https://thehill.com/policy/healthcare/494792-us-surpasses-1-million-covid-19-cases

More than a million people in the United States have tested positive for the coronavirus, a sobering milestone that experts say represents only the beginning of a months-long battle to end the pandemic.
The United States has now registered about a third of all confirmed cases of COVID-19 around the globe, according to data compiled by the Center for Systems Science and Engineering at Johns Hopkins University. More than 57,000 people have died in the United States, about a quarter of the known COVID-19 deaths around the globe.
The United States has now registered more confirmed cases than the next five countries suffering the largest outbreaks — Spain, Italy, France, Germany and the United Kingdom — combined.
Those numbers are partly a reflection of population, but there are troubling signs for the United States.
While those countries have reduced the pace of transmission and the growth in the number of new cases they are seeing on a daily basis, the United States has not similarly bent the curve.
Instead, it is stuck at a deadly plateau: In the last week, the U.S. has reported between 24,000 and 41,000 new cases a day, and between 1,200 and 2,600 deaths per day, according to The Covid Tracking Project, a group of researchers who keep tallies of case counts around the country.

Even as some states begin to relax orders that closed retail and service stores, experts warned the country is still at risk of a new rush of cases, and that the downslope of declining case counts will be much longer than the sudden surge the United States saw in April.
“We’re in the opening stages of this,” said Michael Osterholm, director of the Center for Infectious Disease Research and Prevention at the University of Minnesota. States “are not in the mountains, they’re in the foothills. The mountains are still to come.”
More than a quarter million residents of New York have tested positive for the virus, and commuter suburbs in New Jersey and Connecticut have reported tens of thousands of cases. More than 50,000 residents of Massachusetts have tested positive, and California, Illinois and Pennsylvania have all confirmed more than 40,000 cases.
There are growing signs that the virus is shifting into new, more rural territory. States like Arkansas, Kansas, Minnesota, Nebraska, New Mexico, Rhode Island, Tennessee and Virginia all recorded substantial growth in the number of new cases they had confirmed in the last few days.
That pattern of viral spread beginning in large urban cores and eventually making its way to rural areas is typical, experts said, given societal connections between urban areas, suburbs and more rural areas.
“Epidemiologists know that this pattern is a very expectable one, that rural areas are going to have lagged waves of cases. So we’ve been bracing for that,” said Nita Bharti, a biologist at the Center for Infectious Disease Dynamics at Penn State University. “What they’re experiencing now is what cities have been seeing. It’s the same, it’s just delayed, and we knew it would happen.”
About six months after the coronavirus outbreak was detected in Wuhan, China, and four months after the first case arrived on American shores, the United States still lags the world in testing capacity. States have bolstered their capacity in recent days, conducting more than 225,000 tests per day over four of the last five days, the capacity needed to ensure the virus can be brought under control lags substantially.
An analysis by Harvard researchers for the scientific publication STAT found more than half of states would have to significantly bolster their testing capacity in order to safely begin easing stay-at-home orders in May. The hardest-hit state, New York, will have to be able to test at least 100,000 more people every day than it is currently able to; New Jersey’s capacity would need to increase by 68,000 a day.
Smaller states and those that have yet to experience thousands of new cases — places like Mississippi, Idaho, Montana, Wyoming, Arizona and New Mexico — already have the testing capacity they need to identify and squelch any new viral hotspots. Even Washington state, the first state to confirm a positive case, has built its capacity to meet demand.
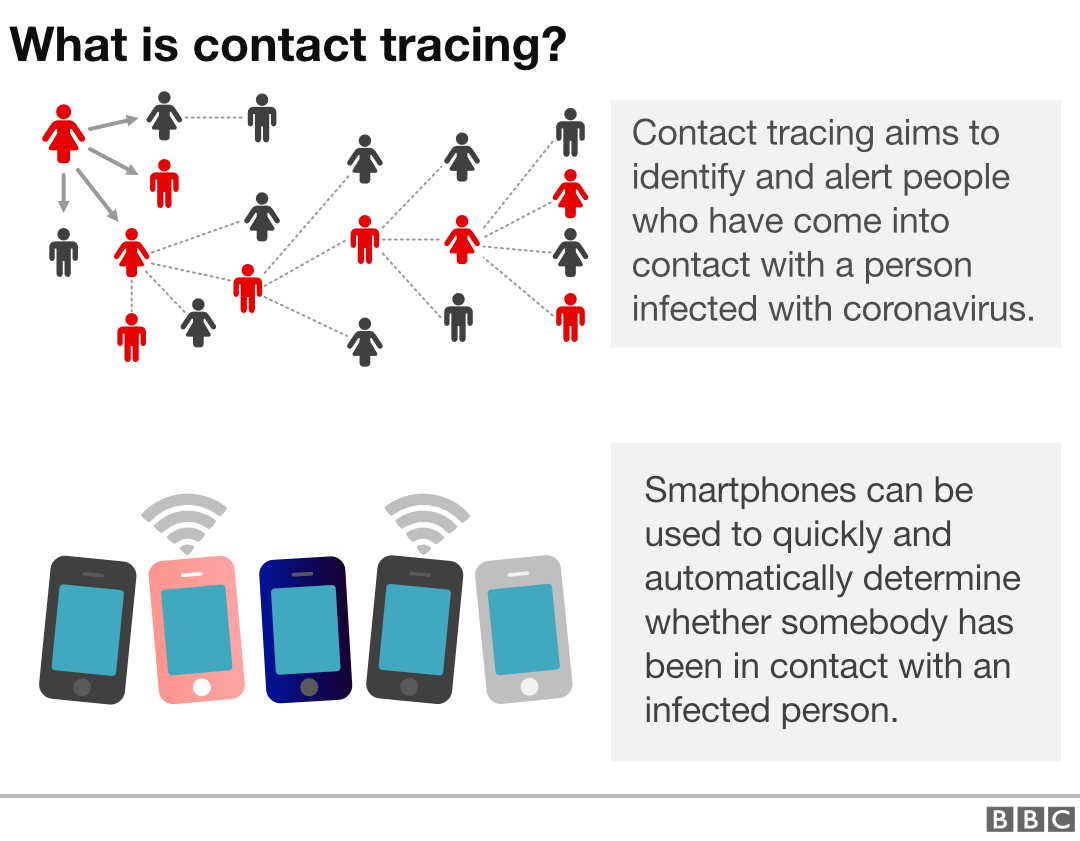
Public health experts say a robust testing program must be supplemented by armies of contact tracers who can track down those who are at risk of contracting the virus.
Already, Massachusetts has partnered with the nonprofit Partners In Health to deploy about 1,000 contact tracers across the state. Alaska has managed to trace the contacts of each of its 341 positive cases. New York City Mayor Bill de Blasio said Monday that the city would hire 1,000 contact tracers of its own, and former Mayor Mike Bloomberg has pledged $10 million to kick start a contact tracing program in the tri-state area.
On Monday, a bipartisan group of top public health experts led by President Trump‘s former FDA commissioner Scott Gottlieb and President Obama’s former Centers for Medicare and Medicaid Services administrator Andy Slavitt called on Congress to spend $46 billion to expand contact tracing capacity, including $12 billion to hire 180,000 new workers.
It is unclear how the outbreak in the United States compares with outbreaks in authoritarian countries like China, Russia and Iran, which do not report reliable numbers.
But even in the United States, where state and local governments are transparent about the data they collect, the actual number of cases and deaths are higher — likely significantly so. Early antibody tests in places like New York City and Miami show a significant number of people contract the virus without showing symptoms, and as studies show people who died inexplicably over the last several months tested positive for the virus.