https://www.politico.com/news/agenda/2019/11/25/medicare-for-all-save-money-072178?utm_source=The+Fiscal+Times&utm_campaign=ae11965f63-EMAIL_CAMPAIGN_2019_11_26_10_44&utm_medium=email&utm_term=0_714147a9cf-ae11965f63-390702969

We invited experts to cut through one of the biggest campaign claims about single-payer health care — and what might really work.
Every year, health care eats up a huge and growing chunk of America’s GDP — soon projected to be $1 in every $5 spent in the U.S. ― and “Medicare for All” supporters love to tout its ability to bring that dizzying price tag down.
Would it? Is that even possible in today’s political reality?
For the answer, we looked past the candidates making lavish promises about their policies and turned instead to the experts who’ve been studying this question for years. To encourage a lively back-and-forth, we opened up a shared file and invited six of America’s smartest health-cost thinkers to weigh in freely on a handful of questions, arguing in real time about how and whether a new system might deliver on this one big promise.
The Lineup

DON BERWICK
- Institute for Healthcare Improvement. Berwick was the Medicare administrator under President Barack Obama and advised Elizabeth Warren on her Medicare for All plan.

KATE BAICKER
- Dean of the University of Chicago Harris School of Public Policy.

BRIAN BLASE
- President of Blase Policy Strategies, a visiting fellow at The Heritage Foundation, and previously special assistant to President Donald Trump for economic policy.

LANHEE CHEN
- Director of domestic policy studies at Stanford University, and fellow at the Hoover Institution.

SHERRY GLIED
- Dean of New York University’s Robert F. Wagner Graduate School of Public Service.

HANNAH NEPRASH
- Assistant professor at University of Minnesota School of Public Health.
1. The Trillion-Dollar Question
Could Medicare for All really rein in health care spending in America?
Don Berwick: A single-payer system may be the only plausible way to get a grip on our health care costs without harming patients. Without it, it’s hard to find a route to the administrative simplification, purchasing power, and investments in better quality of care and prevention that can get at the fundamental drivers of cost increases that don’t add value. Whether it’s realistic or not depends on building public confidence in the benefits of that strategy.
Kate Baicker: The potential simplification has to be balanced against the increase in health care use that we should expect when uninsured people gain access to insurance. Insured people use a lot more health care than uninsured people! That’s a very good thing for their health, but it comes with a cost that taxpayers have to finance. Given that, I’m not sure that we can lower overall health spending without restricting access to care in ways that people might not like, such as through denying coverage, or even shortages caused by cutting back on reimbursement rates.
Hannah Neprash: If I’m sure about anything in this world, it’s that expanding health insurance coverage will increase the total quantity of health care consumed, like Kate said! So that means M4A would need to dramatically reduce the price we pay for care, in order to rein in spending. That’s not out of the question; we know there’s tremendous variation within commercial insurance prices that doesn’t necessarily reflect higher quality. But it could raise concerns about access to care.
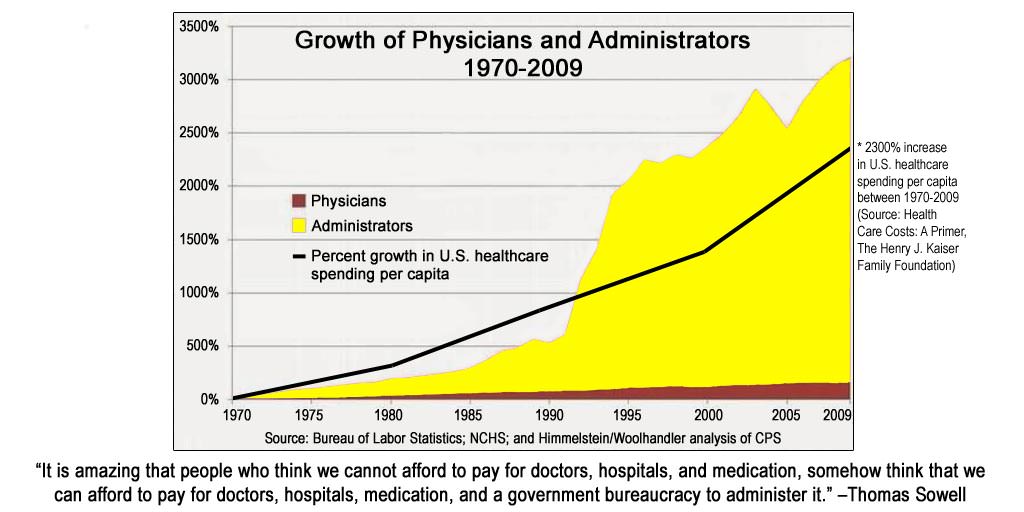
Brian Blase: No. Economics 101 says that increasing the demand without doing anything about the supply will put upward pressure on prices. The government can force prices below market-clearing levels, but that would lead to access problems for patients and complaints from politically powerful hospitals and providers. Also, Medicare rates are set through a political process with a bureaucracy subject to intense pressure. Unsurprisingly, Medicare overpays for certain services and procedures, and underpays for others. A single-payer program would likely lead to more wasteful health care expenditures, since it would further reduce market signals about what is valuable and what is not. Innovation and disruption represent the best way to lower costs without harming quality of care, and an even bigger Medicare-style bureaucracy would favor the status quo over more innovative ways of delivering care.
Don Berwick: I have some skepticism about claims Medicare for All will unleash major increases in utilization. That’s not the case in some European countries with health care “free at the point of service,” and I believe that the experience in Massachusetts with nearly universal coverage didn’t match the predictions of major utilization increases — at least not persistent increases.
Kate Baicker: I think we actually have a fair amount of evidence that when patients have to pay less for care, they use more. Again, that’s not a bad thing in and of itself, but I think it’s unrealistic to hope that we can insure more people but spend less on health care overall without substantially cutting back on payments or restricting services, both of which would restrict access to care for the insured.
Sherry Glied: This question really comes down to politics, not economics. As Hannah says, prices are the key here, but we already know Congress has had a very hard time reducing hospital prices or physician prices . Right now, a Democratic majority in the House can’t even agree on a way to address surprise billing, which benefits only a small minority of physicians. Today, health care is the largest employer in over 55 percent of U.S. congressional districts ― a political reach the defense industry must envy. Under a single-payer system, the entire livelihood of all those health care providers would depend on choices made by federal legislators and regulators. That’s an extraordinarily potent political force, with unparalleled access to members of Congress. Think of those annual checkups! Simply invoking the words “single-payer” isn’t going to change that political reality.
Lanhee Chen: I have to agree with Sherry that the history of entitlement spending in the United States supports the notion that the politics will make it almost impossible for single-payer to be fiscally sustainable. The current proposals from the likes of Elizabeth Warren make dramatically unrealistic assumptions about what will happen to provider reimbursement rates — and the history of how Congress has reacted to the provider lobby makes clear that if it passes some kind of single-payer system, reimbursement rates would steadily rise and costs would rise with them. Of course, single-payer advocates could be honest about their intent to ration care to constrain cost — but here again, it’s unlikely politicians would actually make such a concession.
2. The Hospital Challenge
We know that more money is spent in hospitals than any other setting or service, but hospital costs haven’t gotten much attention from the 2020 candidates — in part because beating up on hospitals isn’t good politics. So what can be done there?
Hannah Neprash: The past decade-plus has seen a tremendous amount of merger and acquisition activity in and across hospital markets. As a result, large hospital systems have the bargaining power to command increasingly high prices from commercial insurers. Antitrust enforcement should certainly play a role. I’m also intrigued by what states like Massachusetts are doing, with agencies like the Health Policy Commission that monitors health care spending growth.
Don Berwick: Moving away from fee-for-service payment to population-based payment would be a powerful way to check needless hospital spending. We’d also benefit from stronger antitrust action to mitigate the price effects of hospital market consolidation. Strengthening community resources for home-based and noninstitutional care is also important.
Brian Blase: The key answer is to increase competition. As a reference, see the Trump administration’s 2018 report, Reforming America’s Health Care System Through Choice and Competition. Beyond putting more resources into antitrust enforcement, Congress should also consider restricting anti-competitive contract terms, like “all-or-nothing” contracts that require that every hospital and provider in a system participate in an insurer’s network if the insurer wants to contract with any hospital or provider in that system. The actual practice of medicine matters, too: If states took steps to allow providers to practice to the “top of their license,” delivering the most advanced care they’re qualified to do, it would let hospitals trim costs by using highly qualified but lower-cost alternatives — such as nurse anesthetists instead of specialist MDs on some procedures.
Sherry Glied: I’m sympathetic to Brian’s emphasis on the role of competition, but unfortunately, only a tiny minority of areas in the U.S. have the population base to support four or more large hospitals, which is the number needed for that kind of competition. Some combination of maximum price regulation in markets where there are few choices and expanded public programs to put downward pressure on prices would help. Interestingly, the share of U.S. health care expenditures that goes to hospitals is the same today as it was in 1960 ― before Medicare and Medicaid. I’m dubious that simply changing methods of payment is going to make much of a dent.
Don Berwick: Competition and transparency may help, but I do not have faith that these will be sufficient to control escalating prices. I suspect we will sooner or later have to turn to some form of direct price controls.
Brian Blase: Of course, we already have price controls throughout the health care sector as a result of Medicare fee-for-service’s prominent role. And just a reminder that the onset of Medicare led to an explosion of health care spending in the United States.
3. Would Transparency Work?
One thing everyone across the ideological spectrum seems to agree on is that we need more transparency in health care pricing, so everyone from patients to regulators can see what things actually cost. But what’s the evidence that this actually helps keep costs down? And what more could policymakers realistically achieve, given pushback from industry groups?
Don Berwick: I’m very much in favor of total transparency in pricing. It’s hard to control costs if we don’t know how the money flows. But the evidence suggests that simple-minded notions of informing patients to create price sensitivity don’t work. The effects of transparency are more subtle and indirect.
Kate Baircke: Information alone goes only so far: It has to be coupled with a system that rewards quality of care and health outcomes, rather than just the quantity of care delivered. And it has to be done in a nuanced way. On the patient side, simply increasing deductibles, for example, is likely to restrict patients’ access to high- as well as low-value care — but cost-sharing that is clearly tied to value, like having lower copayments for highly beneficial services, could create pressure for better use of resources and better outcomes. Similarly, on the provider side, having providers share in the benefits of steering patients toward higher-value care is likely to be much more effective in improving value than just cutting back on payment rates.
Brian Blase: I just wrote a paper on this subject, so I apologize for a somewhat long answer. There’s definitely evidence that consumers who have incentives to care about prices benefit from transparent prices — meaning they shopped and saved money. Consumers who used New Hampshire’s health care price website for medical imaging saved an estimated 36 percent per visit. Safeway linked a reference pricing design with a price transparency tool, and its employees saved 27 percent on laboratory tests and 13 percent on imaging tests. (Reference pricing means that consumers are given a set amount of money for a procedure, and then bear any cost above the reference price.) California used reference pricing for orthopedic procedures for their public employees and retirees, and it led to a 9- to 14-percentage-point increase in the use of low-price facilities, and a 17-percent to 21-percent reduction in prices. Perhaps the neatest finding is that people who didn’t shop also benefited, since providers lowered prices for everyone. In California, about 75 percent of these price reductions benefited people who were not participating in the reference pricing model.
So in my paper, I argue that the primary way price transparency will create benefit is by helping employers drive reforms — by easing their ability to use reference price models, better monitoring insurers, and designing their benefits so employees have an incentive to use lower-cost providers.
Hannah Neprash: I think it really depends on what we mean here. Simply providing price information to patients via price transparency tools hasn’t changed behavior much. Reference pricing is promising — because patients switch providers, and higher-priced providers appear to lower their prices in response. Since patients rely so heavily on the recommendation of their physicians, I’d been hopeful about physician-directed price transparency, but existing evidence doesn’t seem to bear this out. This may very well be another area where aligning financial incentives is crucial, so physicians share in the savings if they steer patients toward more efficient providers.
Sherry Glied: Some kinds of price transparency seem to be no-brainers. No one should ever face an unexpected out-of-pocket bill for a scheduled medical service, and everyone should know exactly how much to expect to pay in an emergency. That’s Consumer Protection 101. Things get more complicated from there. If incentives of patients and referring physicians are aligned, there’s some hope of steering patients toward lower-cost providers and encouraging lower prices all-around through structured shopping tools, like reference pricing, but the scope of these programs is very narrow. We actually don’t know — theoretically or empirically — what would happen if all doctors, hospitals and insurers knew what others were paying or charging. And in general, wholesale prices of that type, paid by one business to another, are not transparent in other industries either.
Brian Blase: I think the potential application of reference price models and value-based arrangements is far broader than Sherry does. Only a small amount of health care procedures or services are for emergency care.
Lanhee Chen: The one thing I would add here is that price transparency — however one defines it — should be coupled with better and more thorough information about provider quality. We have long struggled with a way to report quality measures that account for differences in underlying patient health and other factors, but there are a number of private-sector and nonprofit driven efforts that have made good progress on quality reporting in recent years. Whatever efforts there are to drive forward with transparency on the pricing side, we shouldn’t forget that those measures alone may not be enough to help consumers make truly educated decisions.
4. OK, Panel: Now What?
If it were up to you, what’s a politically viable first step you’d take to bring down health care costs right now?
Don Berwick: I’d like to give provider systems the flexibility to invest in care and supports that really help patients, instead of trapping the providers on the fee-for-service hamster wheel of continually increasing activity. So, continue bipartisan efforts to end fee-for-service payment wherever possible. The more we can orient payment toward a population-based system, the faster we can likely make progress. By “population-based” payment, I mean a range of options including capitated payments, global budgets and, generally, paying integrated care systems to take responsibility for the health of groups of enrollees over time.
Kate Baicker: I agree that moving away from fee-for-service and toward value-based payments would be a big step in the right direction. I’d also like to see the Cadillac tax implemented, to limit the regressive subsidy of expensive employer-based plans. This would both make our system both more progressive and more fair, and also promote higher-value health insurance plans.
Brian Blase: I agree with Kate that the Cadillac tax should be implemented, although I recommend a reform that would exempt contributions to health savings accounts from the tax thresholds — so we’re replacing a subsidy for third-party payment with a subsidy for personal accounts that employees own and control. More generally, Regina Herzlinger, the dean of the consumer-directed health reform movement has put it this way: “Choice supports competition, competition fuels innovation, and innovation is the only way to make things better and cheaper.” The Trump administration’s report I mentioned earlier has more than 50 recommendations to maximize choice and competition in health care. For politically possible steps in the near term, we should pursue real price transparency at the federal level, and at the state level we should encourage states to allow providers to practice to the top of their license and eliminate anti-competitive restrictions, like certificate-of-need laws.
Sherry Glied: Medicaid for all! Give all Americans access to a low-cost health care option, as is done in Australia. That will put downward pressure on prices across the system, because providers will know that if they charge too much, patients will revert to public insurance.
Kate Baicker: When it comes to Medicare for All, my colleagues Mark Shepard, Jon Skinner and I have some new analysis suggesting that a “one size fits all” Medicare-type program is increasingly unsustainable as medical technology advances, income disparities rise and taxes increase. A workable alternative would be a more basic universal insurance package that people could then choose to “top up” if they wanted — more like “Medicaid for All” (thanks for the setup, Sherry!). That has the potential to make our health care spending more efficient in a way that can benefit both high- and low-income people.
Brian Blase: Without knowing the details, I like Kate’s proposal. I’ve long argued that we should send public subsidies directly to people and let them choose how they want to finance their health care, rather than sending subsidies directly to insurance companies or health care providers.
Lanhee Chen: I think there is bipartisan agreement around the need to move away from fee-for-service arrangements, but the devil is in the details. Similarly, bipartisan thinkers and analysts generally agree on the benefits of limiting the tax subsidy for employer-sponsored health insurance — but politically it’s hard to imagine too many politicians coming out to defend the Cadillac tax or supporting other limits.