Insurers and Private Equity Look to Join Forces to Further Consolidate Control of Americans’ Access to Health Care

With both Republicans and Democrats taking on these Goliaths individually, this could be a watershed moment for bi-partisan action.
The push and pull between providers and insurance companies is as old as our health payment system. Doctors have long argued insurers pay too little and that they too often interfere in patient care.
Dramatic increases in prior authorization, aggressive payment negotiations and less-generous reimbursement to doctors by Medicare Advantage plans show there’s little question the balance of power in this equation has swung toward payers.
These practices have led some doctors to look for outside investment, namely private equity, to keep their cash flow healthy and their operations functional. The trend of private equity acquisitions of physician practices is worthy of the federal scrutiny it has attracted. Insurers have noticed this trend, too, and appear ready to propose a profitable partnership.
Bloomberg recently reported that CVS/Aetna is looking for a private equity partner to invest in Oak Street Health, the primary care business CVS acquired for $9.5 billion last year. Oak Street is a significant player in primary care delivery, particularly for Americans on Medicare, with more than 100 clinics nationwide. CVS is said to be exploring a joint venture with a private equity firm to significantly expand Oak Street’s footprint and therefore also expand the parent corporation’s direct control over care for millions of seniors and disabled Americans across hundreds of communities.
Republicans have led scrutiny of pharmacy benefit managers on Capitol Hill. And Democratic attacks on private equity in health care have recently intensified. I hope, then, that both parties would find common ground in being watchful of a joint venture between private equity and one of the country’s largest PBMs, Caremark, also owned by CVS/Aetna.
The combination of health insurers and PBMs over the last decade – United Healthcare and Optum; CVS/Aetna and Caremark, and Cigna and Express Scripts – has increasingly handed a few large corporations the ability to approve or deny claims, set payment rates for care, choose what prescriptions to dispense, what prescriptions should cost, and how much patients must pay out-of-pocket for their medications before their coverage kicks in.
As enrollment in Medicare Advantage plans has grown to include a majority of the nation’s elderly and disabled people, we have seen insurers source record profits off the backs of the taxpayer-funded program. But in recent months, insurers have told investors they have had higher than expected Medicare Advantage claims – in particular CVS/Aetna, which took a hammering on Wall Street recently because its Medicare Advantage enrollees were using more health care services than company executives had expected.
It is natural, then, that one of the largest insurer-owned PBMs is looking to expand its hold on primary care for older Americans. Primary care is often the gateway to our health care system, driving referrals to specialists and procedures that lead to the largest claims insurers and their employer customers have to pay. By employing a growing number of primary care providers, CVS/Aetna can increasingly influence referrals to specialists and therefore the care or pharmacy benefit costs those patients may incur.
Control of primary care doctors holds another benefit for insurers: determination of what primary care doctor a patient sees.
People enrolled in an Aetna Medicare Advantage or employer-sponsored plan may find that care is easier to access at Oak Street clinics. Unfortunately, while that feels monopolistic and ethically alarming, this vertical integration has received relatively little scrutiny by lawmakers and regulators.
No law prevents an insurance company or PBM from kicking doctors it does not own out of network while creating preferential treatment for doctors directly employed by or closely affiliated with the corporate mothership.
In fact, the system largely incentivizes this. And shareholders expect insurers to keep up with their peers. As UnitedHealth Group has become increasingly aggressive in its acquisitions of physician practices – now employing or affiliated with about one in ten of the nation’s doctors – it has also become increasingly aggressive in its contract negotiations with physicians it does not control, particularly the specialists who depend on the referrals that come from primary care physicians.
That’s another area where looking to expand Oak Street Health makes smart business sense for CVS/Aetna. Specialist physicians are historically accustomed to higher compensation than primary care doctors and are used to striking hard-fought deals with insurers to stay in-network.
By controlling the flow of primary care referrals to specialists, CVS/Aetna can control what insurers have long-desired greater influence over: patient utilization. As a key driver of referrals to specialists in a specific market, CVS/Aetna will have even more power in contract negotiations with specialists.
As Oak Street’s clinics grow market share in the communities they serve, specialists in that market will feel even more pressured to stay in-network with Aetna and to refer prescriptions to CVS pharmacies. That has the dual benefit for CVS/Aetna of helping to predict what patients will be treated for once they go to a specialist and control over what the insurer will have to pay that specialist.
With different corporate owners, this sort of model could easily run afoul of the federal Anti-Kickback Statute and Stark Law.
No doctor or physician practice is allowed to receive anything of value for the referral of a patient. But that law only applies when there is separate ownership between the referring doctor and the specialist.
CVS/Aetna would clearly be securing value – in the form of lower patient utilization and effective reimbursement rates – under this model. But with Oak Street owned by CVS/Aetna and specialists forced to agree to lower reimbursement rates through negotiations with an insurer that appears separate from Oak Street, there’s no basis for a claim under the Stark Law. There may be antitrust implications, but those are more difficult and take longer to prove – and the fact the federal government cleared CVS/Aetna to acquire Oak Street Health last year wouldn’t help that argument.
This model is already of concern, which is why I continue to urge examination of increasing insurer control of physicians across the country. Their embrace of private equity to accelerate this model is truly alarming. And given Democrats’ recent focus on private equity in health care, they should work with their Republican colleagues who are rightly alarmed about the increasingly anti-competitive, monopolistic health insurance industry.
The CBO Health Insurance Status Report: Four Reasons it’s Overly Optimistic

In the Congressional Budget Office’ latest report on the status of health insurance coverage from the 2023 National Health Interview Survey released last week, a cautiously optimistic picture of coverage is presented:
- “In 2023, 25.0 million people of all ages (7.6%) were uninsured at the time of interview. This was lower than, but not significantly different from 2022, when 27.6 million people of all ages (8.4%) were uninsured. Among adults ages 18 64, 10.9% were uninsured at the time of interview, 23.0% had public coverage, and 68.1% had private health insurance coverage.
- The percentage of adults ages 18-64 who were uninsured in 2023 (10.9%) was lower than the percentage who were uninsured in 2022 (12.2%).
- Among children ages 0–17 years, 3.9% were uninsured, 44.2% had public coverage, and 54.0% had private health insurance coverage.
- The percentage of people younger than age 65 with exchange-based coverage increased from 3.7% in 2019 to 4.8% in 2023.”
That represents the highest level of coverage in modern history. Later, it adds important context: The percentage of adults ages 18–64 who were uninsured decreased between 2019 and 2023 for all family income groups shown except for adults in families with incomes greater than 400% FPL. Notably, a period in which the Covid-19 pandemic prompted federal government’s emergency funding so households and businesses could maintain their coverage.
- “Among adults with incomes below 100% FPL, the percentage who were uninsured in 2023 (20.2%) was lower than, but not significantly different from, the percentage who were uninsured in 2022 (22.7%).
- Among adults with incomes 100% to less than 200% FPL, the percentage who were uninsured decreased from 22.3% in 2022 to 19.1% in 2023.
- Among adults with incomes 200% to 400% FPL, the percentage who were uninsured decreased from 14.2% in 2022 to 11.5% in 2023.
- No significant difference was observed in the percentage of adults with incomes above 400% FPL who were uninsured between 2022 (4.1%) and 2023 (4.3%).”
- In 2023, among adults ages 18–64, the percentage who were uninsured was highest among health insurance coverage of any type was higher for those with higher household income but decreased coverage in 2023 correlated to ethnicity, non-expansion of state Medicaid programs: From 2019 to 2023.”
- And decreases in the ranks of the uninsured were noted across all ethnic groups:
- Among Hispanic adults, from 29.7% to 24.8%
- Among Black non-Hispanic adults, from 14.7% to 10.4% in 2023
- Among White non-Hispanic adults, decreased from 10.5% to 6.8%
- Among Asian non-Hispanic adults, from 8.8% to 4.4% in 2023.
The New York Times noted “The drops cut significantly into gaps between ethnic groups. The uninsured rate among Black Americans, for example, was almost 8% higher than for white Americans in 2010, and was only 4%higher in 2022. The data points to the broad effects of the Affordable Care Act, the landmark law President Barack Obama signed in 2010 that created new state and federal insurance marketplaces and expanded Medicaid to millions of adults. National uninsured rates have continued to drop in recent years, hitting a record low in early 2023.”
But the report also flags a reversal of the trend: “The uninsured share of the population will rise over the course of the next decade, before settling at 8.9% in 2034, largely as a result of the end of COVID-19 pandemic–related Medicaid policies, the expiration of enhanced subsidies available through the Affordable Care Act health insurance Marketplaces, and a surge in immigration that began in 2022. The largest increase in the uninsured population will be among adults ages 19–44. Employment-based coverage will be the predominant source of health insurance, and as the population ages, Medicare enrollment will grow significantly. After greater-than-expected enrollment in 2023, Marketplace enrollment is projected to reach an all-time high of twenty-three million people in 2025.”
My take:
A close reading of this report suggests its forecast might be overly optimistic. it paints a best-case picture of health insurance coverage that under-estimates the realities of household economics and marketplace trends and over-estimates the value proposition promoted by health insurers to their customers. My conclusion is based on four trends that suggest coverage might slip more than the report suggests:
- The affordability of healthcare insurance is increasingly problematic to lower- and middle-income households who face inflationary prices for housing, food, energy and transportation. The CBO report verifies that household income is key to coverage and working age populations are most-at risk of losing its protections. Subsidies to fund premiums for those eligible, employer plans that expose workers to high deductibles and increased non-covered services are likely to push fewer to enroll as premiums become unaffordable to working age adults and unattractive to their employers. As outlined in a sobering KFF analysis, half of the adult population is worried about the affordability of their healthcare—and that includes 48% who have health insurance. And wages in the working age population are not keeping pace with prices for food, shelter and energy, leaving healthcare expenses including their insurance premiums and out-of-pocket obligations at greater risk.
- The value proposition for health insurance coverage is eroding among employers, consumers and lawmakers. To large employers that provide employee insurance, medical costs are forcing benefits reduction or cessation altogether. Insurance has not negated their medical costs. To small employers, it’s an expensive bet to recruit and keep their workforce. To government sponsors (i.e. Medicare, Medicaid, VHA, et al), insurance is a necessary but increasingly expensive obligation with growing dependence on private insurers to administer their programs. State and federal regulators are keen to limit public spending and address disparities in their public insurance programs. All recognize that private insurers play a necessary role in the system and all recognize that confidence in health insurance protections is suspect. Thus, increased regulation of private insurers is likely though unwelcome by its members.
- Public funding for government payers will be increasingly limited increasing insurer dependence on private capital for sustainability and growth. Funding for Medicare, Medicaid, Veterans and Military Health, Public Health et al are dependent on appropriations and tax collections. All are structured to invite private insurer participation: all are seeing corporate insurers seize market share from their weaker competitors. The issues are complex and controversial as evidenced by the ongoing debates about fairness in Medicare Advantage and administration of Medicaid expansion among others. And polls indicate widespread dissatisfaction with the system and lack of confidence in its insurers, hospitals, physicians or the government to fix it.
- Access to private capital for private health insurers is shrinking enabling corporate insurers to play bigger roles in financing and delivering services. Private investments in healthcare services (i.e. hospitals, physicians, clinics) has slowed and momentum has shifted from sellers to buyers seeking less risk and higher returns. Capital deployment by corporate insurers i.e. UHG, HUM et al has resulted in vertically-integrated systems of health inclusive of physician services, drug distribution, ASCs and more. And funding for AI-investments that lower their admin costs and increase their contracting leverage with providers is a strategic advantage for corporate insurer that operate nationally at scale. Unless the federal government bridles their growth (which is unlikely), corporate insurers will control national coverage while others fail.
Thus, no one knows for sure what coverage will be in 2034 as presented in the CBO report. Its analysis appropriately considers medical inflation, population growth and an incremental shift to value-based purchasing in healthcare, but it fails to accommodate highly relevant changes in the capital markets, corporate insurer shareholder interests and voter sentiment.
P.S. This is an important week for healthcare: Today marks the two-year anniversary of the Supreme Court’s Dobbs decision that overturned Roe v. Wade, ending the constitutional right to an abortion that pushed reproductive rights to states.
And Thursday in Atlanta, President Joe Biden and former President Donald Trump will make history in the first presidential debate between an incumbent and a former president.
Reproductive rights will be a prominent theme along with immigration and border security as wedge issues for voters.
The economy and inflation are the issues of most consequence to most voters, so unless the campaigns directly link healthcare spending and out of pocket costs to voter angst about their household finances, not much will be said.
Notably, half of the U.S. population have unpaid medical bills and medical debt is directly related to their financial insecurity. Worth watching.
36 hospitals, health systems cutting jobs

A number of hospitals and health systems are reducing their workforces or jobs due to financial and operational challenges.
Below are workforce reduction efforts or job eliminations announced this year.
June
West Monroe, La.-based Glenwood Regional Medical Center, part of Dallas-based Steward Health Care, laid off 23 employees. Affected roles included leadership, a spokesperson for the hospital said in a statement shared with Becker’s.
Cleveland-based University Hospitals is reducing its leadership structure by more than 10% as part of more than 300 layoffs. COO Paul Hinchey, MD, told Becker’s C-suite level leaders and vice presidents were included in the cuts.
Portland-based Oregon Health & Science University told staff June 6 that it plans to lay off at least 500 employees, citing financial issues. The news follows the institution and Portland-based Legacy Health signing a binding, definitive agreement to come together as one health system under OHSU Health.
May
The All of Us Research Program, a collaboration of the University of Arizona in Tucson and Phoenix-based Banner Health, plans to lay off 45 workers due to reduced federal research funding, according to an Arizona WARN notice filed May 28. The program, launched in 2018, is part of HHS’ National Institutes of Health.
Burlington, Mass.-based Tufts Medicine will lay off 174 employees due to industry challenges, the health system confirmed in a May 21 statement shared with Becker’s. The layoffs, which have varying effective dates, will primarily affect administrative and non-direct patient care roles. Some leadership roles were affected, a spokesperson told Becker’s.
Doral, Fla.-based Sanitas Medical Center laid off 56 employees between May 17 and May 20. Some of the affected roles included nine care coordinators, one care educator, and two case managers, according to a May 20 WARN notice accessed by Becker’s.
Select Specialty Hospital in Longview, Texas, will close on or about June 30, affecting 94 employees, Becker’s has confirmed. The hospital, operated by Mechanicsburg, Pa.-based Select Medical, is a 32-bed, critical illness recovery facility.
White Rock Medical Center in Dallas laid off nearly 35% of its staff. The hospital temporarily stopped taking patients transported by emergency medical services due to the layoffs, The Dallas Morning News reported. It has since resumed accepting those patients.
Oakland-based Kaiser Foundation Hospitals is laying off 76 workers in California. The layoffs primarily affect employees in IT and marketing, according to regulatory documents filed with the state May 1.
April
Pittsburgh-based UPMC will lay off approximately 1,000 employees. The layoffs, which represent more than 1% of the health system’s 100,000 workforce will primarily affect nonclinical, administrative and non-member-facing employees.
Union Springs, Ala.-based Bullock County Hospital laid off 95 employees beginning April 9, according to regulatory documents filed with the state. The layoffs occurred as Bullock seeks to become a rural emergency hospital and is ending psychiatric services as part of the shift, AL.com reported April 25.
Jackson Health System reduced compensation programs for senior leaders; laid off fewer than 25 people, including one hospital CEO; and froze many vacant positions, especially in support and nonclinical areas, a spokesperson for the Miami-based organization confirmed to Becker’s. President and CEO Carlos Migoya shared these efforts in a message to staff, citing financial challenges.
Coos Bay, Ore.-based Bay Area Hospital plans to conduct layoffs as it outsources its revenue cycle management operations, a spokesperson for the hospital confirmed to Becker’s. The transition will affect 27 positions.
Manchester, N.H.-based Catholic Medical Center plans to cut 142 positions, including 54 layoffs. An April 18 letter to employees from CMC president and CEO Alex Walker, obtained by Becker’s, said cuts would occur through the 54 staff eliminations, open position cuts, reduced hours, planned departures, and resource redeployment in satellite locations for CMC.
Marshfield (Wis.) Clinic Health System will lay off furloughed staff, effective in early May. The health system furloughed about 3% of its workforce in January, affecting positions mostly in non-patient-seeing departments, including leadership roles.
Norwalk, Ohio-based Fisher-Titus Medical Center laid off some workers in nonclinical roles and reduced hours for others. Seven employees, about 0.5% of the health system’s workforce, were laid off April 1. Work hours were reduced for another 10 positions, a hospital spokesperson told Becker’s.
March
Robbinsdale, Minn.-based North Memorial Health is laying off 103 employees in clinical and nonclinical roles, citing financial challenges. The layoffs affect several services across the two-hospital system.
AHMC’s San Gabriel (Calif.) Valley Medical Center is laying off 62 workers, according to regulatory documents filed with the state March 13. The layoffs take effect May 13.
Miami-based North Shore Medical Center, part of Steward Health Care, started conducting layoffs as part of cuts to some of its programs amid the Dallas-based health system’s continued financial struggles. Around 152 workers represented by 1199SEIU were laid off, a union spokesperson confirmed. However that number could be higher as their members do not represent every employee at NSMC, the spokesperson said.
Oakland, Calif.-based Kaiser Foundation Hospitals is laying off more than 70 employees. The layoffs primarily affect those in IT roles.
February
Lion Star, the group that operates Nacogdoches (Texas) Memorial Hospital, is closing four of its clinics on March 22, which will result in fewer than 50 layoffs, a Lion Star spokesperson confirmed to Becker’s. No additional layoffs are planned.
Little Rock-based Arkansas Heart Hospital has laid off fewer than 50 employees since the beginning of 2024, citing low reimbursement rates. The layoffs affected lower-paying positions, Bruce Murphy, MD, CEO of the hospital, said, according to Arkansas Business.
Cincinnati-based Mercy Health will lay off some call center positions. The system attributed the move to its partnership with a third party to operate its enterprise contact center for primary care scheduling.
Ridgecrest (Calif.) Regional Hospital announced more layoffs to avoid closure. It is laying off 31 more employees, including seven licensed vocational nurses and four registered nurses, two months after it announced plans to lay off nearly 30 others and suspend its labor and delivery unit, Bakersfield.com reported Feb. 15.
Medford, Ore.-based Asante health system laid off about 3% of its workforce. The layoffs primarily affected administrative and support roles and were necessary to offset “financial headwinds” over the past several years, according to a report from NBC affiliate KOBI-TV, which is based on an internal memo sent to staff Feb. 9.
Oakdale, Calif.-based Oak Valley Hospital District is scaling back services and laying off workers to improve its finances. The hospital said in a Feb. 2 statement shared with Becker’s that it will close its five-bed intensive care unit, discontinue its family support network department and lay off 28 employees, including those in senior management and supervisor positions.
Chicago-based Rush University System for Health laid off an undisclosed number of workers in administrative and leadership positions, citing “financial headwinds affecting healthcare providers nationwide.” No additional information was provided about the layoffs, including the number of affected employees.
University of Chicago Medical Center laid off about 180 employees, or less than 2% of its roughly 13,000-person workforce. The majority of affected positions are not direct patient facing, the organization said in a statement shared with Becker’s.
Fountain Valley, Calif.-based MemorialCare laid off 72 workers due to restructuring efforts at its Long Beach (Calif.) Medical Center and Long Beach, Calif.-based Miller Children’s and Women’s Hospital. The layoffs include 13 positions at Long Beach Medical Center’s outpatient retail pharmacy, which is closing Feb. 2, a spokesperson for MemorialCare said in a statement shared with Becker’s.
January
George Washington University Hospital in Washington, D.C., part of King of Prussia, Pa.-based Universal Health Services, is laying off “less than 3%” of its employees. The move is attributed to restructuring efforts.
Amarillo-based Northwest Texas Healthcare System, also part of Universal Health Services, announced plans to lay off a “limited number of positions.” The move is attributed to restructuring efforts.
Lehigh Valley Health Network is cutting its chiropractic services and laying off 10 chiropractors. The layoffs are effective April 12 and due to restructuring. The Allentown, Pa.-based health system has 10 chiropractic locations, according to its website.
Central Maine Healthcare is laying off 45 employees as part of management reorganization. The Lewiston-based system, which also ended urgent care services at its Maine Urgent Care on Sabattus Street in Lewiston on Jan. 12, has 3,100 employees total.
University of Vermont Health Network, based in Burlington, is cutting 130 open positions. The move is part of the health system’s efforts to reduce expenses by $20 million.
Med-Trans, a medical transport provider based in Lewisville, Texas, closed its UF Health ShandsCair base serving Gainesville, Fla.-based UF Health Shands Hospital on Jan. 10 due to decreased transportation demands. The move also resulted in layoffs, a spokesperson for UF Health, the hospital’s parent company, told Becker’s in a statement.
RWJBarnabas Health, based in West Orange, N.J., is laying off 79 employees, according to documents filed with the state on Jan. 8. The layoffs are effective March 31 and April 5. A spokesperson for the health system told Becker’s that 74 of the positions were “time-limited information technology training job functions.” The other layoffs were due to closure of an urgent care center.
Quote of the Day – On Courage
BIG INSURANCE 2023: Revenues reached $1.39 trillion thanks to taxpayer-funded Medicaid and Medicare Advantage businesses
The Affordable Care Act turned 14 on March 23. It has done a lot of good for a lot of people, but big changes in the law are urgently needed to address some very big misses and consequences I don’t believe most proponents of the law intended or expected.
At the top of the list of needed reforms: restraining the power and influence of the rapidly growing corporations that are siphoning more and more money from federal and state governments – and our personal bank accounts – to enrich their executives and shareholders.
I was among many advocates who supported the ACA’s passage, despite the law’s ultimate shortcomings. It broadened access to health insurance, both through government subsidies to help people pay their premiums and by banning prevalent industry practices that had made it impossible for millions of American families to buy coverage at any price. It’s important to remember that before the ACA, insurers routinely refused to sell policies to a third or more applicants because of a long list of “preexisting conditions” – from acne and heart disease to simply being overweight – and frequently rescinded coverage when policyholders were diagnosed with cancer and other diseases.
While insurance company executives were publicly critical of the law, they quickly took advantage of loopholes (many of which their lobbyists created) that would allow them to reap windfall profits in the years ahead – and they have, as you’ll see below.
Among other things, the ACA made it unlawful for most of us to remain uninsured (although Congress later repealed the penalty for doing so). But, notably, it did not create a “public option” to compete with private insurers, which many advocates and public policy experts contended would be essential to rein in the cost of health insurance. Many other reform advocates insisted – and still do – that improving and expanding the traditional Medicare program to cover all Americans would be more cost-effective and fair.
I wrote and spoke frequently as an industry whistleblower about what I thought Congress should know and do, perhaps most memorably in an interview with Bill Moyers. During my Congressional testimony in the months leading up to the final passage of the bill in 2010, I told lawmakers that if they passed it without a public option and acquiesced to industry demands, they might as well call it “The Health Insurance Industry Profit Protection and Enhancement Act.”
A health plan similar to Medicare that could have been a more affordable option for many of us almost happened, but at the last minute, the Senate was forced to strip the public option out of the bill at the insistence of Sen. Joe Lieberman (I-Connecticut), who died on March 27, 2024. The Senate did not have a single vote to spare as the final debate on the bill was approaching, and insurance industry lobbyists knew they could kill the public option if they could get just one of the bill’s supporters to oppose it. So they turned to Lieberman, a former Democrat who was Vice President Al Gore’s running mate in 2000 and who continued to caucus with Democrats. It worked. Lieberman wouldn’t even allow a vote on the bill if it created a public option. Among Lieberman’s constituents and campaign funders were insurance company executives who lived in or around Hartford, the insurance capital of the world. Lieberman would go on to be the founding chair of a political group called No Labels, which is trying to find someone to run as a third-party presidential candidate this year.
The work of Big Insurance and its army of lobbyists paid off as insurers had hoped. The demise of the public option was a driving force behind the record profits – and CEO pay – that we see in the industry today.
The good effects of the ACA:
Nearly 49 million U.S. residents (or 16%) were uninsured in 2010. The law has helped bring that down to 25.4 million, or 8.3% (although a large and growing number of Americans are now “functionally uninsured” because of unaffordable out-of-pocket requirements, which President Biden pledged to address in his recent State of the Union speech).
The ACA also made it illegal for insurers to refuse to sell coverage to people with preexisting conditions, which even included birth defects, or charge anyone more for their coverage based on their health status; it expanded Medicaid (in all but 10 states that still refuse to cover more low-income individuals and families); it allowed young people to stay on their families’ policies until they turn 26; and it required insurers to spend at least 80% of our premiums on the health care goods and services our doctors say we need (a well-intended provision of the law that insurers have figured out how to game).
The not-so-good effects of the ACA:
As taxpayers and health care consumers, we have paid a high price in many ways as health insurance companies have transformed themselves into massive money-making machines with tentacles reaching deep into health care delivery and taxpayers’ pockets.
To make policies affordable in the individual market, for example, the government agreed to subsidize premiums for the vast majority of people seeking coverage there, meaning billions of new dollars started flowing to private insurance companies. (It also allowed insurers to charge older Americans three times as much as they charge younger people for the same coverage.) Even more tax dollars have been sent to insurers as part of the Medicaid expansion. That’s because private insurers over the years have persuaded most states to turn their Medicaid programs over to them to administer.
Insurers have bulked up incredibly quickly since the ACA was enacted through consolidation, vertical integration, and aggressive expansion into publicly financed programs – Medicare and Medicaid in particular – and the pharmacy benefit space. Premiums and out-of-pocket requirements, meanwhile, have soared.
We invite you to take a look at how the ascendency of health insurers over the past several years has made a few shareholders and executives much richer while the rest of us struggle despite – and in some cases because of – the Affordable Care Act.
BY THE NUMBERS
In 2010, we as a nation spent $2.6 trillion on health care. This year we will spend almost twice as much – an estimated $4.9 trillion, much of it out of our own pockets even with insurance.
In 2010, the average cost of a family health insurance policy through an employer was $13,710. Last year, the average was nearly $24,000, a 75% increase.
The ACA, to its credit, set an annual maximum on how much those of us with insurance have to pay before our coverage kicks in, but, at the insurance industry’s insistence, it goes up every year. When that limit went into effect in 2014, it was $12,700 for a family. This year, it has increased by 48%, to $18,900. That means insurers can get away with paying fewer claims than they once did, and many families have to empty their bank accounts when a family member gets sick or injured. Most people don’t reach that limit, but even a few hundred dollars is more than many families have on hand to cover deductibles and other out-of-pocket requirements. Now 100 million Americans – nearly one of every three of us – are mired in medical debt, even though almost 92% of us are presumably “covered.” The coverage just isn’t as adequate as it used to be or needs to be.
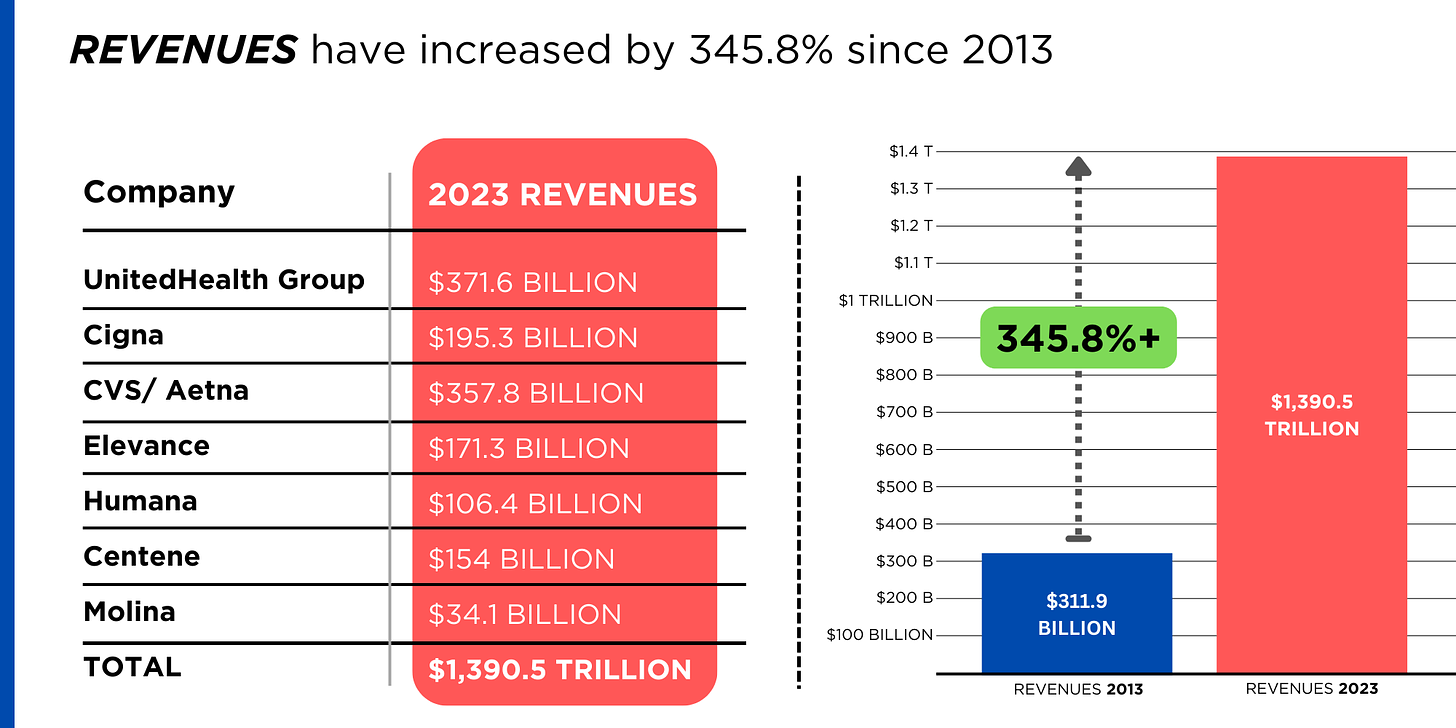
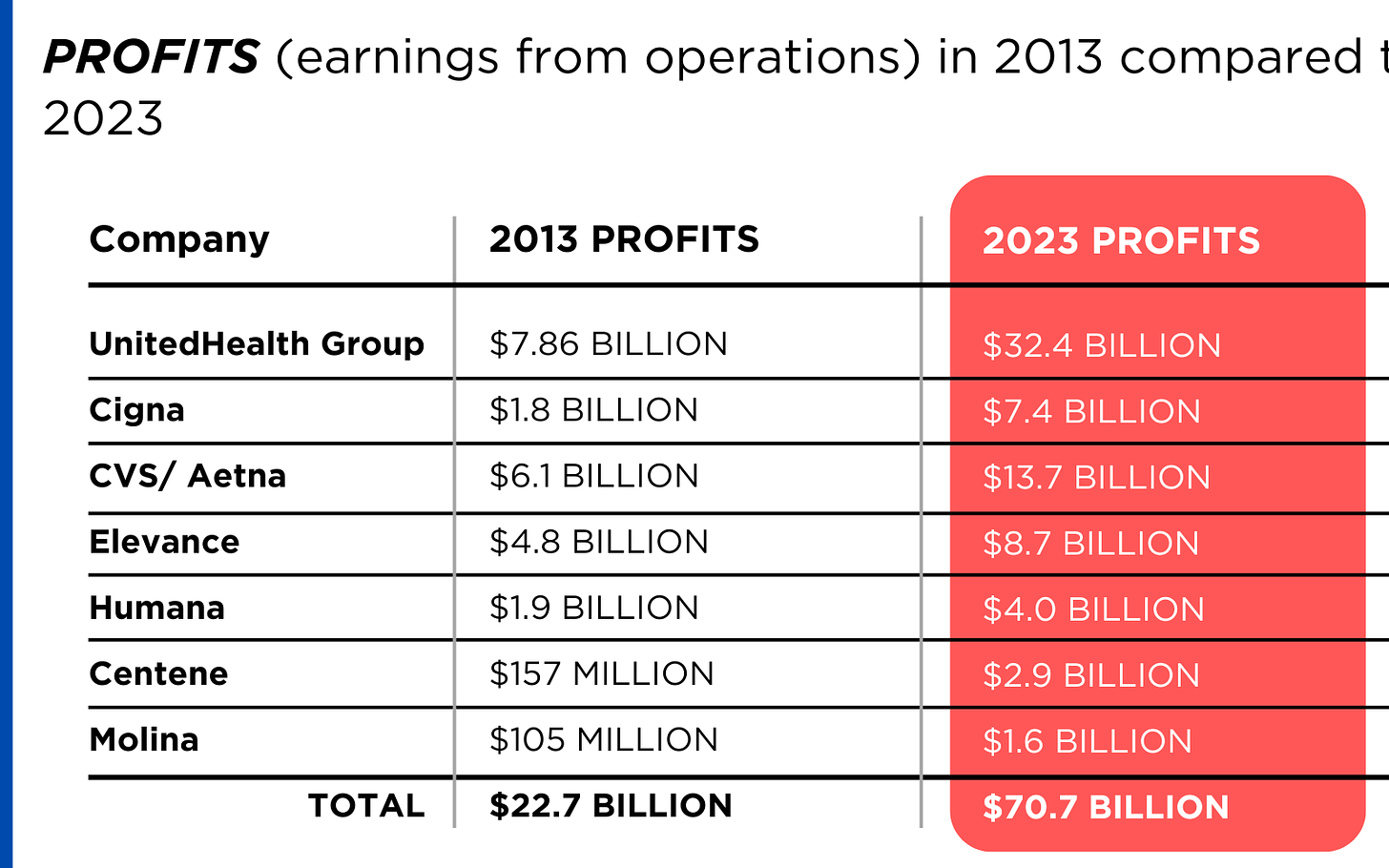
Meanwhile, insurance companies had a gangbuster 2023. The seven big for-profit U.S. health insurers’ revenues reached $1.39 trillion, and profits totaled a whopping $70.7 billion last year.
SWEEPING CHANGE, CONSOLIDATION–AND HUGE PROFITS FOR INVESTORS
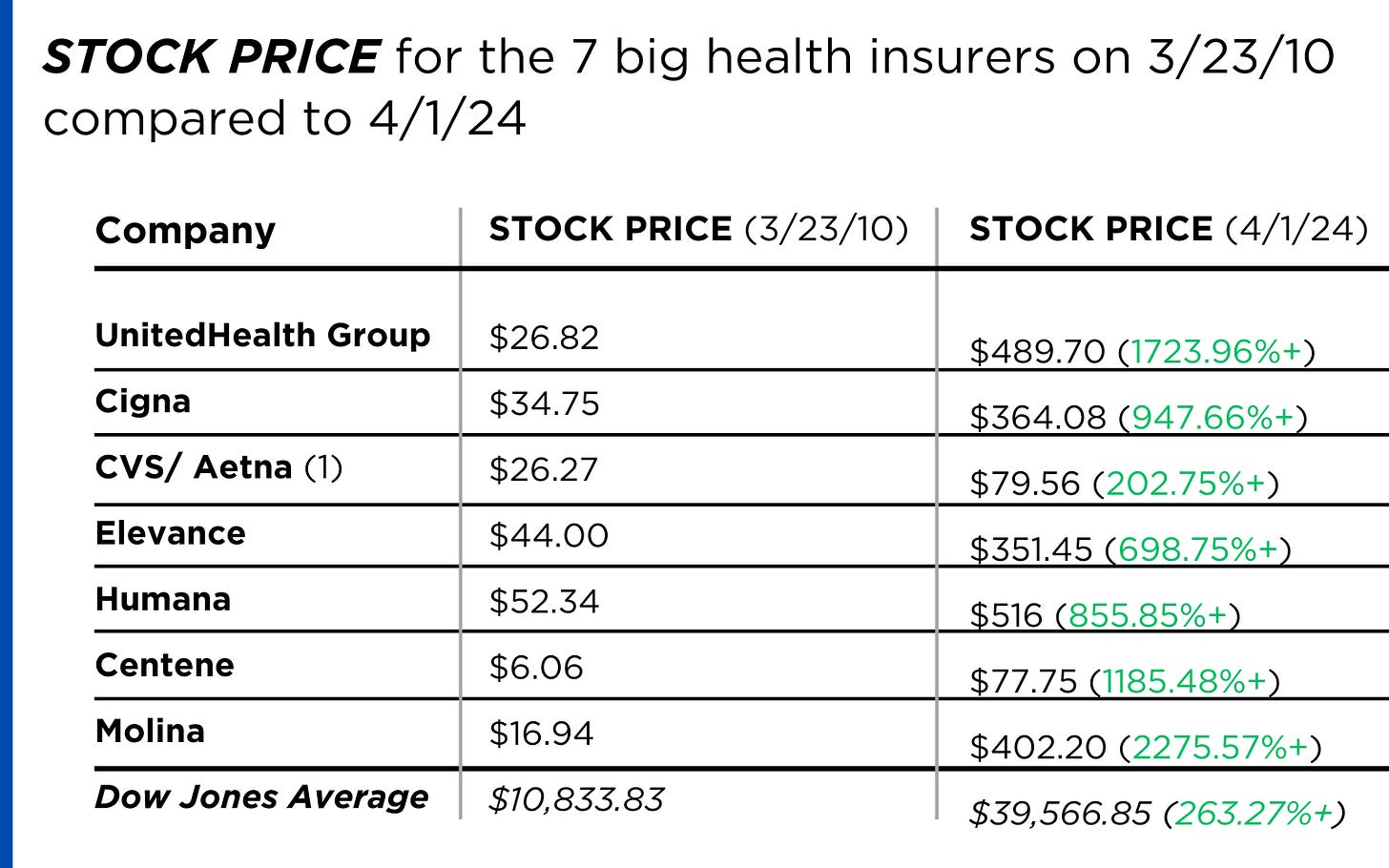
Insurance company shareholders and executives have become much wealthier as the stock prices of the seven big for-profit corporations that control the health insurance market have skyrocketed.
REVENUES collected by those seven companies have more than tripled (up 346%), increasing by more than $1 trillion in just the past ten years.
PROFITS (earnings from operations) have more than doubled (up 211%), increasing by more than $48 billion.
The CEOs of these companies are among the highest paid in the country. In 2022, the most recent year the companies have reported executive compensation, they collectively made $136.5 million.

U.S. HEALTH PLAN ENROLLMENT
Enrollment in the companies’ health plans is a mix of “commercial” policies they sell to individuals and families and that they manage for “plan sponsors” – primarily employers and unions – and government/enrollee-financed plans (Medicare, Medicaid, Tricare for military personnel and their dependents and the Federal Employee Health Benefits program).
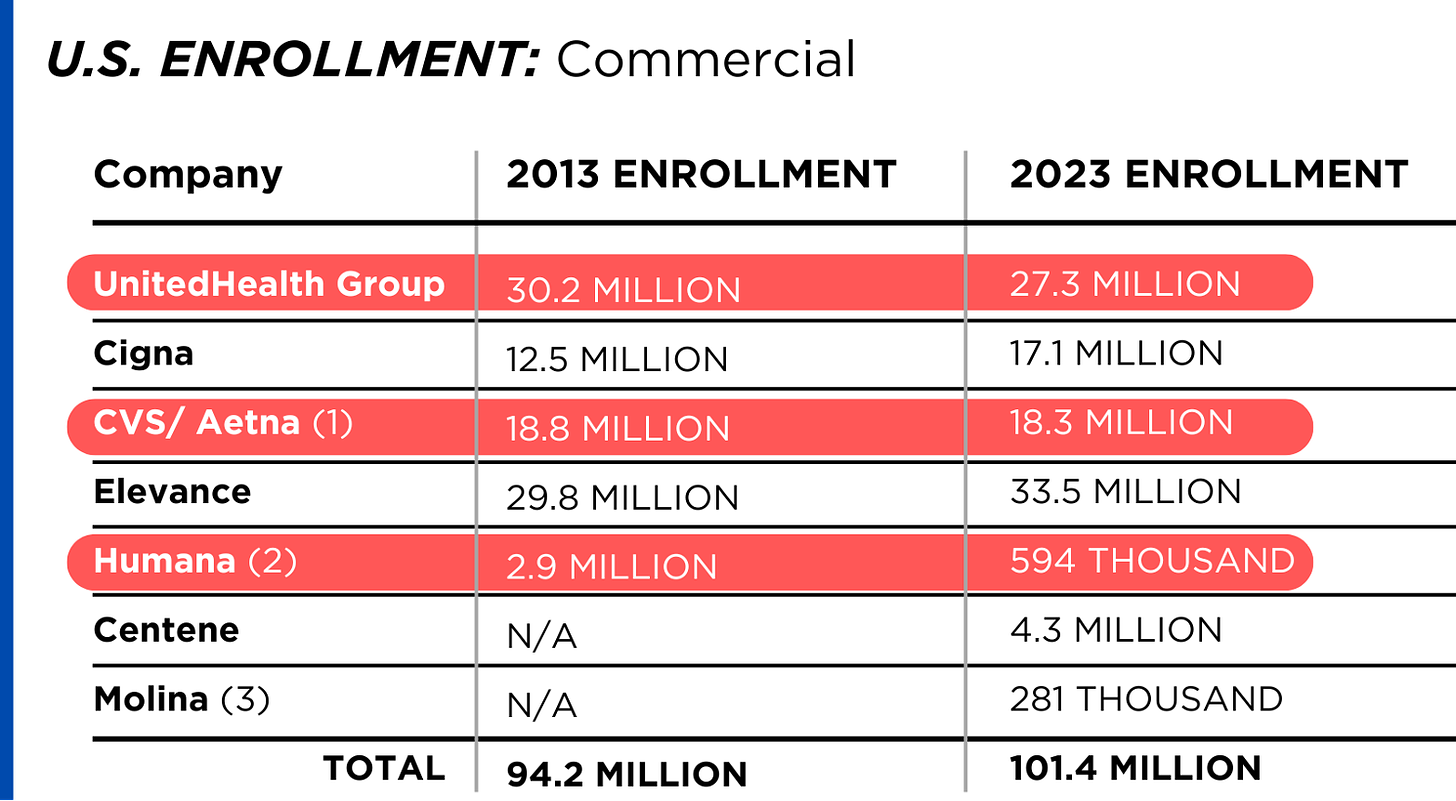
Enrollment in their commercial plans grew by just 7.65% over the 10 years and declined significantly at UnitedHealth, CVS/Aetna and Humana. Centene and Molina picked up commercial enrollees through their participation in several ACA (Obamacare) markets in which most enrollees qualify for federal premium subsidies paid directly to insurers.
While not growing substantially, commercial plans remain very profitable because insurers charge considerably more in premiums now than a decade ago.
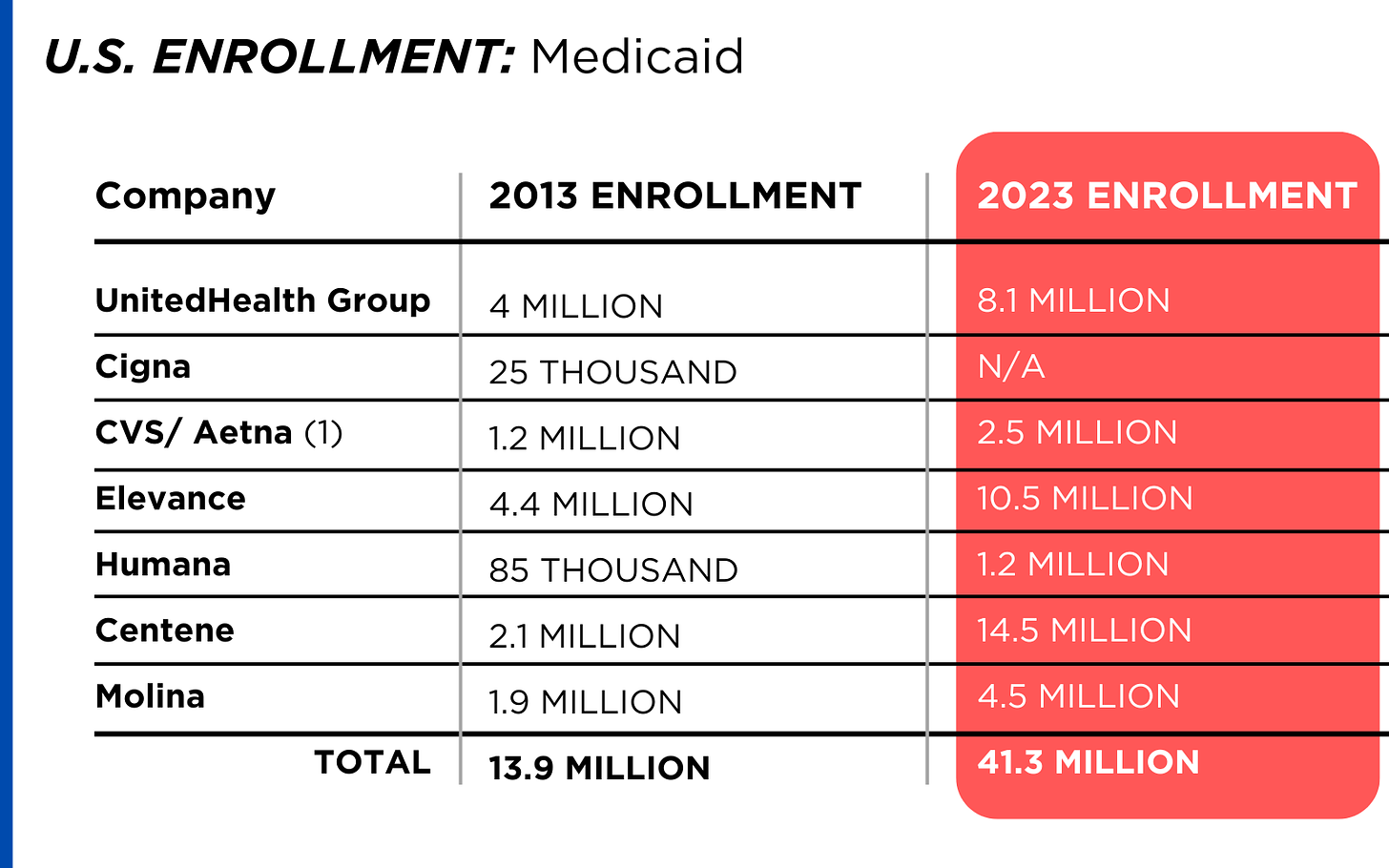
By contrast, enrollment in the government-financed Medicaid and Medicare Advantage programs has increased 197% and 167%, respectively, over the past 10 years.
Of the 65.9 million people eligible for Medicare at the beginning of 2024, 33 million, slightly more than half, enrolled in a private Medicare Advantage plan operated by either a nonprofit or for-profit health insurer, but, increasingly, three of the big for-profits grabbed most new enrollees.
Of the 1.7 million new Medicare Advantage enrollees this year, 86% were captured by UnitedHealth, Humana and Aetna.
Those three companies are the leaders in the Medicare Advantage business among the for-profit companies, and, according to the health care consulting firm Chartis, are taking over the program “at breakneck speed.”
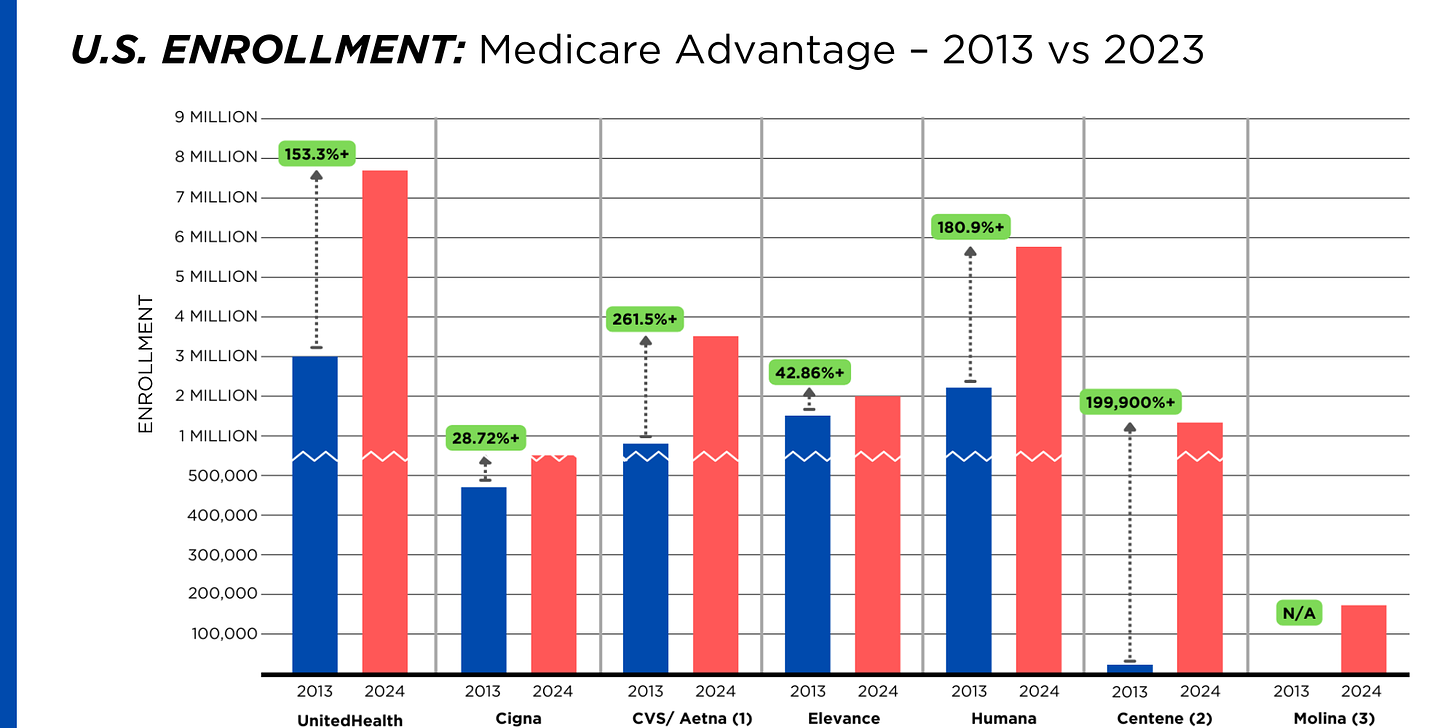
It is worth noting that although four companies saw growth in their Medicare Supplement enrollment over the decade, enrollment in Medicare Supplement policies has been declining in more recent years as insurers have attracted more seniors and disabled people into their Medicare Advantage plans.
OTHER FEDERAL PROGRAMS
In addition to the above categories, Humana and Centene have significant enrollment in Tricare, the government-financed program for the military. Humana reported 6 million military enrollees in 2023, up from 3.1 million in 2013. Centene reported 2.8 million in 2023. It did not report any military enrollment in 2013.
Elevance reported having 1.6 million enrollees in the Federal Employees Health Benefits Program in 2023, up from 1.5 million in 2013. That total is included in the commercial enrollment category above.
PBMs
As with Medicare Advantage, three of the big seven insurers control the lion’s share of the pharmacy benefit market (and two of them, UnitedHealth and CVS/Aetna, are also among the top three in signing up new Medicare Advantage enrollees, as noted above). CVS/Aetna’s Caremark, Cigna’s Express Scripts and UnitedHealth’s Optum Rx PBMs now control 80% of the market.
At Cigna, Express Scripts’ pharmacy operations now contribute more than 70% to the company’s total revenues. Caremark’s pharmacy operations contribute 33% to CVS/Aetna’s total revenues, and Optum Rx contributes 31% to UnitedHealth’s total revenues.
WHAT TO DO AND WHERE TO START
The official name of the ACA is the Patient Protection and Affordable Care Act. The law did indeed implement many important patient protections, and it made coverage more affordable for many Americans.
But there is much more Congress and regulators must do to close the loopholes and dismantle the barriers erected by big insurers that enable them to pad their bottom lines and reward shareholders while making health care increasingly unaffordable and inaccessible for many of us.
Several bipartisan bills have been introduced in Congress to change how big insurers do business. They include curbing insurers’ use of prior authorization, which often leads to denials and delays of care; requiring PBMs to be more “transparent” in how they do business and banning practices many PBMs use to boost profits, including spread pricing, which contributes to windfall profits; and overhauling the Medicare Advantage program by instituting a broad array of consumer and patient protections and eliminating the massive overpayments to insurers.
And as noted above, President Biden has asked Congress to broaden the recently enacted $2,000-a-year cap on prescription drugs to apply to people with private insurance, not just Medicare beneficiaries. That one policy change could save an untold number of lives and help keep millions of families out of medical debt. (A coalition of more than 70 organizations and businesses, which I lead, supports that, although we’re also calling on Congress to reduce the current overall annual out-of-pocket maximum to no more than $5,000.)
I encourage you to tell your members of Congress and the Biden administration that you support these reforms as well as improving, strengthening and expanding traditional Medicare. You can be certain the insurance industry and its allies are trying to keep any reforms that might shrink profit margins from becoming law.
Risant Health plans to acquire North Carolina system

Risant Health, a nonprofit formed under Oakland, Calif.-based Kaiser Permanente, has signed a definitive agreement to acquire Greensboro, N.C.-based Cone Health.
The news comes less than three months after Risant acquired its first health system, Danville, Pa.-based Geisinger Health. If the transaction closes, Cone Health will operate independently as a regional and community-based health system under Risant, which supports organizations with technology and services to improve outcomes and lower care costs in diverse business models.“Cone Health’s impressive work for decades in moving value-based care forward aligns so well with Risant Health’s vision for the future of healthcare. Their longstanding success and deep commitment to providing high-quality care to North Carolina communities make them an ideal fit to become a part of Risant Health,” CEO, Jaewon Ryu, MD, said in a June 21 news release. “We will work together to share our industry-leading expertise and innovation to expand access to value-based care to more people in the communities we serve.”
Cone Health includes four acute-care hospitals, a behavioral health facility, three ambulatory surgery centers, eight urgent care centers and more than 120 physician practices, according to its website. It has more than 13,000 employees and over 700 physicians, along with 1,800 partner physicians. “As part of Risant Health, Cone Health will build upon its long track record of success making evidence-based health care more accessible and affordable for more people. The people across the Triad will be among the first to benefit,” Cone Health President and CEO Mary Jo Cagle, MD, said.
Cone Health will maintain its brand, name and mission, and maintain its own board, CEO and leadership team. It will continue to work with health plans, provider organizations and independent physicians. Dr. Cagle said she does not anticipate changes in the types of care Cone Health provides as a result of becoming part of Risant. The proposed transaction is subject to regulatory approvals and closing conditions.
Pandemic rent inflation is still working its way through the economy
Everybody is waiting for rent relief to help bring overall inflation down. It might take longer than conventional wisdom suggests.
Why it matters:
A surge in market rents in 2021 and 2022 still has a ways to go in fully working its way through the economy, despite moderation in market rents since then, a new paper from a Boston Fed economist finds.
- As a result, rents are on track to exert upward pressure on overall inflation for quite a while to come, the paper argues, a headwind to bringing inflation down to the Fed’s 2% target.
The big picture:
Rents soared during and immediately after the pandemic as Americans sought bigger homes and were flush with higher paychecks and pent-up savings. But private-sector indicators of market rents rose much faster than the rent numbers calculated for the Consumer Price Index and other inflation indicators at that time.
- That’s because market rent data only encompasses people signing new leases. Many existing tenants saw no immediate change — perhaps because they had long-term leases in place, or landlords were reluctant to raise rent on existing tenants, or local laws constrained rent hikes.
- But over time, those leases turn over, with more renters paying the higher market prices. That process is still underway, even though market rents have risen less in 2023 and 2024, according to the analysis from the Boston Fed’s Christopher D. Cotton.
By the numbers:
Compared to 2019 levels, there is a 6 percentage point gap between rents on new leases and the shelter inflation shown in the CPI.
- The process of higher market rents filtering through the inflation data is on track to add 0.7 percentage point to the core Consumer Price Index over the next year and 0.3 percentage points to core inflation using the Fed’s preferred gauge, Cotton finds.
- “The fact that market rents remain 6% higher than CPI-shelter relative to pre-pandemic implies that CPI-shelter will grow more quickly than market rents for the foreseeable future,” Cotton tells Axios.
Of note:
Fed vice chair Philip Jefferson noted last month that “market rents adjust more quickly to economic conditions than what landlords charge their existing tenants.”
- “This lag suggests that the large increase in market rents during the pandemic is still being passed through to existing rents and may keep housing services inflation elevated for a while longer,” Jefferson said.
The intrigue:
One risk to watch is that even once the pandemic-era rent inflation has worked its way through the data, there could be a new surge in market rents due to under-supply.
- Construction of new multifamily housing has plunged below pre-pandemic levels in recent months as builders grapple with high interest rates.
Sign of the Times – Streamlining the Work Force
48 health systems with strong finances

Here are 48 health systems with strong operational metrics and solid financial positions, according to reports from credit rating agencies Fitch Ratings and Moody’s Investors Service released in 2024.
AdventHealth has an “AA” rating and stable outlook with Fitch. The rating is based on the Altamonte Springs, Fla.-based system’s competitive market position—especially in its core Florida markets—and its financial profile, Fitch said.
Advocate Health members Advocate Aurora Health and Atrium Health have “Aa3” ratings and positive outlooks with Moody’s. The ratings are supported by the Charlotte, N.C.-based system’s significant scale, strong market share across several major metro areas, and good financial performance and liquidity, Moody’s said.
Ann & Robert H. Lurie Children’s Hospital of Chicago has an “AA” rating and stable outlook with Fitch. The rating is supported by the system’s strong balance sheet with low leverage ratios derived from modest debt, Fitch said.
Avera Health has an “AA-” rating and a stable outlook with Fitch. The rating reflects the Sioux Falls, S.D.-based system’s strong operating risk and financial profile assessments, and significant size and scale, Fitch said.
Beacon Health System has an “AA-” rating and stable outlook with Fitch. Fitch said the rating reflects the strength of the South Bend, Ind.-based system’s balance sheet.
Carle Health has an “AA-” rating and stable outlook with Fitch. The rating reflects the Urbana, Ill.-based system’s distinctly leading market position over a broad service area and Fitch’s expectation that the system will sustain its strong capital-related ratios in the context of the system’s midrange revenue defensibility and strong operating risk profile assessments.
Carilion Clinic has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the Roanoke, Va.-based system’s scale, regional significance as a tertiary referral system with broad geographic capture, and a highly integrated physician base with a well-defined culture, Moody’s said.
Cedars-Sinai Health System has an “AA-” rating and a stable outlook with Fitch. The rating reflects the Los Angeles-based system’s consistent historical profitability and its strong liquidity metrics, historically supported by significant philanthropy, Fitch said.
Children’s Health has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the Dallas-based system’s continued strong performance from a focus on high margin and tertiary services, as well as a distinctly leading market share, Moody’s said.
Children’s Hospital Medical Center of Akron (Ohio) has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the system’s large primary care physician network, long-term collaborations with regional hospitals, and leading market position as its market’s only dedicated pediatric provider, Moody’s said.
Children’s Hospital of Orange County has an “AA-” rating and a stable outlook with Fitch. The rating reflects the Orange, Calif.-based system’s position as the leading provider for pediatric acute care services in Orange County, a position solidified through its adult hospital and regional partnerships, ambulatory presence, and pediatric trauma status, Fitch said.
Children’s Minnesota has an “AA” rating and stable outlook with Fitch. The rating reflects the Minneapolis-based system’s strong balance sheet, robust liquidity position, and dominant pediatric market position, Fitch said.
Cincinnati Children’s Hospital Medical Center has an “Aa2” rating and stable outlook with Moody’s. The rating is supported by its national and international reputation in clinical services and research, Moody’s said.
Cleveland Clinic has an “Aa2” rating and stable outlook with Moody’s. The rating reflects the system’s strength as an international brand in highly complex clinical care and research and centralized governance model, the ratings agency said.
Cook Children’s Medical Center has an “Aa2” rating and stable outlook with Moody’s. The ratings agency said the Fort Worth, Texas-based system will benefit from revenue diversification through its sizable health plan, large physician group, and an expanding North Texas footprint.
El Camino Health has an “AA” rating and a stable outlook with Fitch. The rating reflects the Mountain View, Calif.-based system’s strong operating profile assessment with a history of generating double-digit operating EBITDA margins anchored by a service area that features strong demographics as well as a healthy payer mix, Fitch said.
Froedtert ThedaCare Health has an “AA” rating and stable outlook with Fitch. The rating reflects the Milwaukee-based system’s solid market position, track record of strong utilization and operations, and strong financial profile, Fitch said.
Hoag Memorial Hospital Presbyterian has an “AA” rating and stable outlook with Fitch. The Newport Beach, Calif.-based system’s rating is supported by its strong operating risk assessment, leading market position in its immediate service area, and strong financial profile, Fitch said.
Inspira Health has an “AA-” rating and stable outlook with Fitch. The rating reflects Fitch’s expectation that the Mullica Hill, N.J.-based system will return to strong operating cash flows following the operating challenges of 2022 and 2023, as well as the successful integration of Inspira Medical Center of Mannington (formerly Salem Medical Center).
JPS Health Network has an “AA” rating and stable outlook with Fitch. The rating reflects the Fort Worth, Texas-based system’s sound historical and forecast operating margins, the ratings agency said.
Mass General Brigham has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the Somerville, Mass.-based system’s strong reputation for clinical services and research at its namesake academic medical center flagships that drive excellent patient demand and help it maintain a strong market position, Moody’s said.
Mayo Clinic has an “Aa2” rating and stable outlook with Moody’s. The rating reflects the Rochester, Minn.-based system’s preeminent reputation for clinical care and research, including new discoveries and cutting-edge treatment, Moody’s said.
McLaren Health Care has an “AA-” rating and stable outlook with Fitch. The rating reflects the Grand Blanc, Mich.-based system’s leading market position over a broad service area covering much of Michigan, the ratings agency said.
Med Center Health has an “AA-” rating and stable outlook with Fitch. The rating reflects the Bowling Green, Ky.-based system’s strong operating risk assessment and leading market position in a primary service area with favorable population growth, Fitch said.
Memorial Healthcare System has an “Aa3” rating and stable outlook with Moody’s. Moody’s said the rating reflects that the Hollywood, Fla.-based system will continue to benefit from good strategic positioning of its large, diversified geographic footprint.
Memorial Hermann Health System has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the Houston-based system’s leading and expanding market position and strong demand in a growing region, Moody’s said.
Methodist Health System has an “Aa3” rating and stable outlook with Moody’s. Moody’s said the rating reflects the Dallas-based system’s consistently strong operating performance, excellent liquidity, and very good market position.
Nationwide Children’s Hospital has an “Aa2” rating and stable outlook with Moody’s. The rating reflects the Columbus, Ohio-based system’s strong market position in pediatric services, growing statewide and national reputation, and continued expansion strategies.
Nicklaus Children’s Hospital has an “AA-” rating and stable outlook with Fitch. The rating is supported by the Miami-based system’s position as the “premier pediatric hospital in South Florida with a leading and growing market share,” Fitch said.
North Mississippi Health Services has an “AA” rating and stable outlook with Fitch. The rating reflects the Tupelo-based system’s strong cash position and strong market position with a leading market share in its primary services area, Fitch said.
Novant Health has an “AA-” rating and stable outlook with Fitch. The ratings agency said the Winston-Salem, N.C.-based system’s recent acquisition of three South Carolina hospitals from Dallas-based Tenet Healthcare will be accretive to its operating performance as the hospitals are highly profited and located in areas with growing populations and good income levels.
Oregon Health & Science University has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the Portland-based system’s top-class academic, research, and clinical capabilities, Moody’s said.
Orlando (Fla.) Health has an “AA-” rating and stable outlook with Fitch. The rating reflects the health system’s strong and consistent operating performance and a growing presence in a demographically favorable market, Fitch said.
Parkland Health has an “AA-” rating and stable outlook with Fitch. The rating reflects Fitch’s expectation that the Dallas-based system will remain the leading provider of public (safety net) services in the vast Dallas County service area, supported by its tax levy.
Presbyterian Healthcare Services has an “AA” rating and stable outlook with Fitch. The Albuquerque, N.M.-based system’s rating is driven by a strong financial profile combined with a leading market position with broad coverage in both acute care services and health plan operations, Fitch said.
Rush University System for Health has an “AA-” rating and stable outlook with Fitch. The rating reflects the Chicago-based system’s strong financial profile and an expectation that operating margins will rebound despite ongoing macro labor pressures, the rating agency said.
Saint Francis Healthcare System has an “AA” rating and stable outlook with Fitch. The rating reflects the Cape Girardeau, Mo.-based system’s strong financial profile, characterized by robust liquidity metrics, Fitch said.
Saint Luke’s Health System has an “Aa2” rating and stable outlook with Moody’s. The Kansas City, Mo.-based system’s rating was upgraded from “A1” after its merger with St. Louis-based BJC HealthCare was completed in January.
Salem (Ore.) Health has an “AA-” rating and stable outlook with Fitch. The rating reflects the system’s dominant marketing position in a stable service area with good population growth and demand for acute care services, Fitch said.
Seattle Children’s Hospital has an “AA” rating and a stable outlook with Fitch. The rating reflects the system’s strong market position as the only children’s hospital in Seattle and provider of pediatric care to an area that covers four states, Fitch said.
SSM Health has an “AA-” rating and stable outlook with Fitch. The St. Louis-based system’s rating is supported by a strong financial profile, multistate presence and scale with good revenue diversity, Fitch said.
St. Elizabeth Medical Center has an “AA” rating and stable outlook with Fitch. The rating reflects the Edgewood, Ky.-based system’s strong liquidity, leading market position, and strong financial management, Fitch said.
Stanford Health Care has an “Aa3” rating and positive outlook with Moody’s. The rating reflects the Palo Alto, Calif.-based system’s clinical prominence, patient demand, and its location in an affluent and well-insured market, Moody’s said.
UChicago Medicine has an “AA-” rating and stable outlook with Fitch. The rating reflects the system’s strong financial profile in the context of its broad and growing reach for high-acuity services, Fitch said.
University Health has an “AA+” rating and stable outlook with Fitch. The San Antonio-based system’s outlook is based on the Bexar County Hospital District’s significant tax margin, good cost management, and strong leverage position relative to its liquidity and outstanding debt.
University of Colorado Health has an “AA” rating and stable outlook with Fitch. The Aurora-based system’s rating reflects a strong financial profile benefiting from a track record of robust operating margins and the system’s growing share of a growth market anchored by its position as the only academic medical center in the state, Fitch said.
VCU Health has an “Aa3” rating and stable outlook with Moody’s. The rating reflects the Richmond, Va.-based system’s status as one of Virginia’s leading academic medical centers and essential role as its largest safety net provider, supporting excellent patient demand at high acuity levels, Moody’s said.
Willis-Knighton Medical Center has an “AA-” rating and positive outlook with Fitch. The outlook reflects the Shreveport, La.-based system’s improving operating performance relative to the past two fiscal years combined with Fitch’s expectation for continued improvement in 2024 and beyond.