Humankind has never had a more urgent task than creating broad immunity for coronavirus.
One of the questions I get asked the most these days is when the world will be able to go back to the way things were in December before the coronavirus pandemic. My answer is always the same: when we have an almost perfect drug to treat COVID-19, or when almost every person on the planet has been vaccinated against coronavirus.
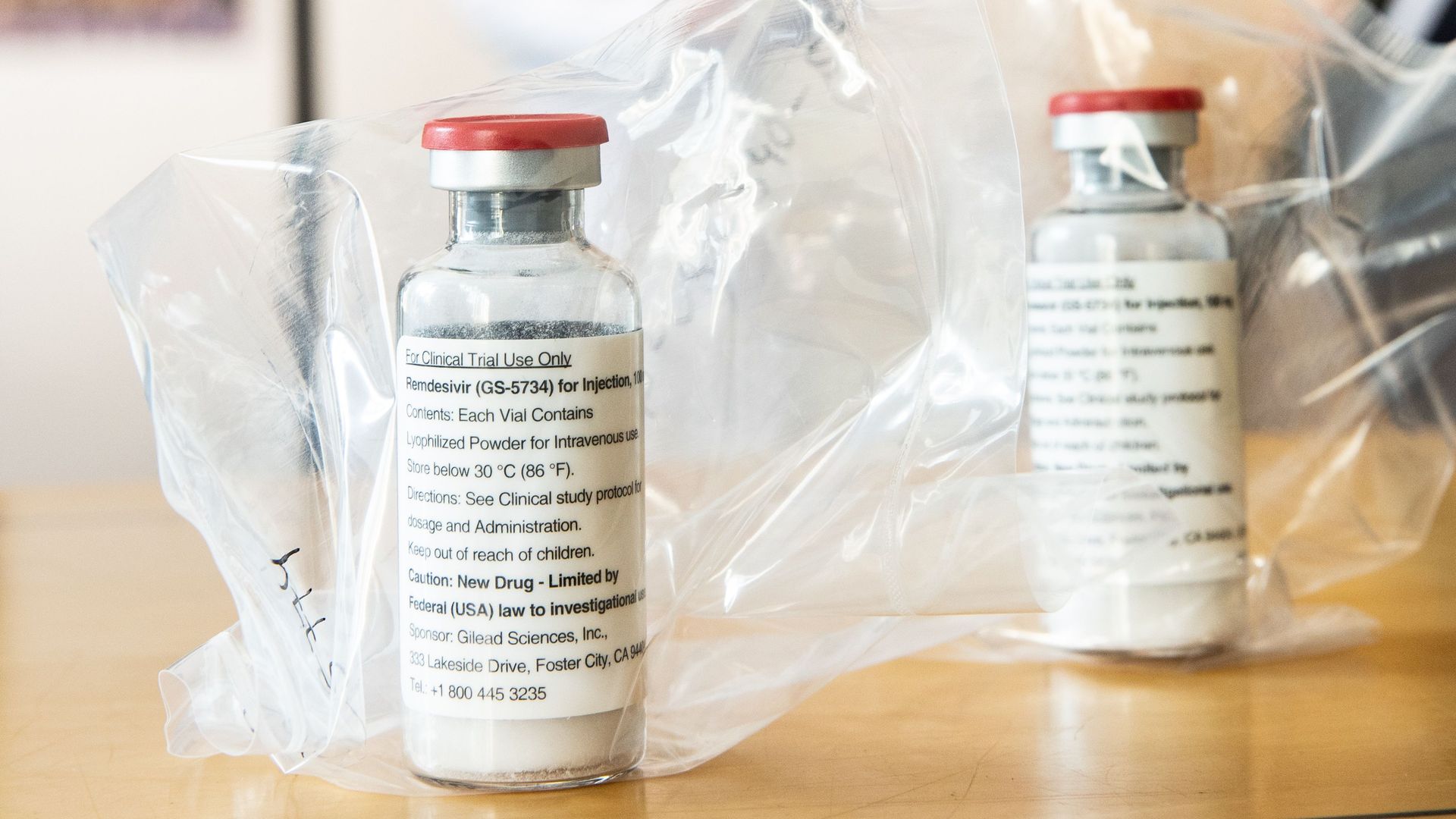
The former is unlikely to happen anytime soon. We’d need a miracle treatment that was at least 95 percent effective to stop the outbreak. Most of the drug candidates right now are nowhere near that powerful. They could save a lot of lives, but they aren’t enough to get us back to normal.
Which leaves us with a vaccine.
Humankind has never had a more urgent task than creating broad immunity for coronavirus. Realistically, if we’re going to return to normal, we need to develop a safe, effective vaccine. We need to make billions of doses, we need to get them out to every part of the world, and we need all of this happen as quickly as possible.
That sounds daunting, because it is. Our foundation is the biggest funder of vaccines in the world, and this effort dwarfs anything we’ve ever worked on before. It’s going to require a global cooperative effort like the world has never seen. But I know it’ll get done. There’s simply no alternative.
Here’s what you need to know about the race to create a COVID-19 vaccine.
The world is creating this vaccine on a historically fast timeline.
Dr. Anthony Fauci has said he thinks it’ll take around eighteen months to develop a coronavirus vaccine. I agree with him, though it could be as little as 9 months or as long as two years.
Although eighteen months might sound like a long time, this would be the fastest scientists have created a new vaccine. Development usually takes around five years. Once you pick a disease to target, you have to create the vaccine and test it on animals. Then you begin testing for safety and efficacy in humans.
Safety and efficacy are the two most important goals for every vaccine. Safety is exactly what it sounds like: is the vaccine safe to give to people? Some minor side effects (like a mild fever or injection site pain) can be acceptable, but you don’t want to inoculate people with something that makes them sick.
Efficacy measures how well the vaccine protects you from getting sick. Although you’d ideally want a vaccine to have 100 percent efficacy, many don’t. For example, this year’s flu vaccine is around 45 percent effective.
To test for safety and efficacy, every vaccine goes through three phases of trials:
- Phase one is the safety trial. A small group of healthy volunteers gets the vaccine candidate. You try out different dosages to create the strongest immune response at the lowest effective dose without serious side effects.
- Once you’ve settled on a formula, you move onto phase two, which tells you how well the vaccine works in the people who are intended to get it. This time, hundreds of people get the vaccine. This cohort should include people of different ages and health statuses.
- Then, in phase three, you give it to thousands of people. This is usually the longest phase, because it occurs in what’s called “natural disease conditions.” You introduce it to a large group of people who are likely already at the risk of infection by the target pathogen, and then wait and see if the vaccine reduces how many people get sick.
After the vaccine passes all three trial phases, you start building the factories to manufacture it, and it gets submitted to the WHO and various government agencies for approval.
This process works well for most vaccines, but the normal development timeline isn’t good enough right now. Every day we can cut from this process will make a huge difference to the world in terms of saving lives and reducing trillions of dollars in economic damage.
So, to speed up the process, vaccine developers are compressing the timeline. This graphic shows how:
In the traditional process, the steps are sequential to address key questions and unknowns. This can help mitigate financial risk, since creating a new vaccine is expensive. Many candidates fail, which is why companies wait to invest in the next step until they know the previous step was successful.
For COVID-19, financing development is not an issue. Governments and other organizations (including our foundation and an amazing alliance called the Coalition for Epidemic Preparedness Innovations) have made it clear they will support whatever it takes to find a vaccine. So, scientists are able to save time by doing several of the development steps at once. For example, the private sector, governments, and our foundation are going to start identifying facilities to manufacture different potential vaccines. If some of those facilities end up going unused, that’s okay. It’s a small price to pay for getting ahead on production.
Fortunately, compressing the trial timeline isn’t the only way to take a process that usually takes five years and get it done in 18 months. Another way we’re going to do that is by testing lots of different approaches at the same time.
There are dozens of candidates in the pipeline.
As of April 9, there are 115 different COVID-19 vaccine candidates in the development pipeline. I think that eight to ten of those look particularly promising. (Our foundation is going to keep an eye on all the others to see if we missed any that have some positive characteristics, though.)
The most promising candidates take a variety of approaches to protecting the body against COVID-19. To understand what exactly that means, it’s helpful to remember how the human immune system works.
When a disease pathogen gets into your system, your immune system responds by producing antibodies. These antibodies attach themselves to substances called antigens on the surface of the microbe, which sends a signal to your body to attack. Your immune system keeps a record of every microbe it has ever defeated, so that it can quickly recognize and destroy invaders before they make you ill.
Vaccines circumvent this whole process by teaching your body how to defeat a pathogen without ever getting sick. The two most common types—and the ones you’re probably most familiar with—are inactivated and live vaccines. Inactivated vaccines contain pathogens that have been killed. Live vaccines, on the other hand, are made of living pathogens that have been weakened (or “attenuated”). They’re highly effective but more prone to side effects than their inactivated counterparts.
Inactivated and live vaccines are what we consider “traditional” approaches. There are a number of COVID-19 vaccine candidates of both types, and for good reason: they’re well-established. We know how to test and manufacture them.
The downside is that they’re time-consuming to make. There’s a ton of material in each dose of a vaccine. Most of that material is biological, which means you have to grow it. That takes time, unfortunately.
That’s why I’m particularly excited by two new approaches that some of the candidates are taking: RNA and DNA vaccines. If one of these new approaches pans out, we’ll likely be able to get vaccines out to the whole world much faster. (For the sake of simplicity, I’m only going to explain RNA vaccines. DNA vaccines are similar, just with a different type of genetic material and method of administration.)
Our foundation—both through our own funding and through CEPI—has been supporting the development of an RNA vaccine platform for nearly a decade. We were planning to use it to make vaccines for diseases that affect the poor like malaria, but now it’s looking like one of the most promising options for COVID. The first candidate to start human trials was an RNA vaccine created by a company called Moderna.
Here’s how an RNA vaccine works: rather than injecting a pathogen’s antigen into your body, you instead give the body the genetic code needed to produce that antigen itself. When the antigens appear on the outside of your cells, your immune system attacks them—and learns how to defeat future intruders in the process. You essentially turn your body into its own vaccine manufacturing unit.
Because RNA vaccines let your body do most of the work, they don’t require much material. That makes them much faster to manufacture. There’s a catch, though: we don’t know for sure yet if RNA is a viable platform for vaccines. Since COVID would be the first RNA vaccine out of the gate, we have to prove both that the platform itself works and that it creates immunity. It’s a bit like building your computer system and your first piece of software at the same time.
Even if an RNA vaccine continues to show promise, we still must continue pursuing the other options. We don’t know yet what the COVID-19 vaccine will look like. Until we do, we have to go full steam ahead on as many approaches as possible.
It might not be a perfect vaccine yet—and that’s okay.
The smallpox vaccine is the only vaccine that’s wiped an entire disease off the face of the earth, but it’s also pretty brutal to receive. It left a scar on the arm of anyone who got it. One out of every three people had side effects bad enough to keep them home from school or work. A small—but not insignificant—number developed more serious reactions.
The smallpox vaccine was far from perfect, but it got the job done. The COVID-19 vaccine might be similar.
If we were designing the perfect vaccine, we’d want it to be completely safe and 100 percent effective. It should be a single dose that gives you lifelong protection, and it should be easy to store and transport. I hope the COVID-19 vaccine has all of those qualities, but given the timeline we’re on, it may not.
The two priorities, as I mentioned earlier, are safety and efficacy. Since we might not have time to do multi-year studies, we will have to conduct robust phase 1 safety trials and make sure we have good real-world evidence that the vaccine is completely safe to use.
We have a bit more wiggle room with efficacy. I suspect a vaccine that is at least 70 percent effective will be enough to stop the outbreak. A 60 percent effective vaccine is useable, but we might still see some localized outbreaks. Anything under 60 percent is unlikely to create enough herd immunity to stop the virus.
The big challenge will be making sure the vaccine works well in older people. The older you are, the less effective vaccines are. Your immune system—like the rest of your body—ages and is slower to recognize and attack invaders. That’s a big issue for a COVID-19 vaccine, since older people are the most vulnerable. We need to make sure they’re protected.
The shingles vaccine—which is also targeted to older people—combats this by amping up the strength of the vaccine. It’s possible we do something similar for COVID, although it might come with more side effects. Health authorities could also ask people over a certain age to get an additional dose.
Beyond safety and efficacy, there are a couple other factors to consider:
- How many doses will it be? A vaccine you only get once is easier and quicker to deliver. But we may need a multi-dose vaccine to get enough efficacy.
- How long does it last? Ideally, the vaccine will give you long-lasting protection. But we might end up with one that only stops you from getting sick for a couple months (like the seasonal flu vaccine, which protects you for about six months). If that happens, the short-term vaccine might be used while we work on a more durable one.
- How do you store it? Many common vaccines are kept at 4 degrees C. That’s around the temperature of your average refrigerator, so storage and transportation is easy. But RNA vaccines need to be stored at much colder temperature—as low as -80 degrees C—which will make reaching certain parts of the world more difficult.
My hope is that the vaccine we have 18 months from now is as close to “perfect” as possible. Even if it isn’t, we will continue working to improve it. After that happens, I suspect the COVID-19 vaccine will become part of the routine newborn immunization schedule.
Once we have a vaccine, though, we still have huge problems to solve. That’s because…
We need to manufacture and distribute at least 7 billion doses of the vaccine.
In order to stop the pandemic, we need to make the vaccine available to almost every person on the planet. We’ve never delivered something to every corner of the world before. And, as I mentioned earlier, vaccines are particularly difficult to make and store.
There’s a lot we can’t figure out about manufacturing and distributing the vaccine until we know what exactly we’re working with. For example, will we be able to use existing vaccine factories to make the COVID-19 vaccine?
What we can do now is build different kinds of vaccine factories to prepare. Each vaccine type requires a different kind of factory. We need to be ready with facilities that can make each type, so that we can start manufacturing the final vaccine (or vaccines) as soon as we can. This will cost billions of dollars. Governments need to quickly find a mechanism for making the funding for this available. Our foundation is currently working with CEPI, the WHO, and governments to figure out the financing.
Part of those discussions center on who will get the vaccine when. The reality is that not everyone will be able to get the vaccine at the same time. It’ll take months—or even years—to create 7 billion doses (or possibly 14 billion, if it’s a multi-dose vaccine), and we should start distributing them as soon as the first batch is ready to go.
Most people agree that health workers should get the vaccine first. But who gets it next? Older people? Teachers? Workers in essential jobs?
I think that low-income countries should be some of the first to receive it, because people will be at a much higher risk of dying in those places. COVID-19 will spread much quicker in poor countries because measures like physical distancing are harder to enact. More people have poor underlying health that makes them more vulnerable to complications, and weak health systems will make it harder for them to receive the care they need. Getting the vaccine out in low-income countries could save millions of lives. The good news is we already have an organization with expertise about how to do this in Gavi, the Vaccine Alliance.
With most vaccines, manufacturers sign a deal with the country where their factories are located, so that country gets first crack at the vaccines. It’s unclear if that’s what will happen here. I hope we find a way to get it out on an equitable basis to the whole world. The WHO and national health authorities will need to develop a distribution plan once we have a better understanding of what we’re working with.
Eventually, though, we’re going to scale this thing up so that the vaccine is available to everyone. And then, we’ll be able to get back to normal—and to hopefully make decisions that prevent us from being in this situation ever again.
It might be a bit hard to see right now, but there is a light at the end of the tunnel. We’re doing the right things to get a vaccine as quickly as possible. In the meantime, I urge you to continue following the guidelines set by your local authorities. Our ability to get through this outbreak will depend on everyone doing their part to keep each other safe.