Cartoon – Acme Health Services


https://mailchi.mp/d953ea288786/newsletter031821-4639518?e=ad91541e82
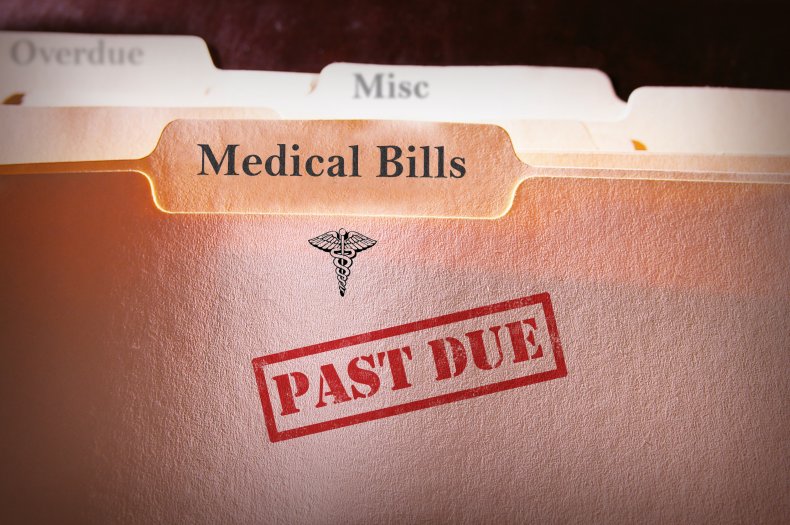
Medical debt can be a crushing burden for families, and it is a major problem in the United States. The nonprofit RIP Medical Debt says it’s wiped out debt for 2.7 million patients since 2014, totalling more than $4.5 billion. One of the most famous health policy studies ever conducted — the Oregon Health Insurance Experiment — found that having Medicaid coverage reduced a person’s likelihood of having an unpaid medical bill sent to collection by 25%. Now a study published last month in JAMA offers new evidence on the relationship between Medicaid and medical debt, and the scale of the country’s medical debt problem.
Using a subset of credit reports from one major U.S. credit agency for every year between 2009 and 2020, researchers Raymond Kluender, Neale Mahoney, Francis Wong and Wesley Yin looked at the total amount of medical debt and new medical debt each year. They found that while both measures of medical debt have decreased almost every year since 2014, nearly 1 in 5 Americans were under collections for medical debt as of early 2020. They also found that since 2014, medical debt has been the largest source of debt for Americans, surpassing all other types of debt — credit cards, personal loans, utilities and phone bills — combined. And the medical debt was not evenly distributed around the country. Approximately, 1 in 4 individuals in the South were under collection for medical debt in 2020, but only 1 in 10 in the Northeast.
To assess the impact of Medicaid coverage on medical debt, Kluender and colleagues compared the total amount of new debt accrued by people living in states that expanded Medicaid and those that have not between 2009 and 2020, allowing them to confirm that any trends they identified didn’t pre-date Medicaid expansion in 2014. They found that between 2013 and 2020 the average amount of new medical debt decreased 34 percentage points more in states that expanded in 2014 compared to non-expansion states, and the drops were most prominent in the lowest income zip codes. The analysis can’t prove a causal relationship between medical debt and Medicaid expansion, but interestingly, the authors found no statistically significant difference in nonmedical debt between expansion and non-expansion states. This lack of an effect on nonmedical debt supports the association between Medicaid and reductions in medical debt.
The article does have limitations: It doesn’t include debts paid on a credit card or through payment plans; it doesn’t reflect the impact of COVID-19; and it can’t account for unobservable changes in policy or circumstance that might have coincided with Medicaid expansion and impacted medical debt. But it does add evidence to support the value of Medicaid coverage — a particularly timely finding, with more than 11 million people joining Medicaid since the start of the pandemic and Democrats in Congress looking to cover the more than 2 million people in the so-called coverage gap in the 12 non-expansion states.

Collection agencies held $140 billion in unpaid medical debt in 2020, according to a study published July 20 in JAMA.
Researchers examined a nationally representative panel of consumer credit reports between January 2009 and June 2020. Below are four other notable findings from their report.




Just as other industries are rolling back some consumer-friendly changes made early in the pandemic — think empty middle seats on airplanes — so, too, are health insurers.
Many voluntarily waived all deductibles, copayments and other costs for insured patients who fell ill with covid-19 and needed hospital care, doctor visits, medications or other treatment.
Setting aside those fees was a good move from a public relations standpoint. The industry got credit for helping customers during tough times. And it had political and financial benefits for insurers, too.
But nothing lasts forever.
Starting at the end of last year — and continuing into the spring — a growing number of insurers are quietly ending those fee waivers for covid treatment on some or all policies.
“When it comes to treatment, more and more consumers will find that the normal course of deductibles, copayments and coinsurance will apply,” said Sabrina Corlette, research professor and co-director of the Center on Health Insurance Reforms at Georgetown University.
Even so, “the good news is that vaccinations and most covid tests should still be free,” added Corlette.
That’s because federal law requires insurers to waive costs for covid testing and vaccination.
Guidance issued early in President Joe Biden’s term reinforced that Trump administration rule about waiving cost sharing for testing and said it applies even in situations in which an asymptomatic person wants a test before, say, visiting a relative.
But treatment is different.
Insurers voluntarily waived those costs, so they can decide when to reinstate them.
Indeed, the initial step not to charge treatment fees may have preempted any effort by the federal government to mandate it, said Cynthia Cox, a vice president at KFF and director for its program on the Affordable Care Act.
In a study released in November, researchers found about 88% of people covered by insurance plans — those bought by individuals and some group plans offered by employers — had policies that waived such payments at some point during the pandemic, said Cox, a co-author. But many of those waivers were expected to expire by the end of the year or early this year.
Some did.
Anthem, for example, stopped them at the end of January. UnitedHealth, another of the nation’s largest insurers, began rolling back waivers in the fall, finishing up by the end of March. Deductible-free inpatient treatment for covid through Aetna expired Feb. 28.
A few insurers continue to forgo patient cost sharing in some types of policies. Humana, for example, has left the cost-sharing waiver in place for Medicare Advantage members, but dropped it Jan. 1 for those in job-based group plans.
Not all are making the changes.
For example, Premera Blue Cross in Washington and Sharp Health Plan in California have extended treatment cost waivers through June. Kaiser Permanente said it is keeping its program in place for members diagnosed with covid and has not set an end date. Meanwhile, UPMC in Pittsburgh planned to continue to waive all copayments and deductibles for in-network treatment through April 20.
What It All Means
Waivers may result in little savings for people with mild cases of covid that are treated at home. But the savings for patients who fall seriously ill and wind up in the hospital could be substantial.
Emergency room visits and hospitalization are expensive, and many insured patients must pay a portion of those costs through annual deductibles before full coverage kicks in.
Deductibles have been on the rise for years. Single-coverage deductibles for people who work for large employers average $1,418, while those for employees of small firms average $2,295, according to a survey of employers by KFF. (KHN is an editorially independent program of KFF.)
Annual deductibles for Affordable Care Act plans are generally higher, depending on the plan type.
Both kinds of coverage also include copayments, which are flat-dollar amounts, and often coinsurance, which is a percentage of the cost of office visits, hospital stays and prescription drugs.
Ending the waivers for treatment “is a big deal if you get sick,” said Robert Laszewski, an insurance industry consultant in Maryland. “And then you find out you have to pay $5,000 out-of-pocket that your cousin didn’t two months ago.”
Costs and Benefits
Still, those patient fees represent only a slice of the overall cost of caring for a hospitalized patient with covid.
While it helped patients’ cash flow, insurers saw other kinds of benefits.
For one thing, insurers recognized early on that patients — facing stay-at-home orders and other restrictions — were avoiding medical care in droves, driving down what insurers had to fork out for care.
“I think they were realizing they would be reporting extraordinarily good profits because they could see utilization dropping like a rock,” said Laszewski. “Doctors, hospitals, restaurants and everyone else were in big trouble. So, it was good politics to waive copays and deductibles.”
Besides generating goodwill, insurers may benefit in another way.
Under the ACA, insurers are required to spend at least 80% of their premium revenue on direct health care, rather than on marketing and administration. (Large group plans must spend 85%.)
By waiving those fees, insurers’ own spending went up a bit, potentially helping offset some share of what are expected to be hefty rebates this summer. That’s because insurers whose spending on direct medical care falls short of the ACA’s threshold must issue rebates by Aug. 1 to the individuals or employers who purchased the plans.
A record $2.5 billion was rebated for policies in effect in 2019, with the average rebate per person coming in at about $219.
Knowing their spending was falling during the pandemic helped fuel decisions to waive patient copayments for treatment, since insurers knew “they would have to give this money back in one form or another because of the rebates,” Cox said.
It’s a mixed bag for consumers.
“If they completely offset the rebates through waiving cost sharing, then it strictly benefits only those with covid who needed significant treatment,” noted Cox. “But, if they issue rebates, there’s more broad distribution.”
Even with that, insurers can expect to send a lot back in rebates this fall.
In a report out this week, KFF estimated that insurers may owe $2.1 billion in rebates for last year’s policies, the second-highest amount issued under the ACA. Under the law, rebate amounts are based on three years of financial data and profits. Final numbers aren’t expected until later in the year.
The rebates “are likely driven in part by suppressed health care utilization during the COVID-19 pandemic,” the report says.
Still, economist Joe Antos at the American Enterprise Institute says waiving the copays and deductibles may boost goodwill in the public eye more than rebates. “It’s a community benefit they could get some credit for,” said Antos, whereas many policyholders who get a small rebate check may just cash it and “it doesn’t have an impact on how they think about anything.”
https://mailchi.mp/da8db2c9bc41/the-weekly-gist-april-23-2021?e=d1e747d2d8
Given regulatory barriers and structural differences in practice, private equity firms have been slow to acquire and roll up physician practices and other care assets in other countries in the same way they’ve done here in the US. But according a fascinating piece in the Financial Times, investors have targeted a different healthcare segment, one ripe for the “efficiencies” that roll-ups can bring—small veterinary practices in the UK and Ireland.
British investment firm IVC bought up hundreds of small vet practices across the UK, only to be acquired itself by Swedish firm Evidensia, which is now the largest owner of veterinary care sites, with more than 1,500 across Europe. Vets describe the deals as too good to refuse: one who sold his practice to IVC said “he ‘almost fell off his chair’ on hearing how much it was offering. The vet, who requested anonymity, says IVC mistook his shock for hesitation—and increased its offer.” (Physician executives in the US, take note.) IVC claims that its model provides more flexible options, especially for female veterinarians seeking more work-life balance than offered by the typical “cottage” veterinary practice.
But consumers have complained of decreased access to care as some local clinics have been shuttered as a result of roll-ups. Meanwhile prices, particularly for pet medications like painkillers or feline insulin, have risen as much as 40 percent—and vets aren’t given leeway to offer the discounts they previously extended to low-income customers. And with IVC attaining significant market share in some communities (for instance, owning 17 of 32 vet practices in Birmingham), questions have arisen about diminished competition and even price fixing.
The playbook for private equity is consistent across human and animal healthcare: increase leverage, raise prices for care, and slash practice costs, all with little obvious value for consumers. It remains to be seen whether and how consumers will push back—either on behalf of their beloved pets, or for the sake of their own health.