https://www.vox.com/2020/7/14/21324201/covid-19-long-term-effects-symptoms-treatment
/cdn.vox-cdn.com/uploads/chorus_image/image/67056715/GettyImages_1224443008.0.jpg)
People with long-term Covid-19 complications are meanwhile struggling to get care.
In late March, when Covid-19 was first surging, Jake Suett, a doctor of anesthesiology and intensive care medicine with the National Health Service in Norfolk, England, had seen plenty of patients with the disease — and intubated a few of them.
Then one day, he started to feel unwell, tired, with a sore throat. He pushed through it, continuing to work for five days until he developed a dry cough and fever. “Eventually, I got to the point where I was gasping for air literally doing nothing, lying on my bed.”
At the hospital, his chest X-rays and oxygen levels were normal — except he was gasping for air. After he was sent home, he continued to experience trouble breathing and developed severe cardiac-type chest pain.
Because of a shortage of Covid-19 tests, Suett wasn’t immediately tested; when he was able to get a test, 24 days after he got sick, it came back negative. PCR tests, which are most commonly used, can only detect acute infections, and because of testing shortages, not everyone has been able to get a test when they need one.
It’s now been 14 weeks since Suett’s presumed infection and he still has symptoms, including trouble concentrating, known as brain fog. (One recent study in Spain found that a majority of 841 hospitalized Covid-19 patients had neurological symptoms, including headaches and seizures.) “I don’t know what my future holds anymore,” Suett says.
Some doctors have dismissed some of his ongoing symptoms. One doctor suggested his intense breathing difficulties might be related to anxiety. “I found that really surprising,” Suett says. “As a doctor, I wanted to tell people, ‘Maybe we’re missing something here.’” He’s concerned not just for himself, but that many Covid-19 survivors with long-term symptoms aren’t being acknowledged or treated.
Suett says that even if the proportion of people who don’t eventually fully recover is small, there’s still a significant population who will need long-term care — and they’re having trouble getting it. “It’s a huge, unreported problem, and it’s crazy no one is shouting this from rooftops.”
In the US, a number of specialized centers are popping up at hospitals to help treat — and study — ongoing Covid-19 symptoms. The most successful draw on existing post-ICU protocols and a wide range of experts, from pulmonologists to psychiatrists. Yet even as care improves, patients are also running into familiar challenges in finding treatment: accessing and being able to pay for it.
What’s causing these long-term symptoms?
Scientists are still learning about the many ways the virus that causes Covid-19 impacts the body — both during initial infection and as symptoms persist.
One of the researchers studying them is Michael Peluso, a clinical fellow in infectious diseases at the University of California San Francisco, who is currently enrolling Covid-19 patients in San Francisco in a two-year study to study the disease’s long-term effects. The goal is to better understand what symptoms people are developing, how long they last, and eventually, the mechanisms that cause them. This could help scientists answer questions like how antibodies and immune cells called T-cells respond to the virus, and how different individuals might have different immune responses, leading to longer or shorter recovery times.
At the beginning of the Covid-19 pandemic, “the assumption was that people would get better, and then it was over,” Peluso says. “But we know from lots of other viral infections that there is almost always a subset of people who experience longer-term consequences.” He explains these can be due to damage to the body during the initial illness, the result of lingering viral infection, or because of complex immunological responses that occur after the initial disease.
“People sick enough to be hospitalized are likely to experience prolonged recovery, but with Covid-19, we’re seeing tremendous variability,” he says. It’s not necessarily just the sickest patients who experience long-term symptoms, but often people who weren’t even initially hospitalized.
That’s why long-term studies of large numbers of Covid-19 patients are so important, Peluso says. Once researchers can find what might be causing long-term symptoms, they can start targeting treatments to help people feel better. “I hope that a few months from now, we’ll have a sense if there is a biological target for managing some of these long-term symptoms.”
Lekshmi Santhosh, a physician lead and founder of the new post-Covid OPTIMAL Clinic at UCSF, says many of her patients are reporting the same kinds of problems. “The majority of patients have either persistent shortness of breath and/or fatigue for weeks to months,” she says.
Additionally, Timothy Henrich, a virologist and viral immunologist at UCSF who is also a principal investigator in the study, says that getting better at managing the initial illness may also help. “More effective acute treatments may also help reduce severity and duration of post-infectious symptoms.”
In the meantime, doctors can already help patients by treating some of their lingering symptoms. But the first step, Peluso explains, is not dismissing them. “It is important that patients know — and that doctors send the message — that they can help manage these symptoms, even if they are incompletely understood,” he says. “It sounds like many people may not be being told that.”
Long-term symptoms, long-term consequences
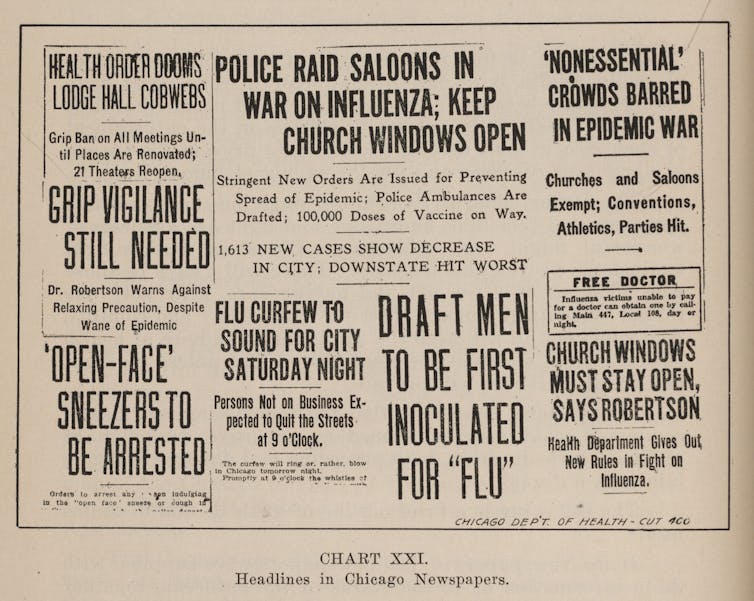
Even though we have a lot to learn about the specific damage Covid-19 can cause, doctors already know quite a bit about recovery from other viruses: namely, how complex and challenging a task long-term recovery from any serious infection can be for many patients.
Generally, it’s common for patients who have been hospitalized, intubated, or ventilated — as is common with severe Covid-19 — to have a long recovery. Being bed-bound can cause muscle weakness, known as deconditioning, which can result in prolonged shortness of breath. After a severe illness, many people also experience anxiety, depression, and PTSD.
A stay in the ICU not uncommonly leads to delirium, a serious mental disorder sometimes resulting in confused thinking, hallucinations, and reduced awareness of surroundings. But Covid-19 has created a “delirium factory,” says Santhosh at UCSF. This is because the illness has meant long hospital stays, interactions only with staff in full PPE, and the absence of family or other visitors.
Theodore Iwashyna, an ICU physician-scientist at the University of Michigan and VA Ann Arbor, is involved with the CAIRO Network, a group of 40 post-intensive care clinics on four continents. In general, after patients are discharged from ICUs, he says, “about half of people have some substantial new disability, and half will never get back to work. Maybe a third of people will have some degree of cognitive impairment. And a third have emotional problems.” And it’s common for them to have difficulty getting care for their ongoing symptoms after being discharged.
In working with Covid-19 patients, says Santhosh, she tells patients, “We believe you … and we are going to work on the mind and body together.”
Yet it’s currently impossible to predict who will have long-lasting symptoms from Covid-19. “People who are older and frailer with more comorbidities are more likely to have longer physical recovery. However, I’ve seen a lot of young people be really, really sick,” Santhosh says. “They will have a long tail of recovery too.”
Who can access care?
At the new OPTIMAL Clinic at UCSF, doctors are seeing patients who were hospitalized for Covid-19 at the UCSF health system, as well as taking referrals of other patients with persistent pulmonary symptoms. For ongoing cough and chest tightness, the clinic is providing inhalers, as well as pulmonary rehabilitation, including gradual aerobic exercise with oxygen monitoring. They’re also connecting patients with mental health resources.
“Normalizing those symptoms, as well as plugging people into mental health care, is really critical,” says Santhosh, who is also the physician lead and founder of the clinic. “I want people to know this is real. It’s not ‘in their heads.’”
Neeta Thakur, a pulmonary specialist at Zuckerberg San Francisco General Hospital and Trauma Center who has been providing care for Covid-19 patients in the ICU, just opened a similar outpatient clinic for post-Covid care. Thakur has also arranged a multidisciplinary approach, including occupational and physical therapy, as well as expedited referrals to neurology colleagues for rehabilitation for the muscles and nerves that can often be compressed when patients are prone for long periods in the ICU. But she’s most concerned by the cognitive impairments she’s seeing, especially as she’s dealing with a lot of younger patients.
These California centers join new post-Covid-19 clinics in major cities across the country, including Mount Sinai in New York and National Jewish Health Hospital in Denver. As more and more hospitals begin to focus on post-Covid care, Iwashyna suggests patients try to seek treatment where they were hospitalized, if possible, because of the difficulty in transferring sufficient medical records.
Santosh recommends that patients with persistent symptoms call their closest hospital, or nearest academic medical center’s pulmonary division, and ask if they can participate in any clinical trials. Many of the new clinics are enrolling patients in studies to try to better understand the long-term consequences of the disease. Fortunately, treatment associated with research is often free, and sometimes also offers financial incentives to participants.
But otherwise, one of the biggest challenges in post-Covid-19 treatment is — like so much of American health care — being able to pay for it.
Outside of clinical trials, cost can be a barrier to treatment. It can be tricky to get insurance to cover long-term care, Iwashyna notes. After being discharged from an ICU, he says, “Recovery depends on [patients’] social support, and how broke they are afterward.” Many struggle to cover the costs of treatment. “Our patient population is all underinsured,” says Thakur, noting that her hospital works with patients to try to help cover costs.
Lasting health impacts can also affect a person’s ability to go back to work. In Iwashyna’s experience, many patients quickly run through their guaranteed 12 weeks of leave under the Family Medical and Leave Act, which isn’t required to be paid. Eve Leckie, a 39-year-old ICU nurse in New Hampshire, came down with Covid-19 on March 15. Since then, Leckie has experienced symptom relapses and still can’t even get a drink of water without help.
“I’m typing this to you from my bed, because I’m too short of breath today to get out,” they say. “This could disable me for the rest of my life, and I have no idea how much that would cost, or at what point I will lose my insurance, since it’s dependent on my employment, and I’m incapable of working.” Leckie was the sole wage earner for their five children, and was facing eviction when their partner “essentially rescued us,” allowing them to move in.
These long-term burdens are not being felt equally. At Thakur’s hospital in San Francisco, “The population [admitted] here is younger and Latinx, a disparity which reflects who gets exposed,” she says. She worries that during the pandemic, “social and structural determinants of health will just widen disparities across the board.” People of color have been disproportionately affected by the virus, in part because they are less likely to be able to work from home.
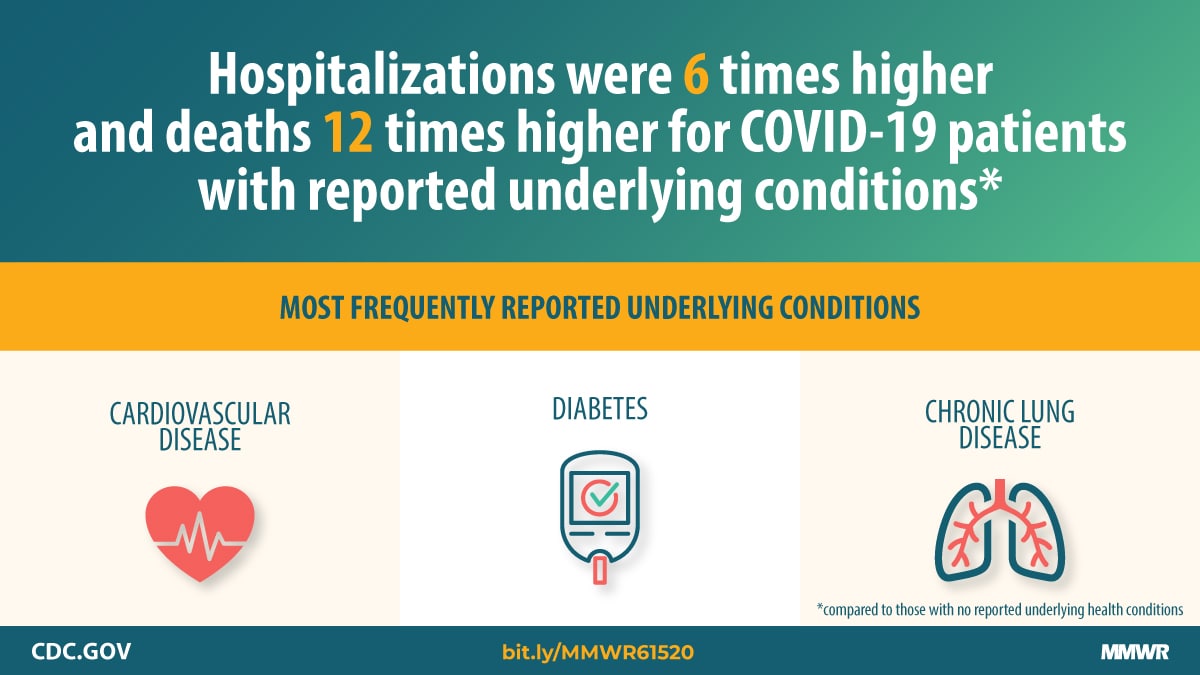
Black people are also more likely to be hospitalized if they get Covid-19, both because of higher rates of preexisting conditions — which are the result of structural inequality — and because of lack of access to health care.
“If you are more likely to be exposed because of your job, and likely to seek care later because of fear of cost, or needing to work, you’re more likely to have severe disease,” Thakur says. “As a result, you’re more likely to have long-term consequences. Depending on what that looks like, your ability to work and economic opportunities will be hindered. It’s a very striking example of how social determinants of health can really impact someone over their lifetime.”
If policies don’t support people with persistent symptoms in getting the care they need, ongoing Covid-19 challenges will deepen what’s already a clear crisis of inequality.
Iwashyna explains that a lot of extended treatment for Covid-19 patients is “going to be about interactions with health care systems that are not well-designed. The correctable problems often involve helping people navigate a horribly fragmented health care system.
“We can fix that, but we’re not going to fix that tomorrow. These patients need help now.”














/cdn.vox-cdn.com/uploads/chorus_image/image/67056715/GettyImages_1224443008.0.jpg)
