Cartoon – Doctors without borders, meet patient without insurance
https://mailchi.mp/burroughshealthcare/april-16-3240709?e=7d3f834d2f
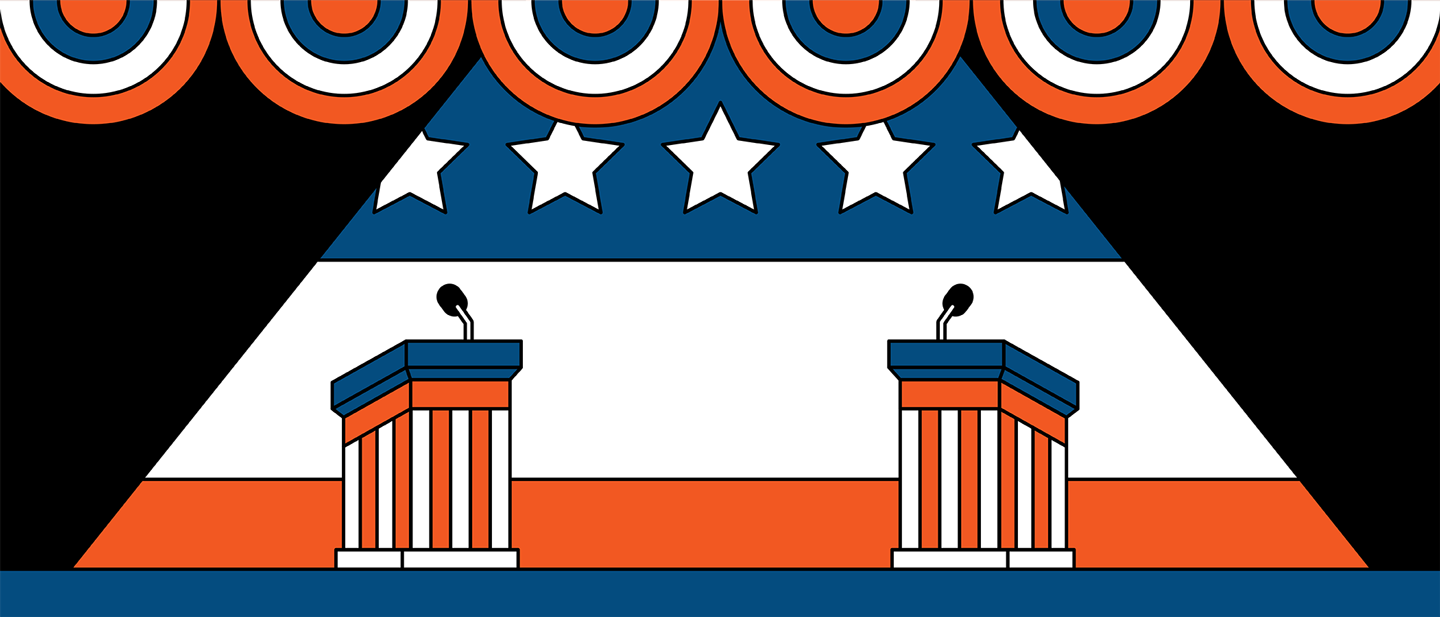
Less than three months from now, either Donald Trump will begin his second term as President, or Joe Biden will begin his first. What the U.S. healthcare system on that date and moving forward could be starkly different depending on who is sworn in.
The policy differences between the two men are essentially on opposite poles. If fully enacted, Trump’s policies could potentially cause tens of millions of Americans to lose their healthcare coverage. Biden’s policies would likely provide healthcare access to tens of millions more Americans compared to today.
In November, the U.S. Supreme Court will hear arguments in a case called California v. Texas. It stems from the 2017 tax bill that zeroed out the penalty individuals paid if they did not obtain health insurance. The argument put forth by the 20 Republican state attorney generals in that case is if the individual mandate no longer has taxing power, the entire law should be declared unconstitutional based upon a lack of severability of the entire law.
Many legal scholars have noted that this case is premised on a shaky argument. But with a 6-3 majority of conservative justices now on the high court, many bets are off as to the ACA’s survival. And President Trump just said in an interview with “60 Minutes” he fervently hoped the ACA is eliminated. He put forth no alternatives to the ACA in that interview.
Should the ACA be declared unconstitutional, health insurance for some 23 million people would be imperiled. That includes some 12 million Americans who are eligible for Medicaid under the ACA’s expanded income guidelines, and another 11 million who purchase insurance on the state and federal health insurance exchanges – roughly 85% of whom receive premium subsidies that make it more affordable. Moreover, another 14 million Americans who are estimated to have lost their employer-based health plans during the COVID-19 pandemic may not have another place to turn for coverage.
Before the ACA case, the Trump administration also promoted so-called “off-exchange” health plans, and health sharing ministries. The first is often a form of short-term health insurance, the second operates as a cooperative serving those of the same religious stripe. Both offer health coverage that is potentially cheaper that what is offered on the exchanges, but both also tend to cap it at low dollar levels. Many also bar applicants for a variety of claims, such as for maternity or cancer care, or if they have pre-existing medical conditions – practices prohibited for ACA plans.
Should Trump be re-elected and the ACA survives constitutional muster, expect to see many states apply for more waivers from that law. Georgia just received approval to modestly expand Medicaid eligibility, primarily for those poor already working 80 hours or more a month. The state is also on the cusp of being able to opt out of the healthcare.gov exchange entirely and have consumers work directly with insurance brokers to purchase coverage. However, there is nothing in the pending waiver to prevent those brokers from offering stripped-down coverage without the ACA protections that the Trump administration is already promoting.
There could also be more block grants to states for their Medicaid budgets, which most experts have concluded would reduce the number of enrollees in that program.
If Biden is elected and both incoming houses of Congress are also Democratic, the entire Supreme Court case can be mooted simply by reattaching a financial penalty to the individual mandate. That hasn’t been mentioned at all during the campaign, presumably because Biden does not want to discuss what would essentially be a promise to raise taxes. But it is the most direct way to skirt the risk of an adverse Supreme Court decision.
Biden’s campaign has also put forth numerous proposals to enlarge the ACA and the Medicare program. They include expanded premium subsidies for individuals and families to purchase coverage, and a public health plan option – which would allow those who live in the states that have yet to expand Medicaid to obtain coverage. Biden has also proposed a buy-in to Medicare at age 60.
The estimates are that an expanded ACA and other Biden plans could net another 20 to 25 million Americans healthcare coverage. That would leave fewer than 10 million – 2% to 3% of the population – without access to coverage. It would probably be as close to universal healthcare as the United States could get given its current political realities.
The two different approaches will either lead to a country where virtually everyone has access to healthcare coverage and services, or one where 50 million or more people could potentially be uninsured. It’s a shift that could impact a minimum of 45 million people – and that’s not even counting those who lost their coverage during the current public health crisis.
Elections have consequences. Less than three months from now, this one will determine whether the U.S. healthcare system will take one consequential path over another.

https://mailchi.mp/f2794551febb/the-weekly-gist-october-23-2020?e=d1e747d2d8

The upcoming election has huge implications for healthcare, far beyond how COVID is managed, ranging from how care is covered to how it’s delivered. The graphic above shows a continuum of potential policy outcomes of the November 3rd vote.
If President Trump wins a second term and Republicans control at least one house of Congress, there will likely be more attempts to dismantle the ACA, as well as continued privatization of Medicare coverage.
If Democrats win the presidency and sweep Congress, actions to expand the Affordable Care Act (ACA), or even create a national public option, are on the table—although major healthcare reform seems unlikely to occur until the second half of a Biden term.
In the short term, we’d expect to see more policy activity in areas of bipartisan agreement, like improving price transparency, ending surprise billing and lowering the cost of prescription drugs, regardless of who lands in the White House.
While healthcare emerged as the most important issue for voters in the 2018 midterm elections, the COVID pandemic has overshadowed the broader healthcare reform platforms of both Presidential candidates heading into the election. As shown in the gray box, many Americans view the election as a referendum on the Trump administration’s COVID response. Managing the pandemic is one of the most important issues for voters, especially Democrats, who now rank the issue above reducing the cost of healthcare or lowering the cost of drugs.
In many aspects, the COVID policies of Biden and Trump are almost diametrically opposed, especially concerning the role of the federal government in organizing the nation’s pandemic response.
The next administration’s actions to prevent future COVID-19 surges, ensure safe a return to work and school, accelerate therapies, and coordinate vaccine delivery will remain the most important aspect of healthcare policy well into 2021.
https://mailchi.mp/f2794551febb/the-weekly-gist-october-23-2020?e=d1e747d2d8
This week Nebraska became the latest state to receive waiver authority from the Trump administration to implement work requirements as part of its Medicaid expansion program.
The program, called “Heritage Health Adult”, will be a two-tiered system, with expansion-eligible adults choosing between “Basic” and “Prime” coverage levels. The lower tier will provide coverage for physical and behavioral health services, with a prescription drug benefit, and is open to adults not eligible for traditional Medicaid with incomes under 138 percent of the federal poverty line.
“Prime” enrollees will get additional dental, vision, and over-the-counter drug benefits, in exchange for agreeing to 80 hours per month of work, volunteering, or active job seeking, which must be reported to the state.
Nebraska voters approved the Medicaid expansion two years ago, although enrollment only began this August, and the work-linked demonstration project is slated to start next year. An estimated 90,000 additional Nebraskans are expected to enroll in Medicaid under the expanded program.
The approval of Nebraska’s Medicaid work requirement comes a week after the Trump administration approved a partial expansion of Medicaid in Georgia, called “Pathways to Coverage”, which is also tied to a requirement to seek or engage in employment or education activities.
The Georgia program also requires premium payments by eligible adults who make between 50 and 100 percent of the federal poverty line. Court challenges will inevitably ensue for both the Nebraska and Georgia programs—only Utah has successfully implemented Medicaid work requirements, with 16 other state programs either pending approval, held up in court, or awaiting implementation. We continue to be deeply skeptical of Medicaid work requirements, and believe they only serve to deter those who would otherwise qualify for coverage from enrolling, and that the expense of their implementation and ongoing operation often outweighs any savings to the state.
The argument that “work encourages health”, often advanced by proponents of work requirements, gets it exactly backwards—rather, health security encourages work, a reality that has become ever more urgent as the COVID pandemic has drawn on.
As the economy continues to falter, Medicaid’s importance as a safety net program grows ever greater, and work requirements create an unhelpful obstacle to basic healthcare access.
https://www.commonwealthfund.org/blog/2020/health-care-2020-presidential-election-whats-stake
As the presidential election draws near, we reflect on the meaningful differences in health policy priorities and platforms between the two candidates, which we’ve described more fully in our recent blog series.
While similarities exist in some areas — most notably prescription drug pricing and proposals to control health care costs — the most striking differences between the positions taken by President Donald Trump and those of former Vice President Joe Biden are on safeguarding access to affordable health care coverage, advancing health equity for those who have been historically disadvantaged by the current system, and managing the novel coronavirus pandemic.
The importance of maintaining or expanding access to affordable health care in the midst of a pandemic cannot be understated. Going into the crisis, 30 million Americans lacked health coverage, with many more potentially at risk as a result of the current economic downturn. And even for many with coverage, costs are a barrier to receiving care. Moreover, despite efforts by Congress and the Trump administration to ease the financial burden of COVID-19 testing and treatment, many people remain concerned about costs; examples of charges for COVID-related medical expenses are not uncommon.
In this context, President Trump’s efforts to repeal the Affordable Care Act (ACA) is the most important signal of his position on health care. The administration’s legal challenge of the law will be considered by the Supreme Court this fall. With no Trump proposal for a replacement to the ACA, if the Court strikes the law in its entirety or in part, many voters cannot be certain that their health coverage will be secure. By undermining the ACA — the vast law that protects Americans with preexisting health conditions and makes health coverage more affordable through a system of premium subsidies and cost-sharing assistance — the president has put coverage for millions at risk.
Trump issued an executive order to preserve preexisting condition protections. If the ACA remains intact, the order is redundant. But if the ACA is repealed by the Court, the order is meaningless because it lacks the legal underpinning and legislative framework to take effect.
In contrast, Vice President Biden has proposed expanding coverage through the ACA by adding a public option, enhancing subsidies to make health care more affordable, filling the gap for low-income families living in states that did not expand Medicaid, and giving people with employer health plans the option to enroll in marketplace coverage and take advantage of premium subsidies. For sure, if Biden is elected, many policy details must be ironed out; passing legislation in a deeply divided Congress is never easy. Despite these challenges, Biden proposes expanding health coverage rather than revoking it.
Just as COVID-19 has exposed gaps in health coverage and affordability, it also has highlighted the poor health outcomes stemming from racial and ethnic inequities in the U.S. health system. Communities of color — Black, Hispanic, and American Indian and Alaska Native people — have higher rates of COVID cases, hospitalizations, and deaths compared to white people. These disparities are a result of myriad factors, many of which are deeply rooted in structural racism. The candidates’ plans to address health disparities and advance health equity set them apart.
The ACA has played a critical role in reducing disparities in access to health care and narrowed the uninsured rate among Black and Hispanic people compared to white people. Medicaid expansion has been key to improving racial equity. Repealing the ACA, as President Trump has sought to do, would reverse these gains. Even beyond repealing the ACA, this administration has pursued policies intended to limit Medicaid eligibility — for example, by permitting states to impose work requirements and other restrictions that would lead to fewer people covered. These measures and others are already having an impact; coverage gains achieved through the ACA have eroded since 2016. Health care for legal immigrants also has declined as a result of policies like the recently finalized “public charge” rule, which seems also to have caused an increase in uninsurance among children. The administration has further revoked ACA antidiscrimination and civil rights protections for LGBTQ people.
In addition to restoring and expanding coverage under the ACA, Vice President Biden has pledged to address health disparities and reinstate antidiscrimination protections. He has a proposal to advance racial equity not just in health care but across the economy. If successful, his plan could address underlying factors contributing to higher rates of COVID-19 cases and deaths among people of color, as well as their higher rates of heart disease, diabetes, and other health conditions tied to social determinants of health.
Finally, the candidates differ deeply in their approaches to the coronavirus pandemic. President Trump has failed to orchestrate a national strategy for combating coronavirus and has routinely undermined accepted public health advice with respect to mask-wearing and social distancing. He has delegated to the states responsibility for controlling the pandemic when it is clear that the virus travels freely across the country, regardless of state borders. Lax states can negate the efforts of those states sacrificing to bring the pandemic under control. Vice President Biden has strongly signaled, though his personal conduct and rhetoric, that he intends more aggressive federal leadership in fighting the virus.
In a recent Commonwealth Fund survey of likely voters, control of the pandemic and covering preexisting conditions were very important factors in choosing a president. In seven battleground states, protections for preexisting conditions outweighed COVID-19 and health costs as the leading health care issue voters are considering. In all 10 battleground states included in the survey, Vice President Biden was viewed as the more likely candidate to address these critical health care issues.
Perhaps since the Civil War, the United States has never faced starker choices in a presidential election. In health and other areas, there are profound differences in the positions of President Trump and former Vice President Biden. Voting this November is literally a matter of life and death for the American people.
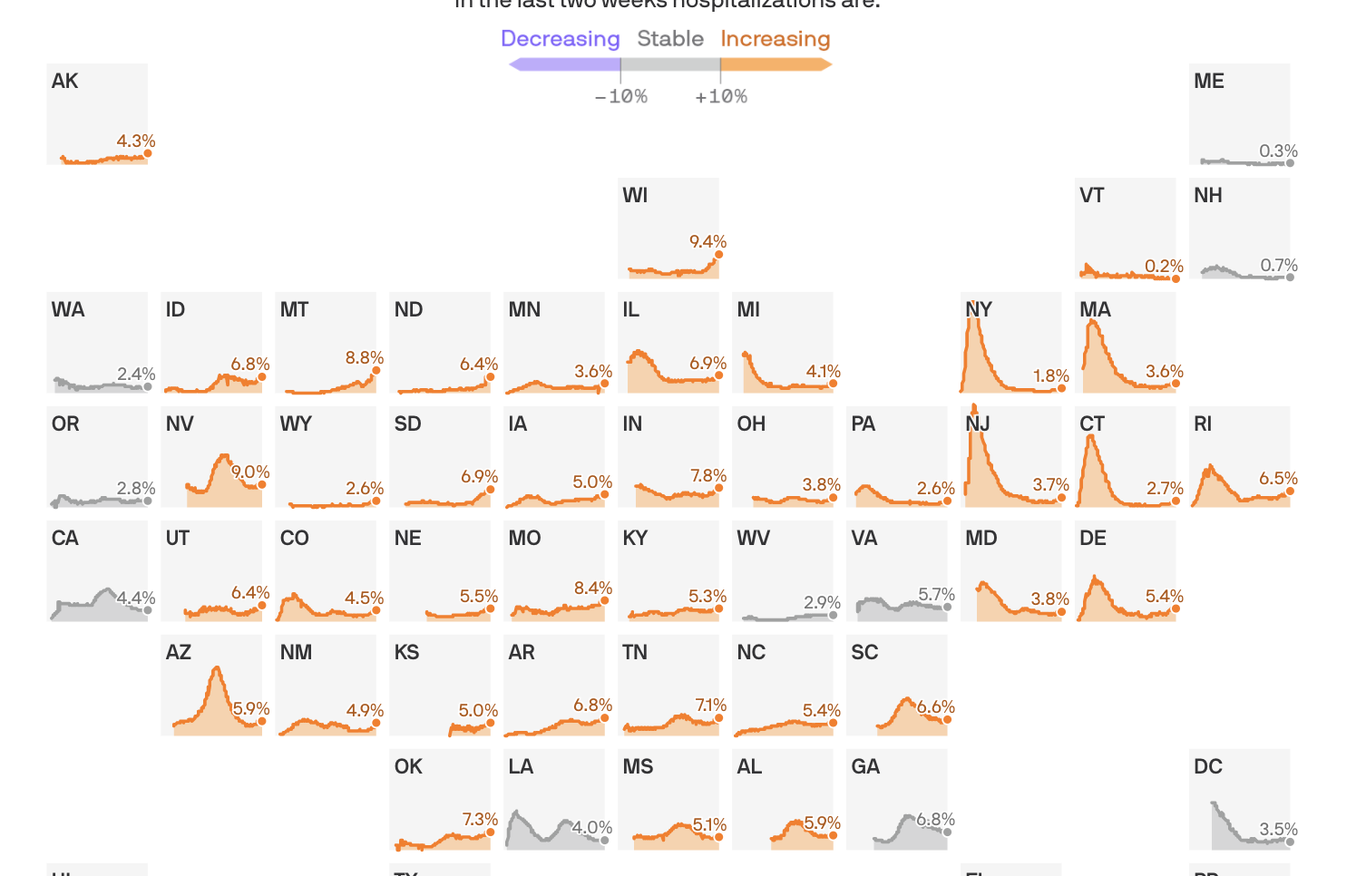
Coronavirus hospitalizations are increasing in 39 states, and are at or near their all-time peak in 16.
The big picture: No state is anywhere near the worst-case situation of not having enough capacity to handle its COVID-19 outbreak. But rising hospitalization rates are a sign that things are getting worse, at a dangerous time, and a reminder that this virus can do serious harm.
By the numbers: 39 states saw an increase over the past two weeks in the percentage of available hospital beds occupied by coronavirus patients.
Yes, but: The all-time peak of coronavirus hospitalizations happened in the spring, when 40% of New Jersey’s beds were occupied by COVID patients. Thankfully, even the the worst-performing states today are still a far cry from that.
Between the lines: These numbers, combined with the nationwide surge in new infections, confirm that the pandemic in the U.S. is getting worse — just as cold weather begins to set in in some parts of the country, which experts have long seen as a potentially dangerous inflection point.

“Last night I shared a post on Facebook that said, ‘Hey, the flu shot isn’t about you.’ Sitting here, soaking up every ounce of caffeine before my night shift, I figured I should elaborate.
The flu shot is for Influenza, a severe respiratory illness that can lead to death. Have you ever had it? I have, and it’s awful. You spike fevers, every bone and muscle in your body aches, and no matter how hard you try, you just can’t seem to catch your breath.
You get the flu shot not always for you, but for those around you. For the grandparents, whose bodies are not what they used to be, and they just can’t kick an illness in the butt like when they were young.
For the 30 year old, with HIV or AIDS, who has a weakened immune system.
For the 25-year-old mother of 3 who has cancer. She has absolutely zero immune system because of chemotherapy.
For the newborn baby who was just welcomed into the world, and isn’t quite strong enough to fight off infections on his own.
For the nurses and doctors that take care of you. If they get sick, they can’t go to work and take care of the countless patients that need them.
For the 50-year-old husband who needs a medication for his chronic illness, and that medication also weakens his immune system.
For the pregnant mom that has been trying to get pregnant for years, and now she’s trying to stay healthy for her unborn baby.
For the single dad who can’t take any more sick days and needs to provide for his kids.
For the 7-year-old boy that just wants to play with his friends. But he has a disease that puts him at a higher risk for infection, so he has to stay inside.
The flu shot is NOT always about you. It’s about protecting those around you, who cannot always protect themselves. I have been in the room as a patient has passed away, because of influenza. I have watched patients struggle to breathe, because of influenza. I have busted my butt to provide tylenol, warm blankets, nebulizers, etc. to keep that patient comfortable and fighting a terrible respiratory infection.
Herd immunity is a thing.
Influenza killing people is a thing.
You getting the flu shot, should be a thing.
Credit: Nurse Amanda Catherine Bitz

Texas has the highest uninsured rate in the U.S., and Massachusetts has the lowest, according to an analysis by WalletHub, a personal finance website.
To measure the rates of uninsured by state, analysts compared the overall insurance rates of each state in 2019 using U.S. Census Bureau data. Analysts also examined the state rates based on age, race and income. Access more information about the methodology here.
Massachusetts has the lowest uninsured rate for adults and children, at 3.39 percent and 1.52 percent, respectively. In Texas, which ranked last, the children’s uninsured rate is 12.75 percent and the adults’ uninsured rate is 20.47 percent.
Here is each state ranked from lowest to highest uninsured rate, according to the analysis:
1. Massachusetts
2. Rhode Island
3. Hawaii
4. Vermont
5. Minnesota
6. Iowa
7. New York
8. Wisconsin
9. Pennsylvania
10. Michigan
11. Connecticut
12. Maryland
13. New Hampshire
14. Kentucky
15. Delaware
16. Ohio
17. Washington
18. West Virginia
19. North Dakota
20. Oregon
21. Illinois
22. California
23. New Jersey
24. Virginia
25. Colorado
26. Maine
27. Montana
28. Nebraska
29. Indiana
30. Louisiana
31. Arkansas
32. Kansas
33. Utah
34. Alabama
35. New Mexico
36. Missouri
37. Tennessee
38. South Dakota
39. Idaho
40. South Carolina
41. North Carolina
42. Arizona
43. Nevada
44. Alaska
45. Wyoming
46. Mississippi
47. Florida
48. Georgia
49. Oklahoma
50. Texas

The undercurrent of the VP debate is the age and health of the two men vying for the presidency.
The two remaining presidential debates, scheduled for October 15 and 22, are in question due to President Trump’s positive COVID-19 and quarantine status, making the vice presidential debate this Wednesday at 9 p.m. even more important than VP debates of past elections.
The undercurrent in the debate consists of the ages of challenger Biden, who is 77 and turning 78 before the end of the year, and Trump, 74, who has been hospitalized for COVID-19 and was released from Walter Reed Army Medical Center on Monday afternoon. Trump has said he plans to debate Biden on October 15.
This VP debate is big, said Paul Keckley, a healthcare policy analyst and managing editor of the Keckley Report.
“The reason is not so much the two are debating,” Keckley said. “We have a 77- year-old challenger and a 74-year-old incumbent. Voters are expecting the odds are one will become disabled and the vice president is going to step in. That’s the undercurrent of this debate.”
Healthcare is an obvious dominant theme Wednesday night beyond the health of the two men seeking the presidency.
It is expected that Biden’s running mate, Kamala Harris will challenge Vice President Mike Pence on his role heading the coronavirus task force when close to 7.5 million people in this country have been infected with COVID-19 and more than 200,000 have died.
Pence will likely challenge Harris on her support for Medicare for All before she backtracked to support Biden’s public-private option for healthcare coverage.
Pence and Harris are expected to lay out the healthcare plans of their respective Republican and Democratic nominees less than four weeks before the election, in a way the lead candidates failed to get across during the first presidential debate that presented more chaos than clarity.
TRUMP AND BIDEN PLANS
Trump and Biden differ fundamentally on whether the federal government should be involved in the business of providing healthcare coverage.
Trump’s guiding principles rest on the pillar of state autonomy as opposed to a federalized healthcare system and Biden’s maxim that healthcare is a right, not a privilege.
Trump believes that private solutions are better than government solutions, according to Keckley. He is much less restrained on private equity and the Federal Trade Commission’s scrutiny of vertical integration. States become the gateway to the market as private solutions are sold to states as innovation.
Trump’s other concept is that the door to engaging consumers in healthcare is price transparency. His view is that price transparency will spawn consumer engagement.
Centers for Medicare and Medicaid Services Administrator Seema Verma, who was appointed by Trump in 2016 based largely on the recommendation of Pence, is instituting a rule, starting January 1, 2021, requiring hospitals to have price transparency for 300 shoppable services. Hospitals are being required to make their contract terms with payer accessible.
This is separate from CMS’s interoperability rule aimed at payers that also goes into effect on January 1.
Trump believes healthcare is a personal responsibility, not a public obligation. To Trump, healthcare is a marketplace where there are winners and losers, according to Keckley.
Biden has a more developed policy platform on making healthcare a universal right, starting with strengthening the Affordable Care Act that was passed while Biden was vice president during President Barack Obama’s terms.
Biden wants to increase the eligibility for tax subsidies in the ACA up to 400% of the federal poverty level, which would expand access to subsidized health insurance.
He also wants to reduce the affordability threshold for employer insurance. Currently, if employees pay more than 9.7% of their adjusted income for their workplace coverage, they can seek a plan in the ACA marketplace. Biden would lower that eligibility for ACA coverage to 8.5%, opening the door for many more consumers to be insured through the ACA, at a lower cost.
Biden would also lower the age of eligibility for Medicare from 65 to 60.
For companies such as manufacturing and transportation, in which individuals can retire after 30 years of service, this lets them into the Medicare system earlier to fill that gap between retirement and Medicare eligibility.
Biden’s public option would create insurance plans that would compete with private plans.
The other factor to watch on the Biden side, Keckley said, is his clear focus on equity and diversity in healthcare.
AFFORDABLE CARE ACT
Biden wants to strengthen Obamacare while Trump is actively pursuing a repeal of the law through the Supreme Court.
President Trump’s debate prep and the White House Rose Garden event announcing the nomination of Judge Amy Coney Barrett to replace the late Supreme Court Justice Ruth Bader Ginsburg, border on the definition of super spreader events.
The Justices, perhaps with the addition of Trump’s pick, Amy Coney Barrett, if there are enough Republican senators well enough and in attendance to vote for confirmation, are scheduled to hear oral arguments in the case brought by 18 GOP-led states on November 10, the week after the election.
Senators must be present to vote, and Republicans, who have a majority of 53 to 47 seats, need a four-vote majority. Two Republican senators – Susan Collins of Maine and Lisa Murkowski of Alaska – have said they wouldn’t vote on a nominee prior to the election. Vice President Mike Pence could cast the deciding vote in a tie.
Three Republican senators have tested positive for the coronavirus. Sens. Mike Lee of Utah and Thom Tillis of North Carolina, who sit on the Judiciary Committee, tested positive for COVID-19 days after attending the White House Rose Garden event on September 26. Republican Sen. Ron Johnson of Wisconsin is now the third to test positive, though he did not attend that event.
There was a lack of social distancing and mask wearing at both the Rose Garden nomination and at a meeting between Trump and staff for debate prep. Twelve people in Trump’s inner circle, including his wife Melania, former New Jersey governor Chris Christie and White House Press Secretary Kayleigh McEnany, have tested positive since attending.
Senate Majority Leader Mitch McConnell wrote in an email to GOP senators obtained by CNN that he needs all Republican senators back in Washington by October 19.
COVID-19
Trump announced in a tweet Monday that he would be leaving Walter Reed later in the afternoon, saying he felt “really good!” and adding, “Don’t be afraid of Covid. Don’t let it dominate your life. We have developed, under the Trump Administration, some really great drugs & knowledge. I feel better than I did 20 years ago!”
Trump has been criticized for leaving the hospital on Monday to take a drive-by ride to wave to supporters. Attending physician Dr. James Phillips called the action “insanity” and “political theater” that put the lives of Secret Service agents in the car with him at risk.
Trump has downplayed the virus in an effort to reopen the country and the economy, and has put the blame on China, where the coronavirus originated.
Trump told Biden during the debate, “We got the gowns; we got the masks; we made the ventilators. You wouldn’t have made ventilators – and now we’re weeks away from a vaccine.”
Biden puts the blame squarely on Trump for delaying action to stop the spread.
Biden said during the debate: “Look, 200,000 dead. You said over seven million infected in the United States. We in fact have 5% or 4% of the world’s population – 20% of the deaths. Forty thousand people a day are contracting COVID. In addition to that, about between 750 and 1,000 people, they’re dying. When [Trump] was presented with that number he said ‘It is what it is’ – what it is what it is – because you are who you are. That’s why it is. The president has no plan. He hasn’t laid out anything.”
Biden said that back in July he laid out a plan for providing protective gear and providing money the House passed to get people the help they need to keep their businesses open and open schools.
Under Trump’s Administration, Congress passed $175 billion in provider relief funds for hospitals, small businesses, individuals and others – $100 billion from the CARES Act and $75 billion from the Paycheck Protection Program and Healthcare Enhancement Act.
MEDICAID EXPANSION
CMS Administrator Seema Verma was healthcare advisor to Pence while he was governor of Indiana. Her consulting firm, SVC, Inc., worked closely with Pence to design Indiana’s Medicaid expansion under the Affordable Care Act. They developed a unique Medicaid expansion program called Health Indiana Plan 2.0, which mandated low income adults above the poverty level pay monthly premiums for their healthcare.
Members who did not pay faced being disenrolled for six months.
As administrator, Verma has initiated similar work requirements for Medicaid coverage nationwide.
While as governor Pence implemented Medicaid expansion, as vice president he has supported torpedoing the ACA, and has pushed the Graham-Cassidy plan for healthcare reform that would have replaced the ACA.
DRUG PRICES
Neither Trump nor Biden has taken on the pharmaceutical industry in a meaningful way, though both have voiced a strong belief that drug manufacturers are egregious to the system, according to Keckley.
“Both camps are saying, we’re really going to take them on,” he said.
During the debate, Trump said he was cutting drug prices by allowing American consumers to buy drugs from Canada and other countries under a favored nation status.
“Drug prices will be coming down, 80 or 90 percent,” Trump said during the debate, telling Biden he hadn’t done anything similar during his 47 years in government.
If Trump gets a second term, there will likely be more industry folks in his circle, following up on his first term of stacking his cabinet with business people.
Biden would be more likely to lean toward a blend of public health officials and industry executives. There would be more of a spotlight on wealth creation in healthcare and executive pay.
In the $1.1 trillion world of prescription drugs, the United States makes up 40% of the market.
“We’re the hub of the prescription drug industry,” Keckley said.