
Category Archives: 2028 Election Issues
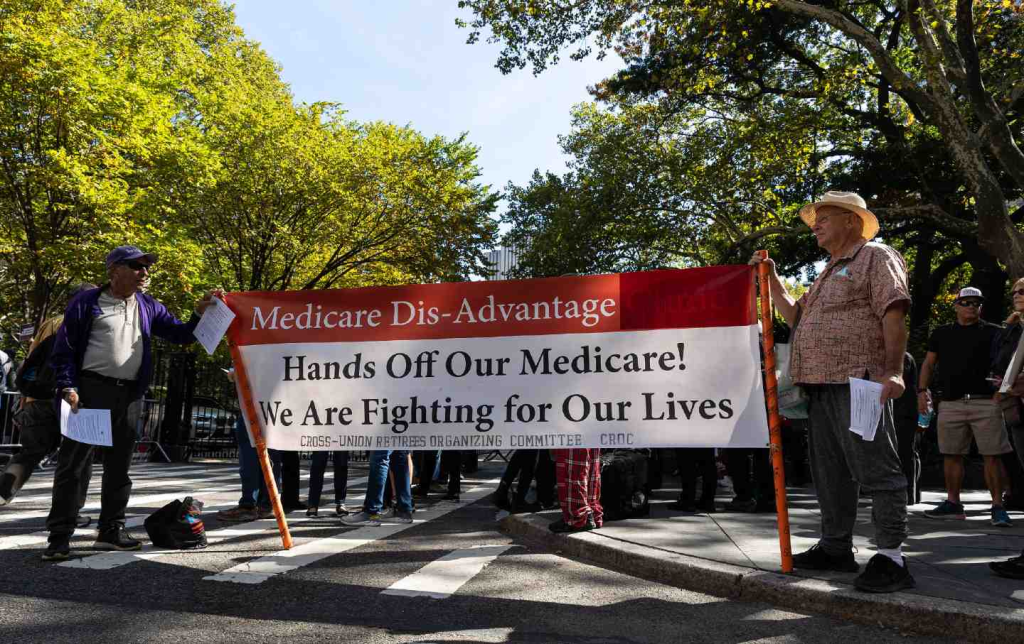
What’s at stake from GOP megabill’s coverage losses
https://www.axios.com/2025/07/01/real-cost-health-coverage-losses
Nearly 12 million people would lose their health insurance under President Trump’s “big, beautiful bill,” an erosion of the social safety net that would lead to more unmanaged chronic illnesses, higher medical debt and overcrowding of hospital emergency departments.
Why it matters:
The changes in the Senate version of the bill could wipe out most of the health coverage gains made under the Affordable Care Act and slash state support for Medicaid and SNAP.
- “We are going back to a place of a lot of uncompensated care and a lot of patchwork systems for people to get care,” said Ellen Montz, a managing director at Manatt Health who oversaw the ACA federal marketplace during the Biden administration.
The big picture:
The stakes are huge for low-income and working-class Americans who depend on Medicaid and subsidized ACA coverage.
- Without health coverage, more people with diabetes, heart disease, asthma and other chronic conditions will likely go without checkups and medication to keep their ailments in check.
- Those who try to keep up with care after losing insurance will pay more out of pocket, driving up medical debt and increasing the risk of eviction, food insecurity and depleted savings.
- Uninsured patients have worse cancer survival outcomes and are less likely to get prenatal care. Medicaid also is a major payer of behavioral health counseling and crisis intervention.
Much of the coverage losses from the bill will come from new Medicaid work reporting requirements, congressional scorekeepers predict. Work rules generally will have to be implemented for coverage starting in 2027, but could be earlier or later depending on the state.
- Past experiments with Medicaid work rules show that many eligible people fall through the cracks verifying they’ve met the requirements or navigating new state bureaucracies.
- Often, people don’t find out they’ve lost coverage until they try to fill a prescription or see their doctor. States typically provide written notices, but contacts can be out of date.
- Nearly 1 in 3 adults who were disenrolled from Medicaid after the COVID pandemic found out they no longer had health insurance only when they tried to access care, per a KFF survey.
Zoom out:
The Medicaid and ACA changes will also affect people who keep their coverage.
- The anticipated drop-off in preventive care means the uninsured will be more likely to go to the emergency room when they get sick. That could further crowd already bursting ERs, resulting in even longer wait times.
- Changes to ACA markets in the bill, along with the impending expiration of enhanced premium subsidies, may drive healthier people to drop out, Montz said, skewing the risk pool and driving up premiums for remaining enrollees.
- States will likely have to make further cuts to their safety-net programs if the bill passes in order to keep state budgets functioning with less federal Medicaid funding.
The other side:
The White House and GOP proponents of the bill say the health care changes will fight fraud, waste and abuse, and argue that coverage loss projections are overblown.
- Conservative health care thinkers also posit that there isn’t strong enough evidence that public health insurance improves health.
Reality check:
Not all insurance is created equally, and many people with health coverage still struggle to access care. But the bill’s impact would take the focus off ways to improve the health system, Montz said.
- “This is taking us catastrophically backward, where we don’t get to think about the things that we should be thinking about how to best keep people healthy,” she said.
The bottom line:
The changes will unfold against a backdrop of Health Secretary Robert F. Kennedy Jr.’s purported focus on preventive care and ending chronic illness in the U.S.
- But American health care is an insurance-based system, said Manatt Health’s Patricia Boozang. Coverage is what unlocks access.
- Scrapping millions of people’s health coverage “seems inconsistent with the goal of making America healthier,” she said.
The Summer of 2025 for U.S. Healthcare: What Organizations should Expect
Last Thursday, the Make America Healthy Again Commission released its 68-page report “Making America’s Children Healthy Again Assessment” featuring familiar themes—the inadequacy of attention to chronic disease by the health system, the “over-medicalization” of patient care vis a vis prescription medicines et al, the contamination of the food-supply by harmful ingredients, and more.
HHS Secretary Kennedy, EPA Administrator Zeldin and Agriculture Secretary Rollins pledged war on the corporate healthcare system ‘that has failed the public’ and an all-of-government approach to remedies for burgeoning chronic care needs.
Also Thursday, the House of Representatives passed its budget reconciliation bill by a vote of 215-214. The 1000-page bill cuts federal spending by $1.6 trillion (including $698 billion from Medicaid) and adds $2.3 trillion (CBO estimate/$3.4 to $5 trillion per Yale Budget Lab) to the national deficit over the next decade. It now goes to the Senate where changes to reduce federal spending to pre-pandemic level will be the focus.
With a 53-37 advantage and 22 of the 36 Senate seats facing mid-term election races in November, 2026, the Senate Republican version of the “Big Beautiful Bill” will include more spending cuts while pushing more responsibility to states for funding and additional cuts. The gap between the House and Senate versions will be wider than currently anticipated by House Republicans potentially derailing the White House promise of a final Big Beautiful Bill by July 4.
And, over the last week and holiday weekend, the President announced a new 25% tariff on Apple devices manufactured in India and new tariffs targeting the EU; threatened cuts to federal grants to Harvard and cessation of its non-citizen student enrollment, a ‘get-tougher’ policy on Russia to pressure an end of its Ukraine conflict, and a pledge to Americans on Memorial that it will double down on ‘peace thru strength’ in its Make America Great Again campaign.
These have 2 things in common:
1-They’re incomplete. None is a finished product.
The MAHA Commission, working with the Departments of Health & Human Services, Interior and Agriculture, is tasked to produce another report within 90 days to provide more details about a plan. The FY26 budgeting process is wrought with potholes—how to satisfy GOP deficit hawks vs. centrist lawmakers facing mid-term election, how to structure a bill that triggers sequestration cuts to Medicare (projected $490 billion/10 yrs. per CBO), how to quickly implement Medicaid work requirements and marketplace enrollment cuts that could leave insurance coverage for up to 14 million in limbo, and much more. And the President’s propensity to “flood the zone” with headline-grabbing Truth Social tweets, Executive Orders and provocative rhetoric on matters at home and abroad will keep media occupied and healthcare spending in the spotlight.
2-They play to the MAGA core.
The MAGA core is primarily composed of older, white, Christian men driven by a belief that the United States has lost its exceptionalism through WOKE policies i.e. DEI in workplaces and government, open borders, globalization and excessive government spending and control. In the 2024 Presidential election, the MAGA core expanded incrementally among Black, Hispanic, and younger voters whose concerns about food, energy and housing prices prompted higher-than expected turnout. The MAGA core believes in meritocracy, nationalism, smaller government, lower taxes, local control and free-market policies that encourage private investment in the economy. The core is price sensitive.
The health system per se is not a concern but it’s the affordability and lack of price transparency are. They respect doctors and frontline caregivers but think executives are overpaid and prone to self-promotion. And the MAGA core think lawmakers have been complicit in the system’s lack of financial accountability largely beneficial to elites.
Looking ahead to the summer, a “Big Beautiful Bill” will pass with optics that allow supporters to claim fiscal constraint and lower national debt and opponents to decry insensitive spending cuts and class warfare against low-and-middle-class households.
Federal cuts to Medicaid and SNAP (Supplemental Nutrition Assistance Program) will be prominent targets in both groups—one a portrayal of waste, fraud and abuse and the other tangible evidence of societal inequity and lack of moral purpose. Each thinks the other void of a balanced perspective. Each thinks the health system is underperforming and in need of transformational change but agreement about how to get there unclear.
As MAHA promotes its agenda, Congress passes a budget and MAGA advances its anti-establishment agenda vis a vis DOGE et al, healthcare operators will be in limbo. The dust will settle somewhat this summer, but longer-term bets will be modified for most organizations as compliance risks change, state responsibilities expand, capital markets react and Campaign 2026 unfolds.
And in most households, concern about the affordability of medical care will elevate as federal and state funding cuts force higher out of pocket costs on consumers and demand for lower prices.
The summer will be busy for everyone in healthcare.
PS: Changes in the housing market are significant for healthcare: 36% of the CPI is based on shelter vs. 8% for medical services & products, 14% for food and 6% for energy/transportation. While the overall CPI increased 2.3% in the last 12 months, medical services prices increased 3.1%. contributing to heightened price sensitivity and delayed payments.
It has not escaped lawmaker attention: revenue cycle management business practices (debt collection) are being scrutinized in hospitals and community benefit declarations by not-for-profit hospitals re-evaluated. The economics of healthcare are not immune to broader market trends nor is spending for healthcare in households protected from day-to-day fluctuations in prices for other goods and services.
The U.S. Anxiety Pandemic
The U.S. bombing of Iran’s nuclear capability is unsettling: whether MAGA or not, hawk or dove, young or old, conservative or liberal, rich or poor—it matters.
Stability at home and abroad is utopian to some but desired by all. Pandemics, mass violence, natural disasters and even election results contribute to instability and lend to insecurity. Operation Midnight Hammer might contribute to the nation’s anxiety—time will tell.
The immediate aftermath of the bunker-bombings in Iran will involve two orchestrated campaigns by government officials:
- The Campaign to Contain Middle East Tension: military, diplomatic and economic levers will be put to the test to limit escalation of the bombing and limit its consequence to the region.
- The Campaign to Win Public Support: issues of consequence like military intervention ultimately depend on public opinion that support laws, funding and subsequent actions taken in response. History teaches and political leaders understand that ‘winning the hearts and minds’ of the public is necessary to success. Predictably, justification for Operation Midnight Hammer will be messaged loudly by supporters and challenged by critics.
For the moment, the news cycle will shift to foreign policy and away from tariffs, inflation, household prices and the “Big Beautiful Budget Bill” which the Senate Republicans hope to bring to the floor this week. News media will speculate about the after-effects of the Israeli-Iran bombing and what role the U.S. plays in an increasingly complicated geopolitical landscape marked by marked by armed conflicts Gaza, Ukraine, Myanmar, Yemen and 26 and other countries.
The attention these get in traditional media and social media channels will exacerbate public anxiety that’s already high: 19% U.S. adults and 40% of the country’s adolescents suffer from anxiety disorder: “a persistent, excessive fear or worry that interferes with daily life and functioning”. But, per the National Institute of Mental Health, fewer than a third suffering from severe anxiety receive professional treatment.
In the public health community, much is known about anxiety: it’s more prevalent among women than men, in minority populations, lower income populations and in the Southeast. It’s significant across all age groups, and at an alarming level among young working-class adults facing unique issues like affordability and job insecurity. And it is stigmatized in certain communities (i.e. certain fundamentalist religious sects, certain ethnic communities) lending to silent suffering and unattended consequences.
My take:
Operation Midnight Hammer came at a time of widespread public anxiety about the economy, tariffs, inflation, costs of living and political division. I will let pundits debate the advisability and timing of the bunker-bombing but I know one thing for sure: mental health issues—including anxiety, mood and substance abuse disorders– deserve more support from policymakers and more attention by the healthcare community.
- The former requires local, state and federal lawmakers to revisit and enforce mental health parity laws already on the books but rarely enforced.
- The latter requires the healthcare community to elevate behavioral health to a national priority alongside obesity, heart disease, cancer and aging to secure the public’s health and avoid unintended consequences of neglect.
Regrettably, the issue is not new. Employers, school systems, religious organizations and local public health agencies have been mental health default safety values to date; extreme have been temporarily shuffled to in hospital emergency rooms most ill-equipped to manage them. But systematic, community-wide, evidence-based help for those in need of mental health remains beyond their reach.
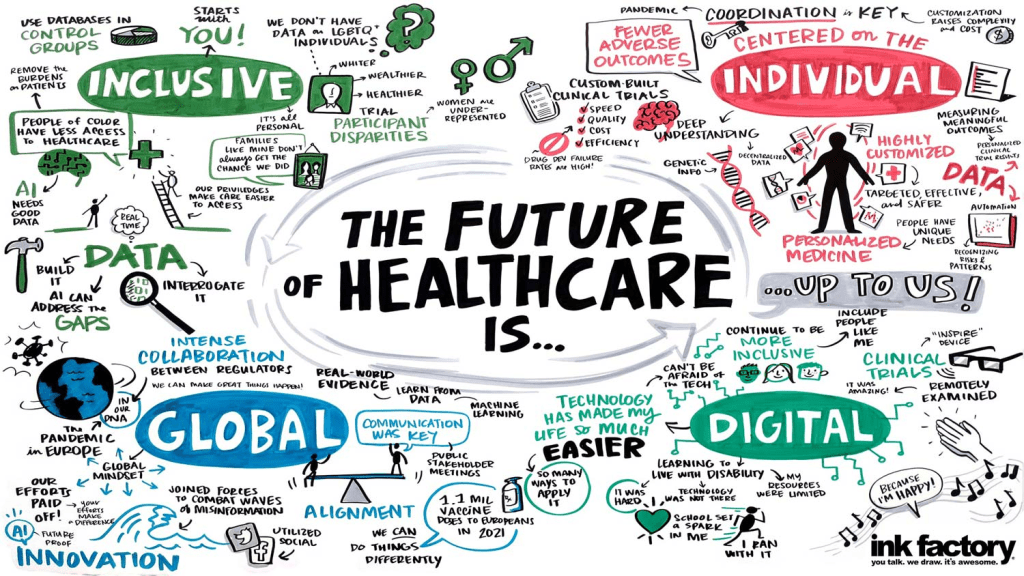
The Trump administration’s healthcare leaders under HHS’ Kennedy and CMS’ Oz espouse the U.S. healthcare system should prioritize chronic disease and preventive health. They believe its proficiency in specialty care is, in part, the result of lucrative incentives that reward providers and their financial backers handsomely in these areas.
In the President’s February 13 Executive Order establishing the Make America Healthy Again Commission, its goal was laid out:
“To fully address the growing health crisis in America, we must re-direct our national focus, in the public and private sectors, toward understanding and drastically lowering chronic disease rates and ending childhood chronic disease. This includes fresh thinking on nutrition, physical activity, healthy lifestyles, over-reliance on medication and treatments, the effects of new technological habits, environmental impacts, and food and drug quality and safety… We must ensure our healthcare system promotes health rather than just managing disease.”
Nothing could be more timely and necessary to the Commission’s work than addressing mass anxiety and mental health as a national priority. And nothing is more urgently needed in communities than mainstreaming anxiety and mental health into the systems of health that accept full risk for whole person health.
PS: Before Operation Midnight Hammer over the weekend, I had prepared today’s report focused on two government reports about the long-term solvency of the Medicaid and Medicare programs. Given the gravity of events in Israel and Iran and other hot spots, and after discussions with my family and friends this weekend, it became clear public anxiety is high.
I am concerned about the future and worry about the health system’s response. It’s composed of good people doing worthwhile work who are worried about the future. I recently spoke to a group on the theme (link below): ‘the future for healthcare is not a repeat of its past.’ That lends to anxiety unless accompanied by a vision for a better future. That’s what all hope for those in Iran, Gaza, Israel and beyond, and for all who serve in our industry.
From Budget Battles to Consumer Backlash: Paul Keckley on the Future of U.S. Health Care
The U.S. health care industry is approaching a critical inflection point, according to veteran health care strategist Paul Keckley. In a candid and thought-provoking keynote at the 2025 Healthcare Marketing & Physician Strategies Summit (HMPS) in Orlando, Keckley outlined the challenges and potential opportunities health care leaders must navigate in an era of unprecedented economic uncertainty, regulatory disruption, and consumer discontent.
Drawing on decades of policy experience and his signature candid style, Keckley delivered a sobering yet actionable assessment of where the industry stands and what lies ahead.
Paul Keckley, PhD, health care research and policy expert and managing editor of The Keckley Report
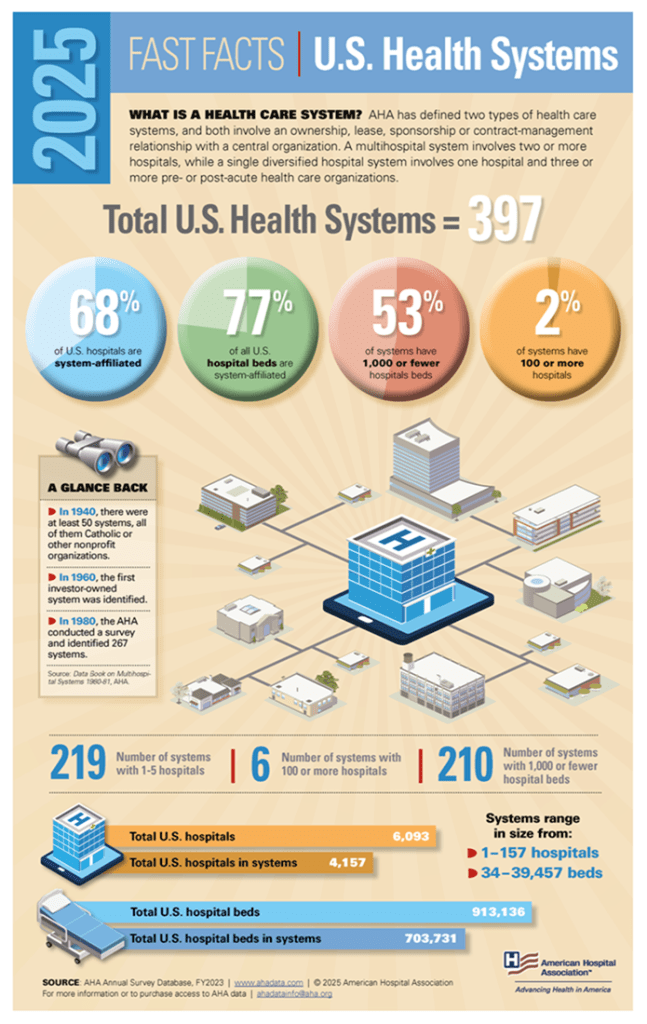
Health care now accounts for a staggering 28 percent of the federal budget, with Medicaid expenditures alone ranging from the low 20s to 34 percent of individual state budgets. Despite its fiscal significance, Keckley points out that health care remains “not really a system, but a collection of independent sectors that cohabit the economy.”
In the article that follows, Keckley warns of a reckoning for those who remain entrenched in legacy assumptions. On the flip side, he notes, “The future is going to be built by those who understand the consumer, embrace transparency, and adapt to the realities of a post-institutional world.”
A Fractured System in a Fractured Economy
Fragmentation complicates any effort to meaningfully address rising costs or care quality. It also heightens the stakes in a political climate marked by what Keckley termed “MAGA, DOGE, and MAHA” factions, shorthand for various ideological forces shaping health care policy under the Trump 2.0 administration.
Meanwhile, macroeconomic conditions are only adding to the strain. At the time of Keckley’s address, the S&P 500 was down 8 percent, the Dow down 10 percent, and inflationary pressures were squeezing both provider margins and household budgets.
“Economic uncertainty is not just about Wall Street,” Keckley warns. “It’s about kitchen-table economics — how households decide between paying for care or paying the cable bill.”
Traditional Forecasting Is Failing
One of Keckley’s key messages was that conventional methods of strategic planning in health care, based on lagging indicators like utilization rates and demographics, are no longer sufficient. Instead, leaders must increasingly look to external forces such as capital markets, regulatory volatility, and consumer behavior.
“Think outside-in,” he urges. “Forces outside health care are shaping its future more than forces within.”
He encourages health systems to go beyond isolated market studies and adopt holistic scenario planning that considers clinical innovation, workforce shifts, AI and tech disruption, and capital availability as interconnected variables.
Affordability and Accountability: The Hospital Reckoning
Keckley pulls no punches in addressing the mounting criticism of hospitals on Capitol Hill, particularly not-for-profit health systems. Public perception is faltering, with hospital pricing increasing faster than other categories in health care and only a third of providers in full compliance with price transparency rules.
“Economic uncertainty is not just about Wall Street. It’s about kitchen-table economics — how households decide between paying for care or paying the cable bill.”
“We have to get honest about trust, transparency, and affordability,” he says. “I’ve been in 11 system strategy sessions this year. Only one even mentioned affordability on their website, and none defined it.”
Keckley also predicts that popular regulatory targets like site-neutral payments, the 340B program, and nonprofit tax exemptions will face intensified scrutiny.
“Hospitals are no longer viewed as sacred institutions,” he says. “They’re being seen as part of the problem, especially by younger, more educated, and more skeptical Americans.”
The Consumer Awakens
Perhaps the most urgent shift Keckley outlines is the redefinition of the health care consumer. “We call them patients,” he says, “but they are consumers. And they are not happy.”
Keckley cites polling data showing that two out of three Americans believe the health care system needs to be rebuilt from the ground up. Roughly 40 percent of U.S. households have at least one unpaid medical bill, with many choosing intentionally not to pay. Among Gen Y and younger households, dissatisfaction is particularly acute.
“[Consumers] expect digital, personalized, seamless experiences — and they don’t understand why health care can’t deliver.”
These consumers aren’t just passive recipients of care; they’re voters, payers, and critics. With 14 percent of health care spending now coming directly from households, Keckley argues, health systems must engage consumers with the same sophistication that retail and tech companies use.
“They expect digital, personalized, seamless experiences — and they don’t understand why health care can’t deliver.”
Tech Disruption Is Real
Keckley underscores the transformative potential of AI and emerging clinical technologies, noting that in the next five years, more than 60 GLP-1-like therapeutic innovations could come to market. But the deeper disruption, he warns, is likely to come from outside the traditional industry.
Citing his own son’s work at Microsoft, Keckley envisions a future where a consumer’s smartphone, not a provider or insurer, is the true hub of health information. “Health care data will be consumer-controlled. That’s where this is headed.”
The takeaway for providers: Embrace data interoperability and consumer-centric technology now, or risk irrelevance. “The Amazons and Apples of the world are not waiting for CMS to set the rules,” Keckley says.
Capital, Consolidation, and Private Equity
Capital constraints and the shifting role of private equity also featured prominently in Keckley’s remarks. With declining non-operating revenue and shrinking federal dollars, some health systems increasingly rely on investor-backed funding.
But this comes with reputational and operational risks. While PE investments have been beneficial to shareholders, Keckley says, they’ve also produced “some pretty dire results for consumers” — particularly in post-acute care and physician practice consolidation.
“Policymakers are watching,” he says. “Expect legislation that will limit or redefine what private equity can do in health care.”
Politics and Optics: Navigating the Policy Minefield
In the regulatory arena, Keckley emphasizes that perception often matters more than substance. “Optics matter often more than the policy itself,” he says.
He cautions health leaders not to expect sweeping policy reform but to brace for “de jure chaos” as the current administration focuses on symbolic populist moves — cutting executive compensation, promoting price transparency, and attacking nonprofit tax exemptions.
With the 2026 midterm elections looming large, Keckley predicts a wave of executive orders and rhetorical grandstanding. But substantive policy change will be incremental and unpredictable.
“Don’t wait for a rescue from Washington. The future is going to be built by those who understand the consumer, embrace transparency, and adapt to the realities of a post-institutional world.”
The Workforce Crisis That Wasn’t Solved
Keckley also addresses the persistent shortage of health care workers and the failure of Title V of the ACA, which had promised to modernize the workforce through new team-based models. “Our guilds didn’t want it,” Keckley notes, bluntly. “So nothing happened.”
He argues that states, not the federal government, will drive the next chapter of workforce reform, expanding the scope of practice for pharmacists, nurse practitioners, and even lay caregivers, particularly in behavioral health and primary care.
What Should Leaders Do Now?
Keckley closed his keynote with a challenge for marketers and strategists: Get serious about defining affordability, understand capital markets, and stop defaulting to legacy assumptions.
“Don’t wait for a rescue from Washington,” he says. “The future is going to be built by those who understand the consumer, embrace transparency, and adapt to the realities of a post-institutional world.”
He encouraged leaders to monitor shifting federal org charts, track state-level policy moves, and scenario-plan for a future where trust, access, and consumer empowerment define success.
Conclusion: A Health Care Reckoning in the Making
Keckley’s keynote was more than a policy forecast; it was a wake-up call. In a landscape shaped by economic headwinds, political volatility, and consumer rebellion, health care leaders can no longer afford to stay in their lane. They must engage, adapt, and transform, or risk becoming casualties of a system under siege.
“Health care is not just one of 11 big industries,” Keckley says. “It’s the one that touches everyone. And right now, no one is giving us a standing ovation.”
Republicans Are Turning on Medicare Advantage
UnitedHealth Group and the other insurance giants running the Medicare Advantage (MA) program might want to start paying attention to something they haven’t worried much about before: growing skepticism from Republicans.
Until recently, efforts to reform MA — a privatized version of Medicare now covering more than half of all beneficiaries — came mostly from Democrats and independent policy experts.
No longer. The latest skepticism is not coming from a liberal think tank or a progressive PAC. It’s coming from two Republican doctors who have spent decades treating patients and sit on powerful House committees overseeing health care. It’s coming from a former Republican congressman who was an author of the law that established Medicare Advantage two decades ago. And it’s coming from right-leaning organizations and policy experts who are now demanding major changes to MA. Their position marks a dramatic and important shift that could lead to meaningful reforms being enacted in a Congress controlled by Republicans.
An Architect of MA Speaks Out
In an op-ed published by The Hill Sunday, former Republican Rep. Jim Greenwood of Pennsylvania — who helped write the Medicare Modernization Act that created Medicare Advantage — said plainly: “The program no longer lives up to [its] promise.”
Greenwood wrote that he had once believed private competition would drive innovation and efficiency. But today, he says, MA has been overtaken by “a handful of massive insurers who are gaming the rules for profit.” Overpayments, cherry-picking, and risk-score manipulation, he said, are now “endemic.”
“It pains me to say this, but the system we helped create is being abused. And it’s not just hurting taxpayers. It’s hurting patients.”
“Seniors… are too often finding out — at the worst possible time — that their plan won’t cover what they need.”
While Greenwood still believes there is a place for private-sector involvement in Medicare, he now calls for rigorous oversight, transparency, and enforcement. He also warns against insurers’ predictable scare tactics whenever reform is on the table.
“I never imagined that Medicare Advantage would become a vehicle for such waste and abuse,” Greenwood concluded. “It’s time to fix it.”
Republican Congressional Docs Say Medicare Advantage Is Broken
Another recent op-ed, written for The Washington Times by two conservative Republicans, Rep. Greg Murphy of North Carolina and Rep. John Joyce of Pennsylvania – both physicians and co-chairs of the GOP Doctors’ Caucus — draws the same conclusion: Medicare Advantage veered too far off course, and it’s time to rein it in. They wrote:
“Profit-driven insurance companies have destroyed [Medicare Advantage’s] model.”
“These plans must stop seeing rewards for delaying or altogether denying care to beneficiaries that need it.”
They called out insurers for “upcoding” — the practice of exaggerating how sick patients are to collect more taxpayer dollars — and for using prior authorization as a weapon to delay or deny necessary care to America’s seniors.
These aren’t unsubstantiated complaints. Recent media investigations found that MA plans regularly reject claims that would be approved under traditional Medicare. The Department of Health and Human Services Inspector General has raised alarms, and the U.S. Justice Department has set its sights on UnitedHealth Group’s Medicare business in particular.
And according to the Medicare Payment Advisory Commission (MedPAC), MA is now costing taxpayers 22% more per beneficiary than traditional Medicare — a difference that translates to $83 billion in overpayments to private health insurers last year alone.
Now, Republicans like Murphy and Joyce are saying the quiet part out loud: MA is making insurance company executives and investors rich at the expense of seniors, people with disabilities and taxpayers.
Conservative Advocacy Voices Are Speaking Up, Too
Phil Kerpen, president of the conservative group American Commitment, warned in an op-ed for the Daily Times that Medicare Advantage — which he said was once a “highly innovative and successful” option — is now “becoming increasingly costly and unstable.”
Kerpen pointed to the Department of Justice’s criminal investigation into UnitedHealth as a wake-up call and criticized the monopolistic consolidation of insurers buying up doctors, hospitals, and pharmacies. He called out opaque billing practices, delays in care, and an “unfair burden on taxpayers.”
“If ever there were a government program in need of DOGE-like accountability, competition, and transparency, Medicare Advantage is it.”
He called for reforms many — including myself — have long demanded: stronger disclosure rules, better tools for plan comparison, and serious action on prior authorization abuse. To save the program, he said, President Trump and Congress must be willing to “take on the big insurers and reform it. And quickly.”
Cracks in the Wall of Insurance Influence
There was even a last-minute push, led by Senate HELP Committee Chair Bill Cassidy (R-Louisiana), a doctor, to include MA reforms in Trump’s “One Big Beautiful Bill.” While that effort reportedly failed, Republican critics of the program are vowing to work on a bipartisan basis to enact changes the insurance lobby has fought for years. Upgrade to paid
I spent years in the executive suites of Cigna and Humana — historically big players in Medicare Advantage — and I can tell you this: Republican lawmakers and conservative thought leaders demanding reforms to MA is no small thing. Private insurance corporations have long counted on bipartisan cover to operate with minimal oversight. If they start losing support from Republicans and conservative media, that protective wall begins to crack.
For years, industry lobbyists succeeded in casting Medicare Advantage as politically untouchable — “too complicated,” “too entrenched,” or “too popular to fix.” But as more members of Congress hear from their constituents about denied care, inadequate provider networks, rising out-of-pocket costs, and profiteering by insurance corporations, that illusion is dissipating.
With GOP leaders like Murphy, Joyce, Kerpen — and now Greenwood — stepping forward, it’s clear the tide is turning. Medicare Advantage reform is no longer a partisan issue — it’s an American issue. And for the sake of patients, taxpayers, and the solvency of the Medicare Trust Fund, it’s time Washington acts like it.
The GOP Still Lacks a Clear Plan for Health Care

he House GOP’s emerging megabill includes significant changes to health care, some of which are long overdue, such as tighter restrictions on the provider taxes which states use to shift Medicaid costs onto the federal budget. But the legislation’s effect on the number of uninsured individuals is likely to get the most attention. Projections showing there will be a sizeable increase are causing internal divisions and creating political risks.
The basic problem for the party remains as it was in 2017 during the failed attempt to repeal and replace the Affordable Care Act (ACA), which is that there is no agreement among its leaders on an overall direction to guide the changes they advance. It is probably too late to develop such a plan for this year’s legislative debate, but it remains necessary if GOP officeholders ever want to have more lasting influence on the workings of the overall system.
The Democratic party has long rallied around an organizing principle for the changes it seeks. The ultimate goal is a universal public utility model with everyone covered. There are differences among leading party members over the specific routes to this destination but not on the direction of travel. The party wants to strongly regulate the entire sector, including insurance and the providers of services, and most especially with respect to the prices they charge. The suppliers would be entirely dependent on government-set rates for their revenue. In return, they would get paid just enough to stay open and face less pressure to compete based on efficiency. A single-payer plan is consistent with the party’s goals, but so too would be an extension of Medicare’s fees to the commercial market.
Republicans have nothing similar to rally around. In the megabill, the goal is to slow the growth of public subsidization of insurance enrollment and promote work, with the savings devoted to a lower level of taxation. It is a fiscal exercise and not a plan to reform American health care.
It also leaves the party exposed to criticism. If the federal government pulls back support without bringing down total costs, then someone else has to pay for the care provided to patients, or else some care might have to be curtailed. Predictably, as analyses emerge showing the GOP bill will produce these effects, the political blowback has been building.
The alternative to a public utility model is a system that is disciplined by market incentives instead of regulations but which still embraces population-wide insurance enrollment. The megabill includes important improvements to Health Savings Accounts (HSAs) that point in this direction, but they are too marginal to substantially alter incentives in the entire sector.
Republicans should consider what can be done to bring down costs across-the-board so that all purchasers get financial relief. There are several targets available.
- Stronger Price Competition.
- The first Trump administration pushed for transparent pricing in health care, which was an important step. However, for the market to work, consumers need to be far more engaged and incentivized to opt for lower-priced options. To promote stronger competition, the federal government should require providers of high-volume services to disclose their prices based on standardized bundles, and then also require insurers to let consumers migrate to lower-priced suppliers and keep the savings.
- Competitive Bidding.
- In Medicare and Medicaid, there is too much reliance on regulated rates and not enough on competitive bidding. Both programs should use bidding to establish the rates that the government will pay for services whenever that is a possibility. For instance, Medicare could require competitive bidding for high-volume services such as laboratory testing and imaging, and then use the submitted prices to build a preferred network of providers. Further, competitive bidding should be used to set rates for Medicare Advantage plans and, in time, to establish a level playing field of competition with the traditional program. Some of the savings from these reforms could be used to provide catastrophic insurance protection as a feature of the entire program, and not just in MA.
- More Enrollment in Job-Based Insurance.
- Republicans should drop their ambivalence toward insurance enrollment. The balance of the empirical evidence backs the importance of staying in coverage to a person’s health status. Moreover, the public does not want large numbers of uninsured again. To lessen the burden on Medicaid and to promote work, Republicans should look to help low-wage workers secure employer-sponsored insurance (ESI). Redirecting a portion of the tax subsidy for this insurance from high-wage to low-wage workers could induce some individuals out of Medicaid and Affordable Care Act plans and into ESI.
The GOP is right that surging costs for Medicare and Medicaid are a fiscal threat, but if their solutions push more financial risk onto individual consumers and patients, the backlash might hasten changes that Democrats have long sought.
Medicare Advantage Is Ripe for an Overhaul
As the Senate eyes alternative or additional cost-saving provisions to those included in the House-passed reconciliation bill, some Republicans are considering reforms to Medicare. That is a promising development because overhauling Medicare Advantage could lower federal costs in ways that even many Democrats have advocated (although it is certain the overall bill will receive no Democratic support due to myriad other provisions).
Medicare Advantage, or MA, is Medicare’s private insurance option.
Beneficiaries can get their coverage through these plans in lieu of the traditional, government-managed program. Medicare pays MA sponsors a per-person monthly fee, which they use in turn to pay providers for the services their enrollees need. Enrollment in MA surged after Congress amended the payment formula in 2003. According to the 2024 Medicare trustees report, in the last decade alone, MA enrollment increased from 16 million people in 2014, or 30 percent of total enrollment, to 34 million people in 2024, or one out of every two program beneficiaries.
MA is growing because the plans usually offer more generous coverage than the traditional program without charging substantially higher premiums. In fact, many MA enrollees get free prescription drug coverage and much lower cost-sharing for hospital and physician services. They also sometimes get limited dental and vision care protection. MA enrollees usually do not pay for Medigap insurance, which can be expensive.
Critics argue MA plans can offer added benefits only because they are overpaid – a contention credible research confirms, including as conducted by the Medicare Payment Advisory Commission (MedPAC). At the same time, other data shows MA plans are often more efficient at delivering services than the traditional program because the plans scrutinize claims more carefully. High MA enrollment is also associated with positive spillover effects in the traditional program.
MA reforms should incentivize efficiency and high-quality care without needlessly overpaying the plans. The Senate should pull together a reform plan that gradually restructures the MA market so that it operates more efficiently and with lower costs for taxpayers. The following general principles should guide what is developed.
- Competitive Bidding.
- MA plans submit bids under the current formula, but Medicare’s payment is a combination of those bids and benchmarks that are set administratively. The Senate should amend the formula to rely strictly on bidding, with a transition to prevent abrupt changes in what is offered to enrollees. The payment could be based on the average bid weighted by enrollment. The new system could be phased in over five years by gradually increasing its influence on the formula (20 percent in year one, going up to 100 percent in year five, for instance).
- Standardized Benefits.
- Competitive bidding should be combined with standardization of the coverage MA plans are offering. Without such rules, it is difficult for individual beneficiaries to compare their options on an apples-to-apples basis. The Senate should require CMS to develop a standard MA offering that is comparable in value to the traditional benefit (it may be necessary to add catastrophic protection to the traditional program to ensure the competition is fair). MA plans would then submit their bids based on this standardized offering, and all Medicare beneficiaries would have the option of opting for such coverage. Further, the Senate should direct CMS to develop a small number of standardized supplemental benefits that could be purchased by beneficiaries with additional premium payments. These offerings could focus on the most popular add-ons in the MA market.
- Risk Adjustment.
- There are many criticisms of the current system of providing payment adjustments to MA plans based on the varied health risks of their enrollees. The current system has several flaws that might be addressed, but the basic problem is too much reliance on the data submitted by the plans which can lead directly to higher revenue. That design of course invites abuse. The Senate should put into law a requirement that CMA is to determine a final annual risk score for the plans based on submitted information, and any needed refinements by the government to ensure the fairest possible comparisons across plans.
- ACOs as MA Plans.
- The Medicare program would benefit from robust provider-driven MA plans that can effectively compete with the insurer-led MA offerings now dominating the market. CMS should work with interested Accountable Care Organizations (ACOs) on building out functions they would need to become viable alternatives in the MA insurance market.
The Congressional Budget Office (CBO) estimates the House bill will increase deficits by $3.0 trillion over ten years when net interest is in the calculation. Medicare reforms could help the Senate produce a more fiscally responsible bill. If an MA bidding system led to a reduction in payments comparable to a 10 percent cut (which is realistic based on MedPAC’s research), the savings over a decade would be close to $500 billion.
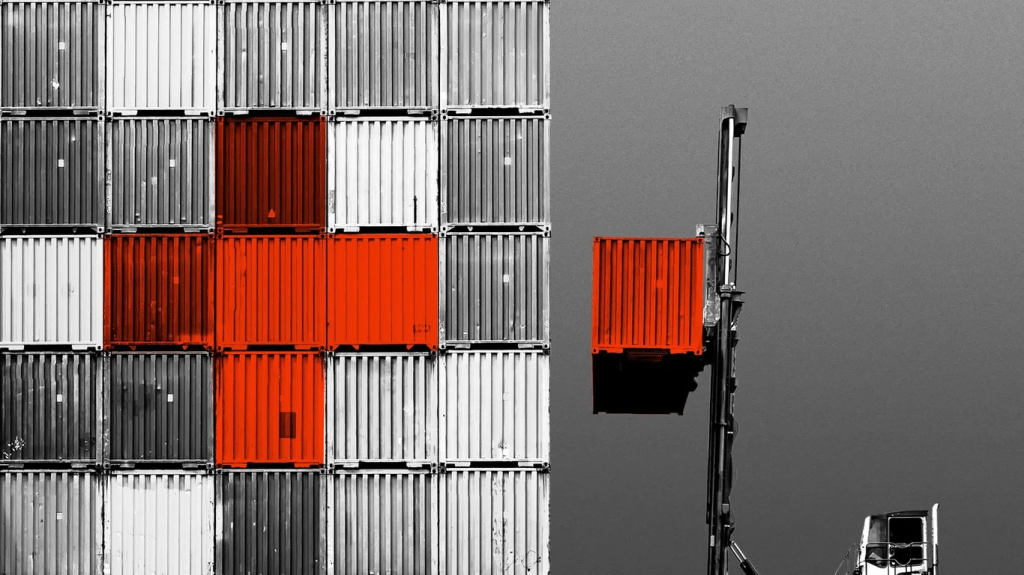
Hospital purchasing still buffeted by trade winds
https://www.axios.com/2025/06/18/hospital-purchasing-tariffs-trump-ppe

Tariffs and supply chain uncertainty are playing havoc with hospitals’ purchasing plans, especially for lower-margin products like gloves, gowns and syringes.
Why it matters:
The uncertainty is in some cases delaying spending decisions, including capital improvements, as health system administrators wait to see the effect of increased duties and whether manufacturers win exemptions from the Trump administration.
What they’re saying:
“Hospitals are definitely feeling a pinch,” Mark Hendrickson, director of Premier’s supply chain policy, told Axios. “We’ve never seen tariffs for this long a period of time for this broad a portfolio of products in basically all of our lifetimes.”
- “It’s really an uncertain enough environment that we’re cautioning members from panic buying and buying ahead,” he added. “We don’t want to drive artificial shortages of products that could be avoided.”
The big picture:
The health care supply chain is already hard enough to navigate, with certain sterile injectable drugs and other essentials regularly going into shortage.
- But President Trump’s existing and threatened tariffs are scrambling the calculus for health systems and the group purchasing organizations they contract with, as they seek a steady supply of what they need and identify possible new sources.
- “Everyone in the supply chain, from hospitals to suppliers to manufacturers, is grappling with how to plan thoughtfully and proceed in a way that doesn’t either under- or over-correct for the potential impacts of these tariffs,” Akin Demehin, the American Hospital Association’s vice president of quality and patient safety policy, told Axios.
Between the lines:
So far, there haven’t been clear price hikes or shortages.
- But certain types of products are being watched more closely, starting with low-cost, high-volume items often imported from China such as PPE and disposable medical devices.
- “Are there going to be instances where those low margin products are just not worth manufacturing anymore?,” Hendrickson said.
U.S. manufacturing of protective gear picked up during the pandemic, to alleviate foreign supply chain disruptions. But some of those sources dried up with the end of mask mandates and other public health measures, when hospitals went back to buying from overseas.
- The hospital association is particularly concerned about critical minerals and derivatives used in medical imaging, radioactive drugs and other applications, which could be subject to sectoral levies imposed in the interests of national security.
- Last month, the AHA sent a letter to the Trump administration calling for medical exemptions.
The bottom line:
“We haven’t seen the bottom fall out,” Hendrickson said. “I’m hoping we don’t.”
Tariffs drive health plan premium hikes
https://www.axios.com/2025/06/18/tariffs-health-insurance-premium-hikes
Health insurers are starting to notify states that tariffs will drive up the premiums they plan to charge individual and small group market enrollees next year.
Why it matters:
The Trump administration’s trade policy is adding another layer of uncertainty for health costs as Congress considers Medicaid cuts and is expected to sunset enhanced subsidies for Affordable Care Act coverage.
- “There are sort of a perfect storm of factors that are driving prices up,” said Sabrina Corlette, research professor at Georgetown’s Center on Health Insurance Reforms.
The big picture:
Health insurers calculate monthly premiums in advance of each year based on the expected price of goods and services and projected demand for them.
- Tariffs announced by President Trump are expected to drive up the cost of prescription drugs, medical devices and other medical products and services. Some of that difference ultimately would be passed down to enrollees.
Where it stands:
A handful of health insurers administering individual and small group plans have already explicitly told state regulators that tariffs are forcing plans to raise enrollee premiums more than they otherwise would next year, KFF policy analyst Matt McGough wrote in an analysis published Monday.
- Independent Health Benefits Corporation told New York regulators in a filing last month that it plans to raise premiums for its individual market enrollees 38.4% next year.
- About 3% of that is directly due to tariffs, based on projections of how much they’ll increase drug prices and the use of imported drugs, Frank Sava, a spokesperson for Independent Health, told Axios.
- Similarly, UnitedHealthcare of Oregon said in a filing that nearly 3% of its planned 19.8% premium increase for small group enrollees next year is due to uncertainty around tariffs, particularly on how they’ll affect pharmaceutical prices.
Insurers “don’t have any historical precedent or data to project what this is going to mean for their business and health costs,” McGough said to Axios. “I think it really makes sense that they’re trying to hedge their bets.”
- Insurers can’t change their premiums throughout the year. But if health plans do overshoot their premium estimates in rate filings, they have to pay enrollees back the difference in rebates.
- While there may be a competitive advantage to keeping premiums lower, there isn’t really a way for insurers to make up for extra unplanned costs after the fact.
Yes, but:
Some insurers indicated that while they’re keeping a close eye on tariff-related impacts, they aren’t baking them into their premium rates yet.
- “There is uncertainty around inflation and the economy due to possible tariffs however we did [not] put anything for this in this filing,” Kaiser Foundation Health Plan of the Northwest’s report to Oregon reads.
- State regulators can also push back on insurers’ premium calculations before they’re finalized, McGough noted.
What we’re watching:
While some states have earlier deadlines, insurers have to submit their 2026 ACA marketplace plan rates to the federal regulators by July 16, and proposed rates will be posted by August 1.
- That’s when we’ll get a better picture of how seriously tariffs are concerning health insurers.

