balance this work, we also have a great opportunity to reimagine what our hospitals and health systems can be as we emerge from the most trying year of our professional lifetimes. How do you want your hospital or system organized? What kind of structural changes are needed to achieve the desired results? What do you really want to focus on? Amid the pressing priorities and urgent decision-making needed to survive, it is easy to overlook the great reimagination period in front of us. The key is to forget what we were like before COVID-19 and reflect upon what we want to be after.
These changes won’t occur overnight. We’ll need patience, but here are my thoughts on five key questions we need to answer to get the right results.
1. How do you enhance productivity and become more efficient? Throughout 2021, most systems will be in recovery mode from COVID’s financial bruises. Hospitals saw double-digit declines in inpatient and outpatient volumes in 2020, and total losses for hospitals and health systems nationwide were estimated to total at least $323 billion. While federal relief offset some of our losses, most of us still took a major financial hit. As we move forward, we must reorganize to operate as efficiently as possible. Does reorganization sound daunting? If so, remember the amount of reorganization we mustered to work effectively in the early days of the pandemic. When faced with no alternative, healthcare moved heaven and earth to fulfill its mission. Crises bring with them great clarity. It’s up to leaders to keep that clarity as this tragic, exhausting and frustrating crisis gradually fades.
2. How do you accelerate digital care? COVID-19 changed our relationship with technology, personally and professionally. Look at what we accomplished and how connected we remain. We were reminded of how high-quality healthcare can go unhindered by distance, commutes and travel constraints with the right technology and telehealth programs in place. Health system leaders must decide how much of their business can be accommodated through virtual care so their organizations can best offer convenience while increasing access. Oftentimes, these conversations don’t get far before confronting doubts about reimbursement. Remember, policy change must happen before reimbursement catches up. If you wait for reimbursement before implementing progressive telehealth initiatives, you’ll fall behind.
3. How will your organization confront healthcare inequities? In 2020, I pledged that Northwell would redouble its efforts and remain a leader in diversity and inclusion. I am taking this commitment further this year and, with the strength of our diverse workforce, will address healthcare inequities in our surrounding communities head-on. This requires new partnerships, operational changes and renewed commitments from our workforce. We need to look upstream and strengthen our reach into communities that have disparate access to healthcare, education and resources. We must push harder to transcend language barriers, and we need our physicians and medical professionals of color reinforcing key healthcare messages to the diverse communities we serve. COVID-19’s devastating effect on communities of color laid bare long-standing healthcare inequalities. They are no longer an ugly backdrop of American healthcare, but the central plot point that we can change. If more equitable healthcare is not a top priority, you may want to reconsider your mission. We need leaders whose vision, commitment and courage match this moment and the unmistakable challenge in front of us.
4. How will you accommodate the growing portion of your workforce that will be remote? Ten to 15 percent of Northwell’s workforce will continue to work remotely this year. In the past, some managers may have correlated remote work and teams with a decline in productivity. The past year defied that assumption. Leaders now face decisions about what groups can function remotely, what groups must return on-site, and how those who continue to work from afar are overseen and managed. These decisions will affect your organizations’ culture, communications, real estate strategy and more.
5. How do you vigorously hold onto your cultural values amid all of this change? This will remain a test through 2021 and beyond. Culture is the personality of your organization. Like many health systems and hospitals, much of Northwell’s culture of connectedness, awareness, respect and empathy was built through face-to-face interaction and relationships where we continually reinforced the organization’s mission, vision and values. With so many employees now working remotely, how can we continue to bring out the best in all of our people? We will work to answer that question every day. The work you put in to restore, strengthen and revitalize your culture this year will go a long way toward cementing how your employees, patients and community come to see your organization for years to come. Don’t underestimate the power of these seemingly simple decisions.
While we’ve been through hell and back over the past year, I’m convinced that the healthcare community can continue to strengthen the public trust and admiration we’ve built during this pandemic. However, as we slowly round the corner on COVID-19, our future success will hinge on what we as healthcare organizations do now to confront the questions above and others head-on. It won’t be quick or easy and progress will be a jagged line. Let’s resist the temptation to return to what healthcare was and instead work toward building what healthcare can be. After the crisis of a lifetime, here’s our opportunity of a lifetime. We can all be part of it.
https://mailchi.mp/e38b070b8787/the-weekly-gist-december-18-2020?e=d1e747d2d8

It turns out it’s not just the kids who aren’t getting snow days this year. This week, we spoke with an executive at a health system hit hard by Wednesday’s Nor’easter, and asked how the system was faring with the expected 18 inches of snowfall. He replied that the medical group was as busy as usual.
With all the work this spring to expand telemedicine capabilities, clinic staff were able to reach out to patients the day before the storm, and proactively convert a majority of scheduled in-person clinic visits to telemedicine. “Normally we would’ve been closed, and most appointments rescheduled for weeks down the road,” he told us. Instead, they were able to keep most of those visits in their scheduled time slot.
“Now that we have a systemwide process for telemedicine, I don’t think we’ll have a reason for the clinic to take a snow day again.” It’s a clear win-win for the system and patients: patient care seamlessly goes on. It’s easy to see the many use cases for the ability to toggle between in-person and virtual visits. A parent is stuck at home with a sick kid, and can’t make her endocrinologist appointment? Moved to virtual! A patient has an unexpected business trip taking him out of town? Don’t cancel, let’s do that follow-up visit via telemedicine.
We’ve been worried about the slowdown in progress made on telemedicine as patients switched back to in-person visits across the summer and fall. The ability to continue patient care during a record-breaking snowstorm is a perfect illustration of why it’s critical not to “backslide” with virtual care: meeting patients where they are, regardless of circumstances, is an essential part of building long-term loyalty and care continuity.

The pandemic put nurses on the front lines of the battle against COVID-19 and caused shifts in the way they provide care.
During this year, nurses have adapted to increased adoption of telehealth and virtual patient monitoring, as well as constantly evolving staffing needs.
These factors — and others, such as the physical and emotional conditions nurses have faced due to the public health crisis — are sure to affect nursing in the years to come. Here, 10 healthcare executives and leaders share their predictions for nursing in the next five years.
Editor’s note: Responses were edited lightly for length and clarity.
Beverly Bokovitz, DNP, RN. Vice President and Chief Nurse Executive of UC Health (Cincinnati): In the next five years, as we continue to encounter a national nursing shortage, I expect to see additional innovative strategies to complement the care provided at the bedside.
One of these strategies will be some type of robot-assisted care. From delivery of medications to answering call lights — and completing simple tasks like needing a blanket or requesting that the heat be adjusted — we will see more electronic solutions. These solutions will allow for a better patient experience and help to exceed the expectations of our patients as customers.
Of course, nothing can take the place of skilled and compassionate bedside care, but many tasks could be automated — and will be — to supplement the professional nursing shortage.
Natalia Cineas, DNP, RN. Senior Vice President and Chief Nurse Executive of NYC Health + Hospitals (New York City): Nurses will continue to play a vital role in addressing the health inequities and social determinants of health among vulnerable populations as the nursing workforce itself becomes more diverse and inclusive. As the largest segment of the healthcare workforce — with some 4 million nurses active in the U.S. — nurses represent the faces of the communities in which they serve. As America becomes a more diverse and inclusive society, so too will the nursing profession become more diverse and inclusive. Currently, industry estimates indicate that between one quarter to one-third of all U.S. nurses identify as a member of a minority group, with between 19 percent and 24 percent of U.S. nurses identifying themselves as Black/African-American; 5 percent to 9 percent identifying themselves as Hispanic; and about 3 percent identifying themselves as Asian. The percentage of minority nurses has been rising steadily for the past two decades and is expected to continue to climb in the coming years.
Blacks and underserved minority populations face numerous genetic, environmental, cultural and socioeconomic factors that account for health disparities, and the impact is particularly visible in the areas of cardiovascular disease, diabetes, pregnancy and childbirth mortality, and cancer outcomes, as well as the enormous toll of the current novel coronavirus global pandemic, where communities of color have been among the hardest hit populations.
In New York City alone, statistics compiled by the city’s health department show Blacks and Hispanics together account for 65 percent of all COVID-19 cases; represented 70 percent of all hospitalizations due to COVID-19; and, sadly, 68 percent of all deaths caused by COVID-19. As demonstrated during this pandemic, in the future, technology such as telehealth and virtual patient monitoring will play a major role in the care of patients. There will be a vast need to address social determinants of health by educating and providing resources to allow utilization of this technology such as using “wearable tech” to monitor ongoing health issues, such as high blood pressure, diabetes, heart conditions and other chronic illnesses.
Ryannon Frederick, MSN, RN. Chief Nursing Officer of Mayo Clinic (Rochester, Minn.): Nursing research will experience extraordinary demand and growth driven by a realization that both complex and unmet patient needs can often be best served by the role of a professional registered nurse. Nurses are uniquely positioned to implement symptom and self-management interventions for patients and their caregivers. Significant disruption in healthcare, including increasing use of technology, will lead to a dramatic shift to understand the role of the RN in improving patient outcomes and implementing interventions using novel approaches. Nursing researchers will provide a scientific body of evidence proving equivalent, if not better, patient care outcomes that can be obtained at a lower cost than traditional models, leading to an even greater demand for the role of the professional nurse in patient care.
Karen Higdon, DNP, RN, Vice President and Chief Nursing Officer of Baptist Health Louisville (Ky.): The value of nursing has never been more apparent. Nurses have led the front line during this pandemic. In the next five years, we must be flexible and creative in establishing new models of care, specifically around roles that support nursing, such as assistant and tech roles. Creating roles with clear role definition, that are attractive and meaningful for nursing support will help build consistent, high-quality models for nursing to lead. This consistency, along with IT capabilities that enhance workflow, will better allow nurses to work at the top of their scope.
Karen Hill, DNP, RN. COO and Chief Nursing Officer of Baptist Health Lexington (Ky.): 2020 was declared the “Year of the Nurse” and this reality has never been more true than realizing the personal and professional sacrifices of nurses in dealing with issues surrounding the pandemic. The next five years will require nursing professionals to be flexible to address new, unknown emerging issues in all settings, to be open to new opportunities for leadership in hospitals, schools and communities and to use technology and telehealth to provide safer care to patients. Nurses need to evaluate our practices and traditions that are value-added and leave behind the task orientation of the past. We need to honor our legacy and create our path.
Therese Hudson-Jinks, MSN, RN. Chief Nursing Officer and Chief Patient Experience Officer at Tufts Medical Center and Tufts Children’s Hospital (Boston): Over the next five years, I expect that the support and retention of clinical nurses will become the top priority of every CNO and executive team, given nurses’ direct impact on supporting the business of healthcare. This will be particularly critical because there will be a concerning shortage of experienced clinical nurses as a result of advancing technologies increasing complexity in care, additional nurse roles created outside traditional areas, fierce competition for talent between large healthcare systems, aging baby boom workforce retiring at higher rates year over year, and a lack of sufficient numbers of PhD-prepared nurses working in academia and supporting higher enrollments.
I also believe that CNOs will be laser-focused on creating the practice environment that enhances retention of top, talented clinical nurses, and we will put a greater emphasis on the influence of effective nursing leadership in reaching that goal. In addition, I fully expect that nurses will be seen more as individuals with talents and experience than ever before — not just a number on a team, but rather a professional with specific, unique, talents that are highly sought after in competitive markets.
Finally, I anticipate that nursing innovation will blossom, given the exposure of the “innovation/solutionist superpower” within nurses during the pandemic. Philanthropy will grow exponentially in support of nursing innovation as a result.
Carol Koeppel-Olsen, MSN, RN. Vice President of Patient Care Services at Abbott Northwestern Hospital (Minneapolis): During the COVID-19 pandemic nurses have been working in difficult physical and emotional conditions, which may lead to significant turnover after the pandemic resolves. Nurses have a commitment to serving others and will persevere until the crisis is past; however, when conditions improve, many nurses may decide to pursue careers outside acute care settings. A possible turnover, coupled with a service economy that has been devastated, may result in large numbers of former service workers seeking stable jobs in nursing. Hospitals will have to be nimble and creative to onboard an influx of new nurses that are not only new to the profession but new to healthcare. Tactics to onboard these new nurses may include the use of retired RNs as mentors, instructor-model clinical groups in the work setting, job shadowing and aptitude testing to determine the best clinical fit.
Jacalyn Liebowitz, DNP, RN. Senior Vice President and System Chief Nurse Officer of Adventist Health (Roseville, Calif.): Over the next five years, I see nurses providing more hospital-based care in the home using remote technology. Based on that shift, we will see lower-acuity patients move into home-based care, and higher-acuity care in hospitals will increase. With that, hospital beds will be used at a different level. My bold prediction is that we will not need as many beds, but we will need higher acute care in the hospitals.
Nurses will learn differently. As we are seeing now, nurses have not been able to train in the traditional way. They are already using more remote technology to educate, onboard and orient to their roles. It looks and feels vastly different, and nurses need to be comfortable with that.
As for patient care, I think data that can be gleaned from wearable biometrics, and the use of artificial intelligence will help predict patient care on a patient-by-patient basis. Nurses will work with AI as part of their thought process, instead of completely focusing on their own judgment and assessment.
I also believe we are going to face a nursing shortage post-COVID for a few reasons. Due to the emotional and physical toll of responding to a pandemic, some nurses will decide to retire, and another group will leave based on the risks that go hand-in-hand with the profession.
As for patient care, we are going to collaborate differently. There will be more video conferencing regarding collaboration around the patient. And I think in the future we will see that the full continuum of care will include a wellness plan.
Debi Pasley, MSN, RN. Senior Vice President Chief Nursing Officer of Christus Health (Irving, Texas): I believe the demand for nurses will become increasingly visible and newsworthy throughout the pandemic. This could drive increases in salaries and numbers of qualified candidates seeking nursing as a profession in the medium and long term. The shortage will, however, continue to be a factor, leading to more remote work options to both supplement nursing at the bedside and substitute for in-person care.
Denise Ray, RN. Chief Nursing Executive of Piedmont Healthcare (Atlanta): Nursing schools will need to focus on emergency management and critical care training utilizing a team nursing model. While nursing has become very specialty-driven, the pandemic has demonstrated gaps in our ability to adapt as quickly utilizing a team model where nurses lead and direct care teams. By implementing a team model and enhancing education in the areas of emergency management and critical care, nursing can adapt quickly to the ever-changing environment.
Also, communication with patients and families will take on different dimensions with wider use of tele-therapeutic communication. Nurses will be leaders and liaisons in the process, connecting physicians, patients and patient families virtually. Nurses will play a key role in integrating patient family members as true patient care partners — making sure they have the information they need to serve an active caregiving role for their family members during and after hospitalization. We’ll also see more nurses becoming advanced nurse practitioners, playing an expanded role in all healthcare settings.
https://mailchi.mp/f2794551febb/the-weekly-gist-october-23-2020?e=d1e747d2d8

A quick stop at the local Whole Foods Market recently yielded surprising insights into the dilemma faced by physician practices in the COVID-era telemedicine boom.
The store location opened just last year, part of a brand-new residential and shopping complex designed for busy professionals. It’s larger than the old-style, pre-Amazon era stores, and was designed to integrate Amazon’s online grocery operations into the bricks-and-mortar retail setting. There’s a portion of the store set aside for Amazon “shoppers” to receive and pack online orders for pickup and delivery, along with an expanded array of convenience-food offerings for the app-powered consumer to scan and purchase.
But when COVID hit, the volume of online orders went through the roof, and the store hired a small army of Amazon shoppers (including one of our own adult children who’s on a “gap year”) to keep up with demand. The result has been barely controlled chaos—easily 70 percent of the shoppers in the aisles last weekend were young Amazon employees “shopping” on behalf of online customers. They’re all held to an Amazon-level productivity standard, which makes the pace of their cart-pushing somewhat frantic and erratic. And the discreet area at the front of the store for managing the Amazon orders has become a noisy hub, making entering and exiting the store problematic. Even the “regular” store employees at Whole Foods have begun to complain about the disruption caused by the Amazon fulfillment operation.
It’s a cautionary tale for traditional physician practices and other care delivery organizations looking to “integrate” telemedicine into normal operations. Integration sounds great in theory, but in practice raises important questions:
1) What physical space should be set aside for delivering virtual care?
2) Should telemedicine work be done in a separate, centralized location, or in existing clinic space?
3) How does the staffing of clinics need to change to meet the demand for virtual care?
4) How can we flex staffing up and down based on demand for telemedicine?
5) If new staff are required, how will they be incorporated into the existing team—or should they be managed separately?
6) What operational metrics will they be held accountable for, and what impact will those metrics have on other operational goals?
If Amazon, a worldwide leader online, renowned for running tight, precision, productivity-driven operations, is having trouble figuring out physical-virtual integration at the front end of their business, imagine how difficult these challenges will be for healthcare providers. The sooner we start to dig into these issues and find sustainable solutions, the better.