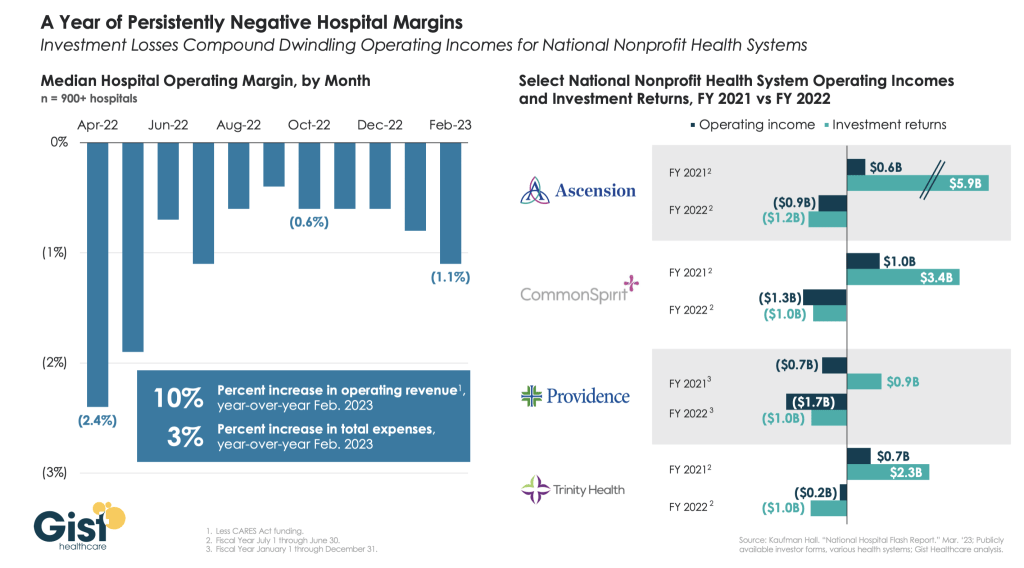
For the first time in recent history, we saw all three
functions of the not-for-profit healthcare system’s
financial structure suffer significant and sustained
dislocation over the course of the year 2022
(Figure above).
The headwinds disrupting these functions
are carrying over into 2023, and it is uncertain how
long they will continue to erode the operating and
financial performance of not-for-profit hospitals
and health systems.
The Operating Function is challenged by elevated
expenses, uncertain recovery of service volumes, and
an escalating and diversified competitive environment.
The Finance Function is challenged by a more
difficult credit environment (all three rating agencies
now have a negative perspective on the not-forprofit healthcare sector), rising rates for debt, and
a diminished investor appetite for new healthcare
debt issuance. Total healthcare debt issuance in
2022 was $28 billion, down sharply from a trailing
two-year average of $46 billion.
The Investment Function is challenged by volatility and
heightened risk in markets concerned with the Federal
Reserve’s tightening of monetary policy and the
prospect of a recession. The S&P 500—a major stock
index—was down almost 20% in 2022. Investments
had served as a “resiliency anchor” during the first
two years of the pandemic; their ability to continue
to serve that function is now in question.
A significant factor in Operating Function challenges is
labor: both increases in the cost of labor and staffing
shortages that are forcing many organizations to
run at less than full capacity. In Kaufman Hall’s 2022
State of Healthcare Performance Improvement Survey, for
example, 67% of respondents had seen year-over-year
increases of more than 10% for clinical staff wages,
and 66% reported that they had run their facilities at
less-than-full capacity because of staffing shortages.
These are long-term challenges,
dependent in part on
increasing the pipeline of new talent entering healthcare
professions, and they will not be quickly resolved.
Recovery of returns from the Investment Function
is similarly uncertain. Ideally, not-for-profit health
systems can maintain a one-way flow of funds into
the Investment Function, continuing to build the
basis that generates returns. Organizations must now
contemplate flows in the other direction to access
funds needed to cover operating losses, which in
many cases would involve selling invested assets at a
loss in a down market and reducing the basis available
to generate returns when markets recover.
The current situation demonstrates why financial
reserves are so important:
many not-for-profit
hospitals and health systems will have to rely on
them to cover losses until they can reach a point
where operations and markets have stabilized, or
they have been able to adjust their business to a
new, lower margin environment. As noted above,
relief funding and the MAAP program helped bolster
financial reserves after the initial shock of the
pandemic. As the impact of relief funding wanes
and organizations repay remaining balances under
the MAAP program, Days Cash on Hand has begun
to shrink, and the need to cover operating losses is
hastening this decline. From its highest
point in 2021, Days Cash on Hand had decreased, as
of September 2022, by:
29% at the 75th percentile, declining from 302 to 216
DCOH (a drop of 86 days)
28% at the 50th percentile, declining from 202 to 147
DCOH (a drop of 55 days)
49% at the 25th percentile, declining from 67 to 34
DCOH (a drop of 33 days)
Financial reserves are playing the role
for which they were intended; the only
question is whether enough not-for-profit
hospitals and health systems have built
sufficient reserves to carry them through
what is likely to be a protracted period of
recovery from the pandemic.
KEY TAKEAWAYS
All three functions of the not-for-profit healthcare
system’s financial structure—operations, finance,
and investments—suffered significant and
sustained dislocation over the course of 2022.
These headwinds will continue to challenge not-forprofit
hospitals and health systems well into 2023.
Days Cash on Hand is showing a steady decline, as
the impact of relief funding recedes and the need
to cover operating losses persists.
Financial reserves are playing a critical role in
covering operating losses as hospitals and health
systems struggle to stabilize their operational and
financial performance.
Conclusion
Not-for-profit hospitals and health systems serve
many community needs. They provide patients
access to healthcare when and where they need it.
They invest in new technologies and treatments that
offer patients and their families lifesaving advances
in care. They offer career opportunities to a broad
range of highly skilled professionals, supporting the
economic health of the communities they serve.
These services and investments are expensive and
cannot be covered solely by the revenue received
from providing care to patients.
Strong financial reserves are the foundation of good
financial stewardship for not-for-profit hospitals and
health systems.
Financial reserves help fund needed
investments in facilities and technology, improve an
organization’s debt capacity, enable better access to
capital at more affordable interest rates, and provide a
critical resource to meet expenses when organizations
need to bridge periods of operational disruption or
financial distress.
Many hospitals and health systems today are relying
on the strength of their reserves to navigate a difficult
environment; without these reserves, they would
not be able to meet their expenses and would be at
risk of closure.
Financial reserves, in other words,
are serving the very purpose for which they are
intended—ensuring that hospitals and health systems
can continue to serve their communities in the face of
challenging operational and financial headwinds.
When these headwinds have subsided, rebuilding these
reserves should be a top priority to ensure that our
not-for-profit hospitals and health systems can remain
a vital resource for the communities they serve.