https://www.healthcaredive.com/news/medicaid-expansion-rural-hospitals-health-affairs/579005/

Dive Brief:
- Struggling rural hospitals are faring better financially in states that expanded Medicaid under the Affordable Care Act, according to a new Health Affairs study examining 1,004 rural hospitals’ CMS cost reports submitted from 2011 to 2017.
- Among rural, nonprofit critical access hospitals in states that expanded Medicaid, the median overall margin increased from 1.8% to 3.7%, while it dropped from 3.5% to 2.8% in states that did not expand the program.
- Tax-exempt status played another key role in determining rural hospitals’ financial viability. During the study period, the median overall profit margin at nonprofit critical access hospitals rose from 2.5% to 3.2%, while it dropped among for-profit operators from 3.2% to 0.4%.
Dive Insight:
The unprecedented financial distress mega health systems are under amid the ongoing pandemic is all too familiar to rural hospitals.
These systems are often smaller, employing fewer specialists and less medical technology, thus limiting the variety of services they can provide and profit on. They remain the closest point of care for millions of Americans, yet face rising closures.
The good news is that most rural hospitals are nonprofit, the designation that fared best in Health Affairs’ six-year study. More than 80% of the 1,004 private, rural hospitals analyzed in the study were nonprofit, while 17% were for-profit.
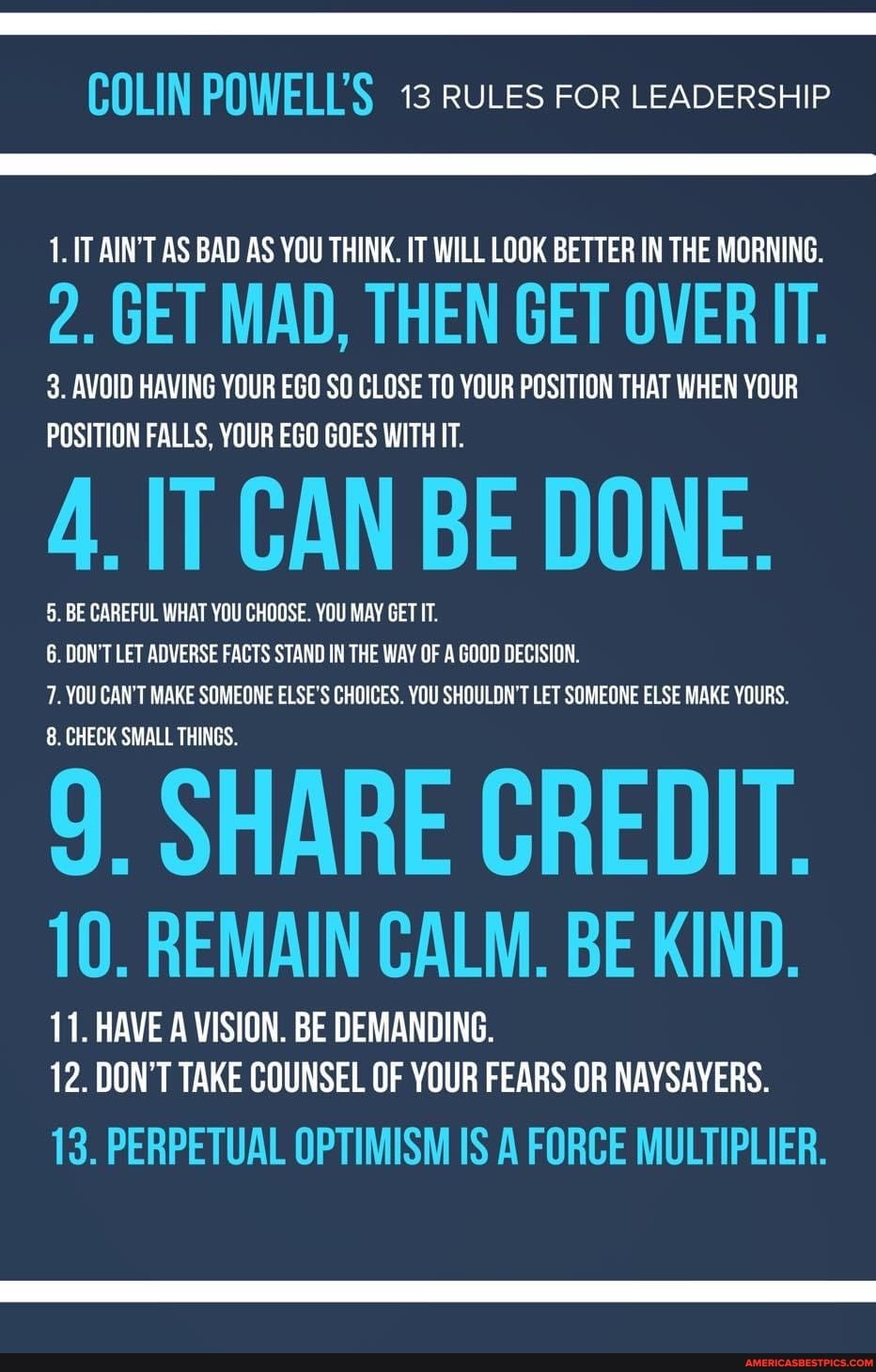
But researchers found Medicaid expansion played a key role in rural hospitals’ financial viability during the study period, with closures occurring more often in the South than in other regions.
Thirty-seven states have expanded Medicaid under the ACA, but 14 have not, and a majority of them are concentrated in the southern U.S., according to data from the Kaiser Family Foundation.
One of those states is Oklahoma, which on Monday withdrew its planned July 1 Medicaid expansion, citing a lack of funding.
Another factor researchers found positively associated with overall margins and financial viability was charge markups, or the charged amount for a service relative to the Medicare allowable cost. Hospitals with low-charge markups had median overall margins of 1.8%, while those with high-charge markups had margins at 3.5%.
The same is true for occupancy rates. In 2017, rural hospitals with low occupancy rates had median overall profit margins of 0.1% Those with high occupancy rates had margins of 4.7%.
That presents a unique challenge for rural hospitals. Reimbursements from public and private payers do not compensate for fixed costs associated with providing standby capacity, which is essential in rural communities, where few hospitals serve large geographic areas.
Since 1997, CMS has been granting rural hospitals — particularly those with 25 or fewer acute care inpatient beds and located more than 35 miles from another hospital — critical access status, reimbursing them at cost for treating Medicare patients.
In the Health Affairs study, critical access hospitals accounted for 21% of the rural hospital bed capacity, with the remaining 79% of bed capacity provided by noncritical access hospitals.