Cartoon – Today’s Board Agenda
https://mailchi.mp/f4f55b3dcfb3/the-weekly-gist-may-15-2020?e=d1e747d2d8

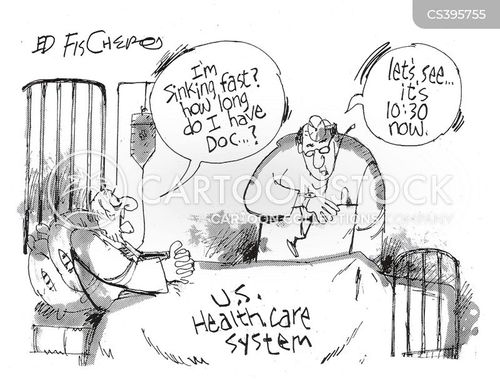
Even after hearing dozens of reports from health systems about how steep their COVID-related volume losses have been, we were still floored by this analysis from healthcare analytics firm Strata Decision Technology, documenting a 55 percent drop in patients seeking hospital care across the country.
The report, which analyzed data from 228 hospitals in 51 health systems across 40 states, found that no clinical service line was immune from steep volume losses. The graphic below shows volume loss by service line in March-April 2020 compared to the same period in 2019.
Unsurprisingly, ophthalmology, gynecology, ortho/spine and ENT—all specialties with a high portion of elective cases, and heavily dependent on procedures—saw volume declines of greater than 70 percent. But even obstetrics and neonatology (which we expected to be “pandemic proof”) and infectious disease (which we thought might be busier in the throes of COVID-19) saw losses of 20-30 percent.
Looking at specific procedures, complex elective surgeries like spinal fusion and hip and knee replacements were almost completely obliterated. Precipitous declines in encounters for chronic diseases like coronary heart disease and diabetes (down 75 and 67 percent, respectively) and cancer screenings (a 55 percent decline in breast health and a 37 percent decline in cancer care overall) point to the likelihood of worrisome disease exacerbations, and a future full of more complex patients.
The volume losses, plus a 114 percent rise in uninsured patients, led to average two-week losses of $26.5M per health system across the study’s cohort. Strata will continue to track and publish volume changes, but this early snapshot paints a bleak picture of staggering financial hits, and “lost” patient care that will carry lasting ramifications for the health of communities nationwide.
https://mailchi.mp/f4f55b3dcfb3/the-weekly-gist-may-15-2020?e=d1e747d2d8
It’s easy to become numb to the numbers we’re bombarded with on a daily basis—case counts, deaths, financial losses, unemployment claims, bailout funding. An article from the Washington Post this week put a very human face on how the coronavirus crisis is playing out on the ground, profiling the experience of 115-bed Griffin Hospital in Derby, CT.
We first got to know Griffin, and its CEO Patrick Charmel, years ago in the course of work for our former employer. It’s a remarkable, fiercely independent organization—recognized as the flagship hospital of the “Planetree” patient-centered care model, and a decade-long fixture on Fortune’s list of Top 100 Best Companies to Work For. But the COVID-19 wave hit Griffin hard, as it did much of Connecticut.
With the high cost of caring for COVID patients, and lost revenue from cancelled procedures, Griffin has had to make hard decisions about furloughing and redeploying staff—incredibly difficult for a small facility that has been a pillar of the community for a century. Charmel has been able to secure some relief in the form of advance payment from Medicare, but his efforts to lobby for a share of the state’s allocation of CARES Act grant funding for hospitals proved unsuccessful, and so the future of the hospital—or at least its continued viability as an independent organization—is in jeopardy.
In the words of Griffin’s chief financial officer, “This could be devastating for us.” As the recovery begins, and questions begin to be asked about the billions of dollars of “bailouts” paid to “greedy hospitals”—an easy narrative for the media to latch onto—it’s worth remembering what’s happening to Griffin Hospital, and to hundreds of other similar organizations across the country.
Countless communities rely on these hospitals, and their survival is worth safeguarding.




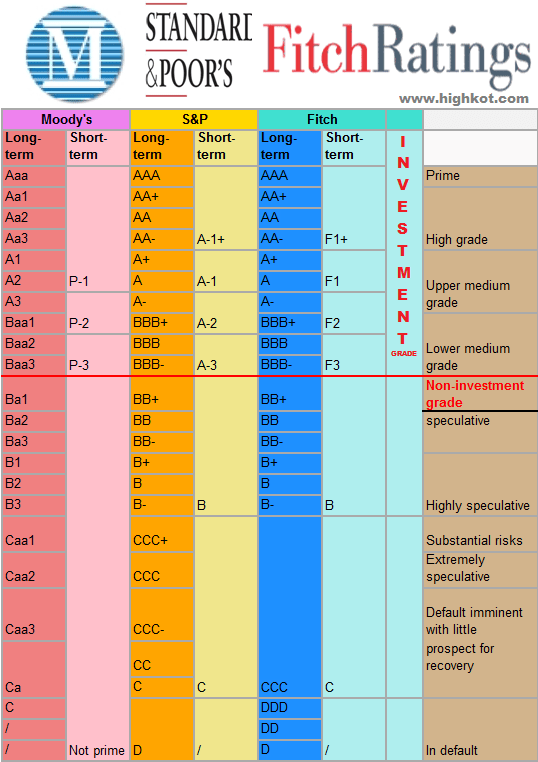
The following 16 hospital and health system credit rating downgrades occurred since March 1. They are listed below in alphabetical order.
1. Boulder (Colo.) Community Health — from “A2” to “A3” (Moody’s Investors Service)
2. Butler (Pa.) Health System — from “Baa1” to “Baa2” (Moody’s Investors Service)
3. Catholic Health System (Buffalo, N.Y.) — from “Baa1” to “Baa2” (Moody’s Investors Service)
4. Catholic Medical Center (Manchester, N.H.) — from “Baa1” to “Baa2” (Moody’s Investors Service)
5. Hutchinson (Kan.) Regional Medical Center — from “Baa3” to “Ba1” (Moody’s Investors Service)
6. Magnolia Regional Health Center (Corinth, Miss.) — from “Ba3” to “B1” (Moody’s Investors Service)
7. Marshall Medical Center (Placerville, Calif.) — from “BBB-” to “BB+” (Fitch Ratings)
8. Prisma Health (Greenville, S.C.) — from “A2” to “A3” (Moody’s Investors Service)
9. Quorum Health (Brentood, Tenn.) — from “Caa2” to “Ca” (Moody’s Investors Service)
10. SoutheastHealth (Cape Girardeau, Mo.) — from “Baa3” to “Ba1” (Moody’s Investors Service)
11. Sutter Health (Sacramento, Calif.) — from “Aa3” to “A1” (Moody’s Investors Service); from “AA-” to “A+” (S&P Global Ratings)
12. University of Vermont Health Network (Burlington) — from “A2” to “A3” (Moody’s Investors Service)
13. UPMC (Pittsburgh) — from “A+” to “A” (Fitch Ratings); from “A1” to “A2” (Moody’s Investors Service)
14. Virginia Mason Medical Center (Seattle) — from “Baa2” to “Baa3” (Moody’s Investors Service)
15. Washington County (Calif.) Health Care District — from “Baa1” to “Baa2” (Moody’s Investors Service)
16. Wood County Hospital (Bowling Green, Ky.) — from “Ba2” to “Ba3” (Moody’s Investors Service)