https://www.bain.com/insights/getting-the-most-out-of-generative-ai-in-healthcare/

Generative AI applications can already help health systems improve margins, yet only 6% have a strategy ready.
At a Glance
- In the wake of their most challenging financial year since 2020, US hospitals are desperately searching for margin improvements.
- Generative AI can increase productivity and cost efficiency, but only 6% of health systems currently have a strategy.
- Leading providers and payers will start with highly focused, low-risk generative AI use cases, generating the funds and experience for more transformative future applications.
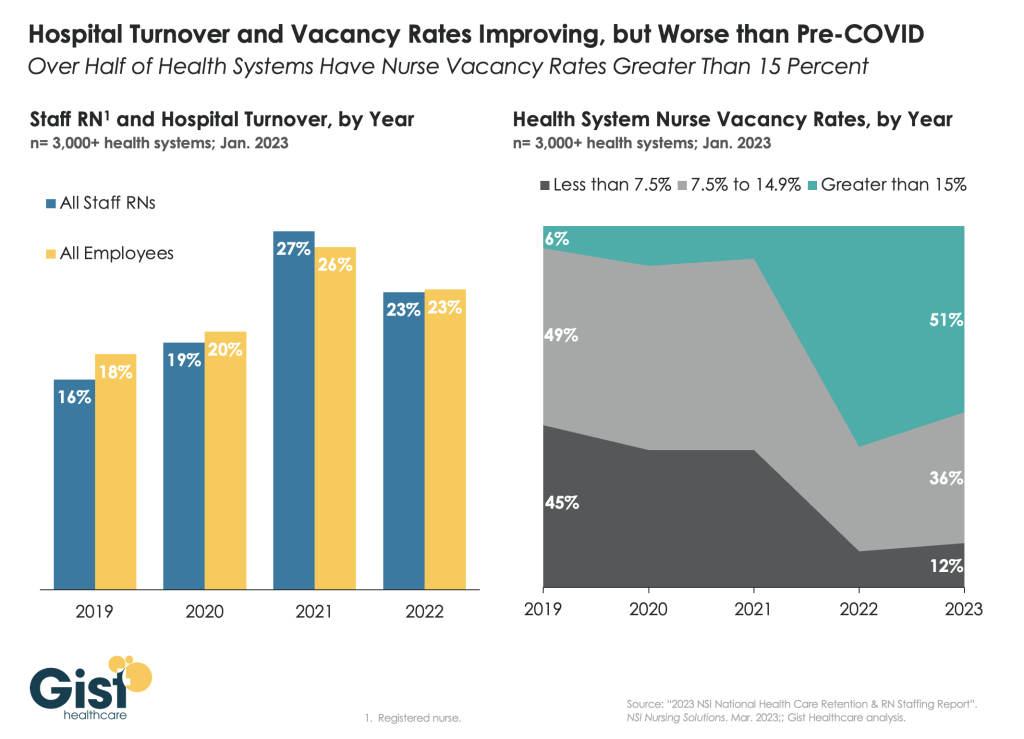
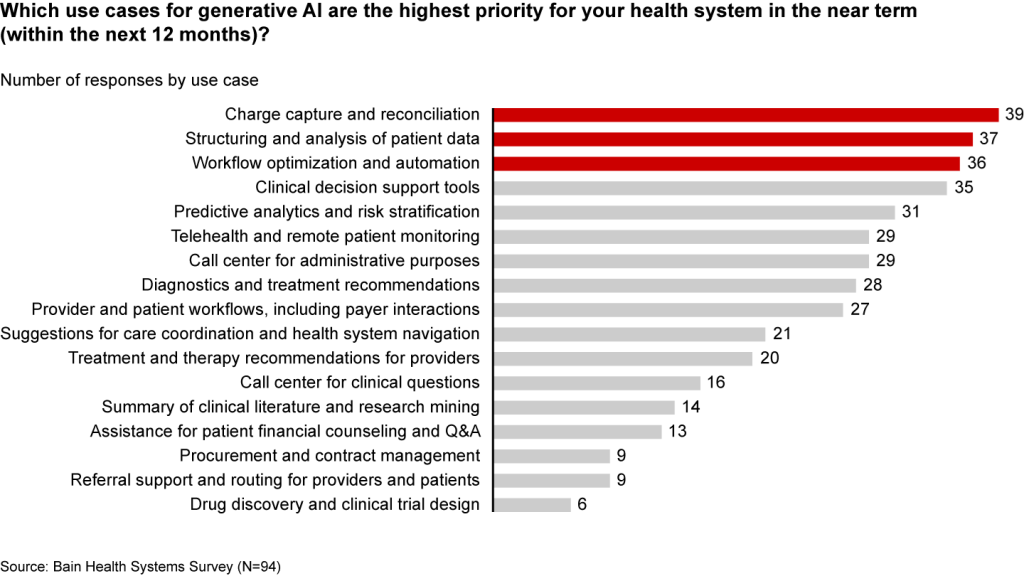
While Covid-19 may no longer be dominating the global news cycle, healthcare providers and payers are still feeling its reverberations. More than half of US hospitals ended 2022 with a negative margin, marking the most difficult financial year since the start of the pandemic.
CEOs and CFOs remember the challenges all too well: The Omicron surge halted nonurgent procedures in the first half of the year, government support tapered off, and labor expenses ballooned amid staffing shortages. There was also the record-high inflation that continues to intensify margin pressures today. According to a recent Bain survey of health system executives, 60% cite rising costs as their greatest concern.
Payers and providers are now on the hunt for margin improvements. In our experience, the most successful companies won’t merely reduce costs, but also ramp up productivity. When done right, modest technology investments can accomplish both.
Artificial intelligence (AI) may hold part of the answer. With the costs to train a system down 1,000-fold since 2017, AI provides an arsenal of new productivity-enhancing tools at a low investment.
Many executives recognize the growing opportunity, especially with the recent rise of generative AI, which uses sophisticated large language models (LLMs) to create original text, images, and other content. It’s inspiring an explosion of ideas around use cases, from reviewing medical records for accuracy to making diagnoses and treatment recommendations.
Our survey reveals that 75% of health system executives believe generative AI has reached a turning point in its ability to reshape the industry. However, only 6% have an established generative AI strategy.
It’s time to play offense—or be forced to play defense later. But choosing from the laundry list of generative AI applications is daunting. Companies are at high risk of overinvesting in the wrong opportunities and underinvesting in the right ones, undermining future profitability, growth, and value creation. A wait-and-see approach is a tempting prospect.
However, we believe the next generation of leading healthcare companies will start today, with highly focused, low-risk use cases that boost productivity and cost efficiency. Over the next three to nine months, these companies will improve margins and learn how to implement a generative AI strategy, building up the funds and experience needed to invest in a more transformative vision.
Endless potential—and high hurdles
The excitement around generative AI may feel akin to the hype around other recent digital and technology developments that never quite rose to their promised potential. Well-intentioned, well-informed individuals are debating how much change will truly materialize in the next few years. While developments over the past six months have been a testament to the breakneck speed of change, nobody can accurately predict what the next six months, year, or decade will look like. Will new players emerge? Will we rely on different LLMs for different use cases, or will one dominate the landscape?
Despite the uncertainty, generative AI already has the power to alleviate some of providers’ biggest woes, which include rising costs and high inflation, clinician shortages, and physician burnout. Quick relief is critical, considering that the heightened risk of a recession will only compound margin pressures, and the US could be short 40,800 to 104,900 physicians by 2030, according to the Association of American Medical Colleges.
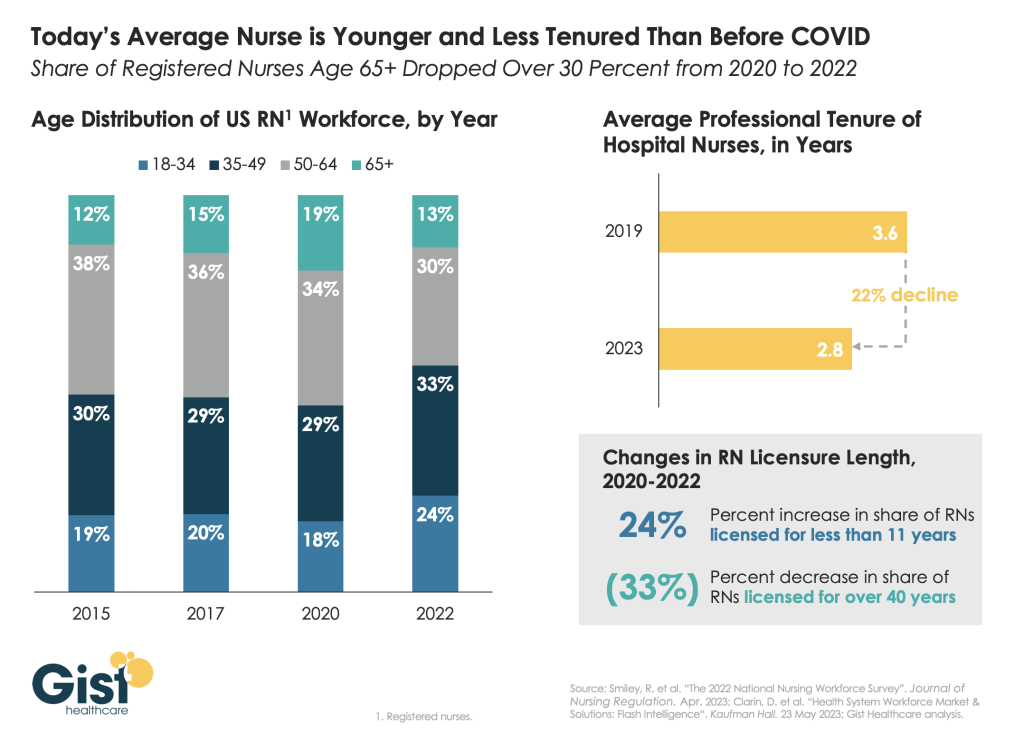
Many health systems are eyeing imminent opportunities to reduce administrative burdens and enhance operational efficiency. They rank improving clinical documentation, structuring and analyzing patient data, and optimizing workflows as their top three priorities (see Figure 1).
Figure 1
In the near term, generative AI can reduce administrative burdens and enhance efficiency
Some generative AI applications are already streamlining administrative tasks and allowing thinly stretched physicians to spend more time with patients. For instance, Doximity is rolling out a ChatGPT tool that can draft preauthorization and appeal letters. HCA Healthcare partnered with Parlance, a conversational AI-based switchboard, to improve its call center experience while reducing operators’ workload. And there are new announcements seemingly every week: Consider how healthcare software company Epic Systems is incorporating ChatGPT with electronic health records (EHRs) to draft response messages to patients, or how Google Cloud is launching an AI-enabled Claims Acceleration Suite for prior authorization processing.
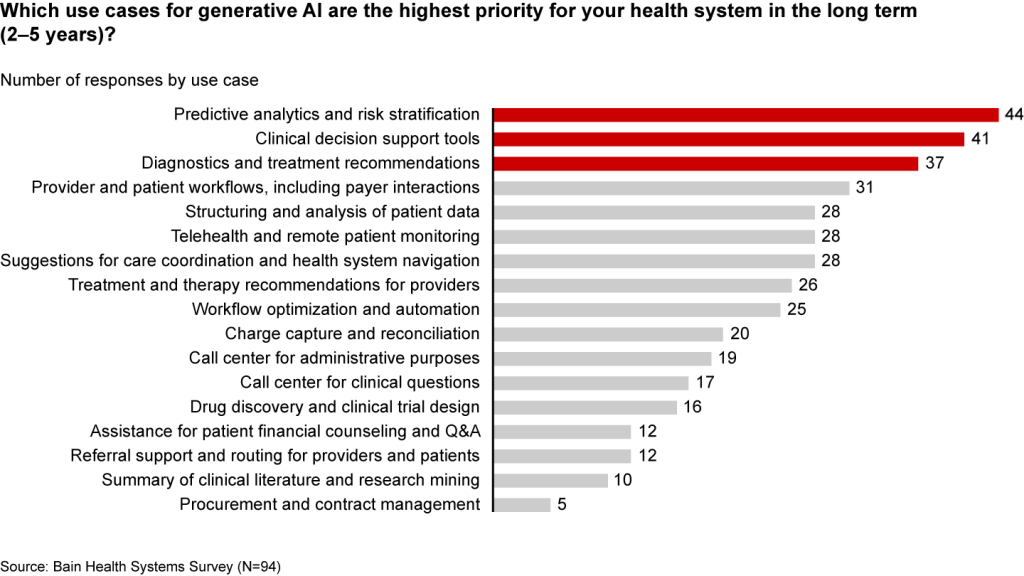
These applications only scratch the surface of potential. In the future, generative AI could profoundly transform care delivery and patient outcomes. Looking ahead two to five years, executives are most interested in predictive analytics, clinical decision support, and treatment recommendations (see Figure 2).
Figure 2
Predictive analytics, clinical decisions, and care recommendations are long-term generative AI priorities
It’s hard not to catch AI “fever.” But there are real challenges ahead. Some are already tackling the biggest questions: Organizations such as Duke Health, Stanford Medicine, Google, and Microsoft have formed the Coalition for Health AI to create guidelines for responsible AI systems. Even so, solutions to the greatest hurdles aren’t yet keeping up with the rapid technology development.
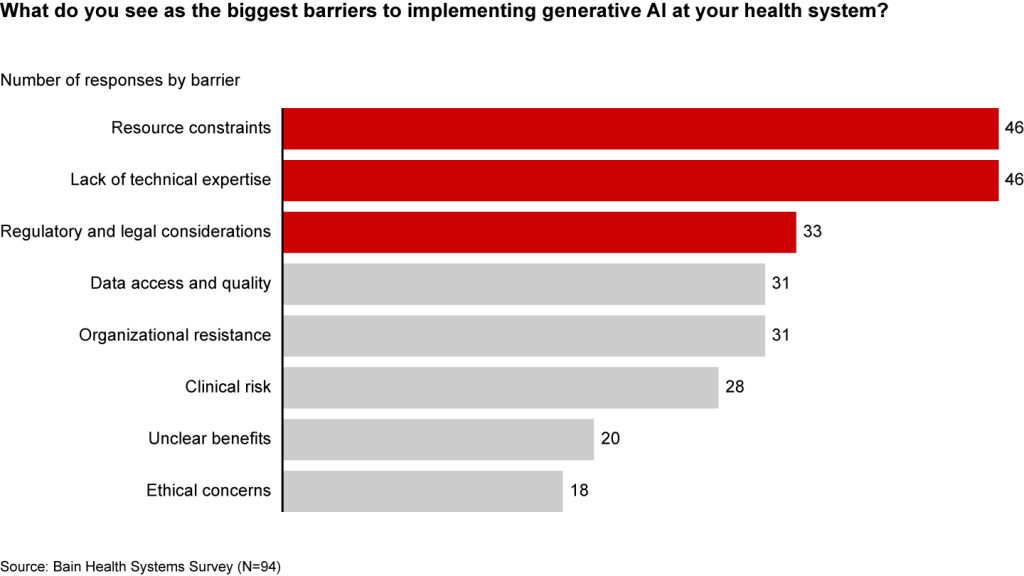
Resource and cost constraints, a lack of expertise, and regulatory and legal considerations are the largest barriers to implementing generative AI, according to executives (see Figure 3).
Figure 3
A lack of resources, expertise, and regulation are the biggest barriers to generative AI in healthcare
Even when organizations can overcome these hurdles, one major challenge remains: focus and prioritization. In many boardrooms, executives are debating overwhelming lists of potential generative AI investments, only to deem them incomplete or outdated given the dizzying pace of innovation. These protracted debates are a waste of precious organizational energy—and time.
Starting small to win big
Setting the bar too high is setting up for failure. It’s easy to get caught up, betting big on what seems like the greatest opportunity in the moment. But 12 months later, leaders often find themselves frustrated that they haven’t seen results or feeling as if they’ve made a misplaced bet. Momentum and investments slow, further hindering progress.
Leading companies are forming a more pragmatic strategy that considers current capabilities, regulations, and barriers to adoption. Their CEOs and CFOs work together to enforce four guiding principles:
- Pilot low-risk applications with a narrow focus first. Tomorrow’s leaders are making no-regret moves to deliver savings and productivity enhancements in short order—at a time when they need it most. Gaining experience with currently available technology, they are testing and learning their way to minimum viable products in low-risk, repeatable use cases. These quick wins are typically in areas where they already have the right data, can create tight guardrails, and see a strong potential return on investment. Some, like call center and chatbot support, can improve the patient experience. However, given the current challenges around regulation and compliance, the most successful early initiatives are likely to be internally focused, such as billing or scheduling. Most importantly, executives prioritize initiatives by potential savings, value, and cost.
- Decide to buy, partner, or build. CEOs will need to think about how to invest in different use cases based on availability of third-party technology and importance of the initiative.
- Funnel cost savings and experience into bigger bets. As the technology matures and the value becomes clear, companies that generate savings, accumulate experience, and build organizational buy-in today will be best positioned for the next wave of more sophisticated, transformative use cases. These include higher-risk clinical activities with a greater need for accuracy due to ethical and regulatory considerations, such as clinical decision support, as well as administrative activities that require third-party integration, such as prior authorization.
- Remember generative AI isn’t a strategy unto itself. To build a true competitive advantage, top CEOs and CFOs are selective and discerning, ensuring that every generative AI initiative reinforces and enables their overarching goals.
Some health systems are already seeing powerful results from relatively small, more practical investments. For instance, recognizing that clinicians were spending an extra 130 minutes per day outside of working hours on administrative tasks, the University of Kansas Health System partnered with Abridge, a generative AI platform, to reduce documentation burden. By summarizing the most important points from provider-patient conversations, Abridge is improving the quality and consistency of documentation, getting more patients in the door, and cutting down on pervasive physician burnout.
Although it will require some upfront investment, in the long run it will be more costly to underestimate the level and speed at which generative AI will transform healthcare. The next generation of leaders will start testing, learning, and saving today, putting them on a path to eventually revolutionize their businesses.