As visits plummet because of the coronavirus, small physician practices are struggling to survive.
Autumn Road in Little Rock, Ark., is the type of doctor’s practice that has been around long enough to be treating the grandchildren of its eldest patients.
For 50 years, the group has been seeing families like Kelli Rutledge’s. A technician for a nearby ophthalmology practice, she has been going to Autumn Road for two decades.
The group’s four doctors and two nurse practitioners quickly adapted to the coronavirus pandemic, sharply cutting back clinic hours and switching to virtual visits to keep patients and staff safe.
When Kelli, 54, and her husband, Travis, 56, developed symptoms of Covid-19, the couple drove to the group’s office and spoke to the nurse practitioner over the phone. “She documented all of our symptoms,” Ms. Rutledge said. They were swabbed from their car.
While the practice was never a big moneymaker, its revenues have plummeted. The number of patients seen daily by providers has dropped to half its average of 120. The practice’s payments from March and April are down about $150,000, or roughly 40 percent.
“That won’t pay the light bill or the rent,” said Tabitha Childers, the administrator of the practice, which recently laid off 12 people.
While there are no hard numbers, there are signs that many small groups are barely hanging on. Across the country, only half of primary care doctor practices say they have enough cash to stay open for the next four weeks, according to one study, and many are already laying off or furloughing workers.
“The situation facing front-line physicians is dire,” three physician associations representing more than 260,000 doctors, wrote to the secretary of health and human services, Alex M. Azar II, at the end of April. “Obstetrician-gynecologists, pediatricians, and family physicians are facing dramatic financial challenges leading to substantial layoffs and even practice closures.”
By another estimate, as many as 60,000 physicians in family medicine may no longer be working in their practices by June because of the pandemic.
The faltering doctors’ groups reflect part of a broader decline in health care alongside the nation’s economic downturn. As people put off medical appointments and everything from hip replacements to routine mammograms, health spending dropped an annualized rate of 18 percent in the first three months of the year, according to recent federal data.
While Congress has rushed to send tens of billions of dollars to the hospitals reporting large losses and passed legislation to send even more, small physician practices in medicine’s least profitable fields like primary care and pediatrics are struggling to stay afloat. “They don’t have any wiggle room,” said Dr. Lisa Bielamowicz, a co-founder of Gist Healthcare, a consulting firm.
None of the money allocated by lawmakers has been specifically targeted to the nation’s doctors, although the latest bill set aside funds for community health centers. Some funds were also set aside for small businesses, which would include many doctors’ practices, but many have faced the same frustration as other owners in finding themselves shut out of much of the funding available.
Federal officials have taken some steps to help small practices, including advancing Medicare payments and reimbursing doctors for virtual visits. But most of the relief has gone to the big hospital and physician groups. “We have to pay special attention to these independent primary care practices, and we’re not paying special attention to them,” said Dr. Farzad Mostashari, a former health official in the Obama administration, whose company, Aledade, works with practices like Autumn Road.
“The hospitals are getting massive bailouts,” said Dr. Christopher Crow, the president of Catalyst Health Network in Texas. “They’ve really left out primary care, really all the independent physicians,” he said.
“Here’s the scary thing — as these practices start to break down and go bankrupt, we could have more consolidation among the health care systems,” Dr. Crow said. That concerns health economists, who say the steady rise in costs is linked to the clout these big hospital networks wield with private insurers to charge high prices.
While the pandemic has wreaked widespread havoc across the economy, shuttering restaurants and department stores and throwing tens of millions of Americans out of work, doctors play an essential role in the health of the public. In addition to treating coronavirus patients who would otherwise show up at the hospital, they are caring for people with chronic diseases like diabetes and asthma.
Keeping these practices open is not about protecting the doctors’ livelihoods, said Michael Chernew, a health policy professor at Harvard Medical School. “I worry about how well these practices will be able to shoulder the financial burden to be able to meet the health care needs people have,” he said.
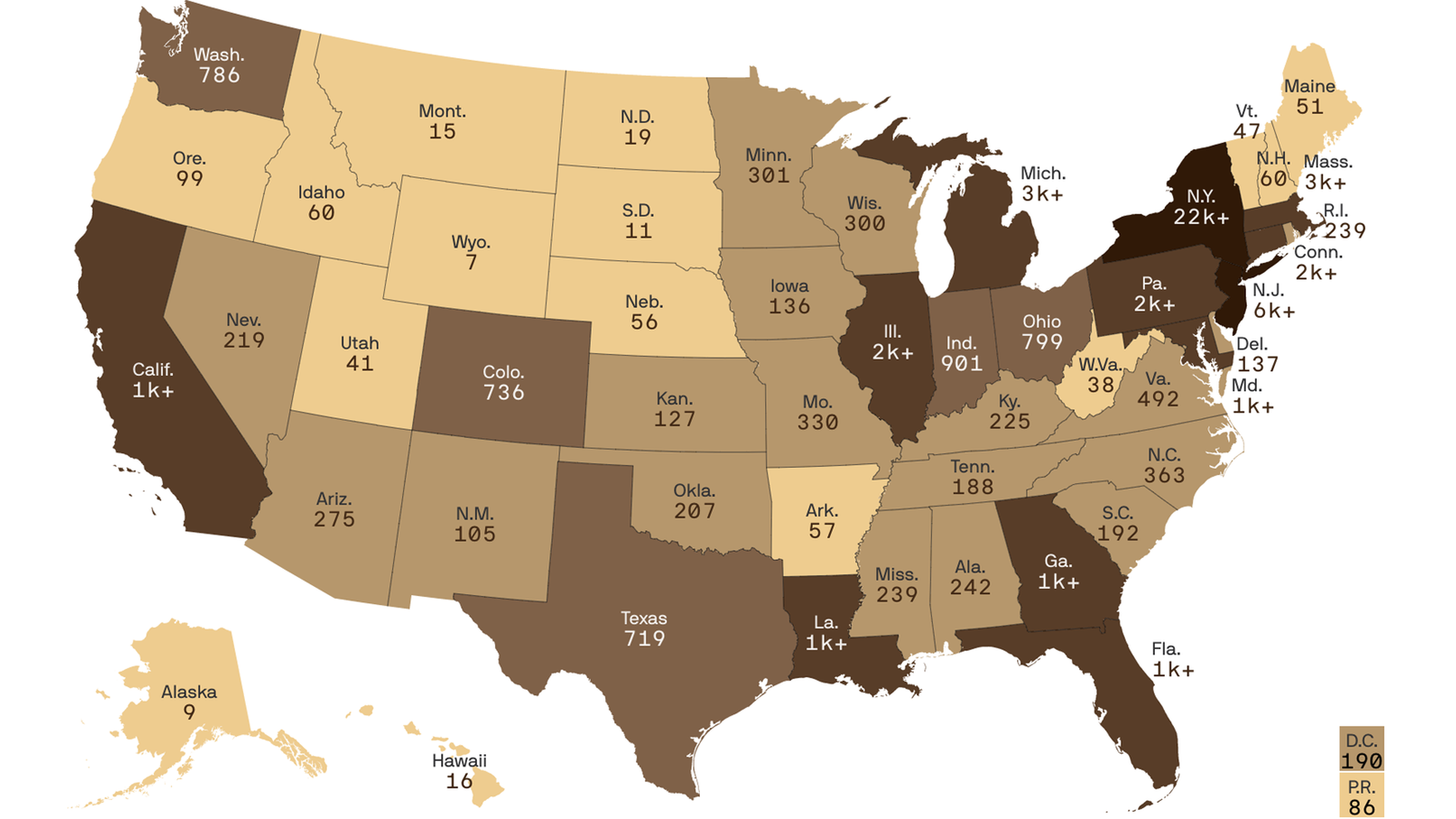
“If practices close down, you lose access to a point of care,” said Dr. Chernew, who was one of the authors of a new analysis published by the Commonwealth Fund that found doctor’s visits dropped by about 60 percent from mid-March to mid-April. The researchers used visit data from clients of a technology firm, Phreesia.
Nearly 30 percent of the visits were virtual as doctors rushed to offer telemedicine as the safest alternative for their staff and patients. “It’s remarkable how quickly it was embraced,” said Dr. Ateev Mehrotra, a hospitalist and associate professor of health policy at Harvard Medical School, who was also involved in the study. But even with virtual visits, patient interaction was significantly lower.
Almost half of primary care practices have laid off or furloughed employees, said Rebecca Etz, an associate professor of family medicine at Virginia Commonwealth University and co-director of the Larry A. Green Center, which is surveying doctors with the Primary Care Collaborative, a nonprofit group. Many practices said they did not know if they had enough cash to stay open for the next month.
Pediatricians, which are among the lowest paid of the medical specialties, could be among the hardest hit. Federal officials used last year’s payments under the Medicare program to determine which groups should get the initial $30 billion in funds. Because pediatricians don’t generally treat Medicare patients, they were not compensated for the decline in visits as parents chose not to take their children to the doctor and skipped their regular checkups.
“This virus has the potential to essentially put pediatricians out of business across the country,” said Dr. Susan Sirota, a pediatrician in Chicago who leads a network of a dozen pediatric practices in the area. “Our waiting rooms are like ghost towns,” she said.
Pediatricians have also ordered tens of thousands of dollars on vaccines for their patients at a time when vaccine rates have plunged because of the pandemic, and they are now working with the manufacturers to delay payments for at least a time. “We don’t have the cash flow to pay them,” said Dr. Susan Kressly, a pediatrician in Warrington, Pa.
Even those practices that quickly ramped up their use of telemedicine are troubled. In Albany, Ga., a community that was an unexpected hot spot for the virus, Dr. Charles Gebhardt, a doctor who is treating some infected patients, rapidly converted his practice to doing nearly everything virtually. Dr. Gebhardt also works with Aledade to care for Medicare patients.
But the telemedicine visits are about twice as long as a typical office visit, Dr. Gebhardt said. Instead of seeing 25 patients a day, he may see eight. “We will quickly go broke at this rate,” he said.
Although he said the small-business loans and advance Medicare payments are “a Godsend, and they will help us survive the next few months,” he also said practices like his need to go back to seeing patients in person if they are to remain viable. Medicare will no longer be advancing payments to providers, and many of the small-business funding represents a short-term fix.
While Medicare and some private insurers are covering virtual visits, which would include telephone calls, doctors say the payments do not make up for the lost revenue from tests and procedures that help them stay in business. “Telehealth is not the panacea and does not make up for all the financial losses,” said Dr. Patrice Harris, the president of the American Medical Association.
To keep the practices open, Dr. Mostashari and others propose doctors who treat Medicare and Medicaid patients receive a flat fee per person.
Even more worrisome, doctors’ groups may not be delivering care to those who need it, said Dr. Mehrotra, the Harvard researcher, because the practices are relying on patients to get in touch rather than reaching out.
Some doctors are already voicing concerns about patients who do not have access to a cellphone or computer or may not be adept at working with telemedicine apps. “Not every family has access to the technology to connect with us the right way,” said Dr. Kressly, who said the transition to virtual care “is making disparities worse.”
Some patients may also still prefer traditional office visits. While the Rutledges appreciated the need for virtual visits, Kelli said there was less time to “talk about other things.”
“Telehealth is more inclined to be about strictly what you are there for,” she said.
Private equity firms and large hospital systems are already eying many of these practices in hopes of buying them, said Paul D. Vanchiere, a consultant who advises pediatric practices.
“The vultures are circling here,” he said. “They know these practices are going to have financial hardship.”






%2Farc-anglerfish-washpost-prod-washpost%2FEAJ46XUOLMI6VEZCUKPHL374SM.jpg&w=908)