https://www.yahoo.com/news/during-pandemic-unanticipated-problem-health-150355070.html
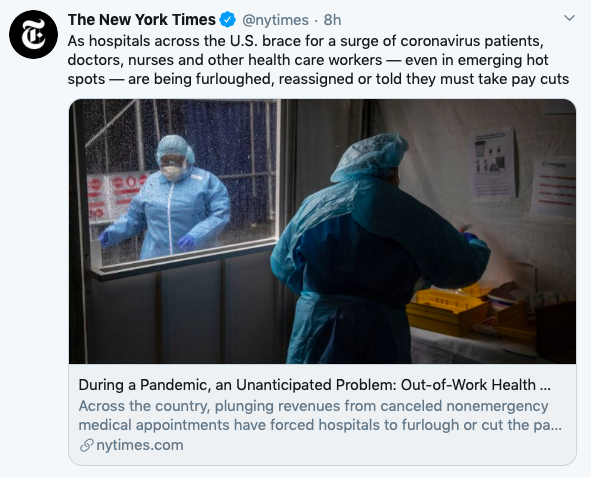
As hospitals across the country brace for an onslaught of coronavirus patients, doctors, nurses and other health care workers — even in emerging hot spots — are being furloughed, reassigned or told they must take pay cuts.
The job cuts, which stretch from Massachusetts to Nevada, are a new and possibly urgent problem for a business-oriented health care system whose hospitals must earn revenue even in a national crisis. Hospitals large and small have canceled many elective services — often under state government orders — as they prepare for the virus, sending revenues plummeting.
That has left trained health care workers sidelined, even in areas around Detroit and Washington, where infection rates are climbing, and even as hard-hit hospitals are pleading for help.
“I’m 46. I’ve never been on unemployment in my life,” said Casey Cox, who three weeks ago worked two jobs, one conducting sleep research at the University of Michigan and another as a technician at the St. Joseph Mercy Chelsea Hospital near Ann Arbor, Michigan. Within a week, he had lost both.
Mayor Bill de Blasio of New York has begged doctors and other medical workers from around the country to come to the city to help in areas where the coronavirus is overwhelming hospitals.
“Unless there is a national effort to enlist doctors, nurses, hospital workers of all kinds and get them where they are needed most in the country in time, I don’t see, honestly, how we’re going to have the professionals we need to get through this crisis,” de Blasio said Friday morning on MSNBC.
And the Department of Veterans Affairs is scrambling to hire health care workers for its government-run hospitals, especially in hard-hit New Orleans and Detroit, where many staff members have fallen ill. The department moved to get a federal waiver to hire retired medical workers to beef up staff levels.
But even as some hospitals are straining to handle the influx of coronavirus patients, empty hospital beds elsewhere carry their own burden.
“We’re in trouble,” said Gene Morreale, the chief executive of Oneida Health Hospital in upstate New York, which has not yet seen a surge in coronavirus patients.
Governors in dozens of states have delivered executive orders or guidelines directing hospitals to stop nonurgent procedures and surgeries to various degrees. Last month, the U.S. surgeon general, Dr. Jerome M. Adams, also implored hospitals to halt elective procedures.
That has left many health systems struggling to survive.
Next week, Morreale said, Oneida will announce that it is putting 25% to 30% of its employees on involuntary furlough. They will have access to their health insurance through June. Physicians and senior staff at the hospital have taken a 20% pay cut.
“We’ve been here 121 years, and I’m hoping we’re still there on the other side of this,” Morreale said.
Appalachian Regional Healthcare, a 13-hospital system in eastern Kentucky and southern West Virginia, has seen a 30% decrease in its overall business because of a decline in patient volume and services related to the pandemic. Last week, the hospital system announced it would furlough about 8% of its workforce — around 500 employees.
Hospital executives across the country are cutting pay while also trying to repurpose employees for other jobs.
At Intermountain Healthcare, which operates 215 clinics and 24 hospitals in Utah, Idaho and Nevada, about 600 of the 2,600 physicians, physicians assistants and registered nurses who are compensated based on volume will see their pay dip by about 15%, said Daron Cowley, a company spokesman.
Those reductions are tied to the drop in procedures, which has fallen significantly for some specialties, he said. The organization is working to preserve employment as much as possible, in part by trying to deploy 3,000 staff members into new roles.
“You have an endoscopy tech right now that may be deployed to be at hospital entrances” where they would take the temperatures of people coming in, Cowley explained.
In Boston, a spokesman for Partners HealthCare, with 12 hospitals, including Massachusetts General and Brigham and Women’s, said staff members whose work has decreased are being deployed to other areas or will be paid for up to eight weeks if no work is available.
But redeployment is not always an option. Janet Conway, a spokeswoman for Cape Fear Valley Health System in Fayetteville, North Carolina, said many of the company’s operating room nurses trained in specialized procedures have been furloughed because their training did not translate to other roles.
“Those OR nurses, many have never worked as a floor nurse,” she said.
Conway said nearly 300 furloughed staff members have the option to use their paid time off, but beyond that, the furlough would be unpaid. Most employees are afforded 25 days per year.
Some furloughed hospital workers are likely to be asked to return as the number of coronavirus cases rise in their communities. But the unpredictable virus has offered little clarity and left hospitals, like much of the economy, in a free fall.
Many health systems are making direct cuts to their payrolls, eliminating or shrinking performance bonuses and prorating paychecks to mirror reduced workload until operations stabilize.
Scott Weavil, a lawyer in California who counsels physicians and other health care workers on employment contracts, said he was hearing from doctors across the country who were being asked to take pay cuts of 20% to 70%.
The requests are coming from hospital administrators or private physician groups hired by the hospitals, he said, and are essentially new contracts that doctors are being asked to sign.
Many of the contracts do not say when the cuts might end, and are mostly affecting doctors who are not treating coronavirus patients on the front lines, such as urologists, rheumatologists, bariatric surgeons, obstetricians and gynecologists.
Such doctors are still being asked to work — often in a decreased capacity — yet may be risking their health going into hospitals and clinics.
“It’s just not sitting well,” Weavil said, noting that he tells doctors they unfortunately have few options if they want to work for their institution long term.
“If you fight this pay cut, administration could write your name down and remember that forever,” he said he tells them.
In other cases, physicians are continuing to find opportunities to practice in a more limited capacity, like telemedicine appointments. But that has not eliminated steep pay cuts.
“Physicians are only paid in our clinic based on their productivity in the work they do,” said Dr. Pam Cutler, the president of Western Montana Clinic in Missoula. “So they’re automatically taking a very significant — usually greater than 50% or 25% — pay cut just because they don’t have any work.”
In some areas, layoffs have left behind health care workers who worry that they will not be able to find new roles or redeploy their skills.
Cox in Michigan said he was briefly reassigned at his hospital, helping screen and process patients coming in with coronavirus symptoms, but eventually the people seeking reassignments outgrew the number of roles.
He also expressed concern that inevitable changes in the health care industry after the pandemic — paired with the possibility of a lengthy period of unemployment — could make it difficult to get his job back.
“I’m just concerned that the job I got laid off from may not be there when this is over,” Cox said. “The longer you’re away, the more you worry, ‘Am I going to be able to come back?’ So there’s a lot of anxiety about it.”
Even as many of the largest hospital networks grapple with sudden financial uncertainty, much smaller practices and clinics face a more immediate threat.
According to a statistical model produced by HealthLandscape and the American Academy of Family Physicians, by the end of April, nearly 20,000 family physicians could be fully out of work, underemployed or reassigned elsewhere, particularly as cities like New York consider large-scale, emergency reassignments of physicians.
“Many of these smaller practices were living on a financial edge to start with, so they’re not entering into this in a good position at all,” said Dr. Gary Price, the president of the Physicians Foundation. “Their margins are narrower, their patients don’t want to come in, and many of them shouldn’t anyway, so their cash flow has been severely impacted and their overhead really hasn’t.”