https://www.healthcaredive.com/news/what-its-like-to-be-a-nurse-6-months-coronavirus/581709/

Those on the front lines of the fight against the novel coronavirus worry about keeping themselves, their families and their patients safe.
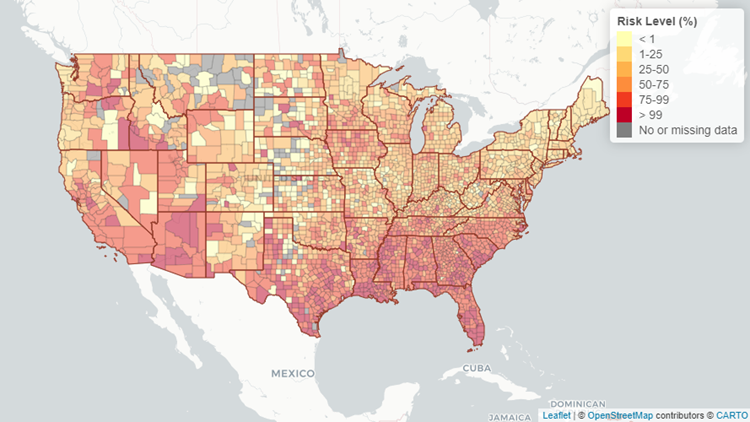
That’s especially true for nurses seeking the reprieve of their hospitals returning to normal operations sometime this year. Many in the South and West are now treating ICUs full of COVID-19 patients they hoped would never arrive in their states, largely spared from spring’s first wave.
And like many other essential workers, those in healthcare are falling ill and dying from COVID-19. The total number of nurses stricken by the virus is still unclear, though the Centers for Disease Control and Prevention has reported 106,180 cases and 552 deaths among healthcare workers. That’s almost certainly an undercount.
National Nurses United, the country’s largest nurses union, told Healthcare Dive it has counted 165 nurse deaths from COVID-19 and an additional 1,060 healthcare worker deaths.
Safety concerns have ignited union activity among healthcare workers during the pandemic, and also given them an opportunity to punctuate labor issues that aren’t new, like nurse-patient ratios, adequate pay and racial equality.
At the same time, the hospitals they work for are facing some of their worst years yet financially, after months of delayed elective procedures and depleted volumes that analysts predict will continue through the year. Many have instituted furloughs and layoffs or other workforce reduction measures.
Healthcare Dive had in-depth conversations with three nurses to get a clearer picture of how they’re faring amid the once-in-a-century pandemic. Here’s what they said.
Elizabeth Lalasz, registered nurse, John H. Stroger Hospital in Chicago
Elizabeth Lalasz has worked at John H. Stroger Hospital in Chicago for the past 10 years. Her hospital is a safety net facility, catering to those who are “Black, Latinx, the homeless, inmates,” Lalasz told Healthcare Dive. “People who don’t actually receive the kind of healthcare they should in this country.”
Data from the CDC show racial and ethnic minority groups are at increased risk of getting COVID-19 or experiencing severe illness, regardless of age, due to long-standing systemic health and social inequities.
CDC data reveal that Black people are five times more likely to contract the virus than white people.
This spring Lalasz treated inmates from the Cook County Jail, an epicenter in the city and also the country. “That population gradually decreased, and then we just had COVID patients, many of them Latinx families,” she said.

Once Chicago’s curve began to flatten and the hospital could take non-COVID patients, those coming in for treatment were desperately sick. They’d been delaying care for non-COVID conditions, worried a trip to the hospital could risk infection.
A Kaiser Family Foundation poll conducted in May found that 48% of Americans said they or a family member had skipped or delayed medical care because of the pandemic. And 11% said the person’s condition worsened as a result of the delayed care.
When patients do come into Lalasz’s hospital, many have “chest pain, then they also have diabetes, asthma, hypertension and obesity, it just adds up,” she said.
“So now we’re also treating people who’ve been delaying care. But after the recent southern state surges, the hospital census started going down again,” she said.
Amy Arlund, registered nurse, Kaiser Permanente Medical Center in Fresno, California:
Amy Arlund works the night shift at Kaiser Fresno as an ICU nurse, which she’s done for the past two decades.
She’s also on the hospital’s infection control committee, where for years she’s fought to control the spread of clostridium difficile colitis, or C. diff., in her facility. The highly infectious disease can live on surfaces outside the body for months or sometimes years.
The measures Arlund developed to control C. diff served as her litmus test, as “the top, most stringent protocols we could adhere to,” when coronavirus patients arrived at her hospital, she told Healthcare Dive.
But when COVID-19 cases surged in northern states this spring, “it’s like all those really strict isolation protocols that prior to COVID showing up would be disciplinable offenses were gone,” Arlund said.
Widespread personal protective equipment shortages at the start of the pandemic led the CDC and the Occupational Safety and Health Administration to change their longstanding guidance on when to use N95 respirator masks, which have long been the industry standard when dealing with novel infectious diseases.
The CDC also issued guidance for N95 respirator reuse, an entirely new concept to nurses like Arlund who say those changes go against everything they learned in school.
“I think the biggest change is we always relied on science, and we have always relied heavily on infection control protocols to guide our practice,” Arlund said. “Now infection control is out of control, we can no longer rely on the information and resources we always have.”

The CDC says experts are still learning how the coronavirus spreads, though person-to-person transmission is most common, while the World Health Organization recently acknowledged that it wouldn’t rule out airborne transmission of the virus.
In Arlund’s ICU, she’s taken care of dozens of COVID positive patients and patients ruled out for coronavirus, she said. After a first wave in the beginning of April, cases dropped, but are now rising again.
Other changing guidance weighing heavily on nurses is how to effectively treat coronavirus patients.
“Are we doing remdesivir this week or are we going back to the hydroxychloroquine, or giving them convalescent plasma?”Arlund said. “Next week I’m going to be giving them some kind of lavender enema, who knows.”
Erik Andrews, registered nurse, Riverside Community Hospital in Riverside, California:
Erik Andrews, a rapid response nurse at Riverside Community Hospital in California, has treated coronavirus patients since the pandemic started earlier this year. He likens ventilating them to diffusing a bomb.
“These types of procedures generate a lot of aerosols, you have to do everything in perfectly stepwise fashion, otherwise you’re going to endanger yourself and endanger your colleagues,” Andrews, who’s been at Riverside for the past 13 years, told Healthcare Dive.
He and about 600 other nurses at the hospital went on strike for 10 days this summer after a staffing agreement between the hospital and its owner, HCA Healthcare, and SEIU Local 121RN, the union representing RCH nurses, ended without a renewal.
The nurses said it would lead to too few nurses treating too many patients during a pandemic. Insufficient PPE and recycling of single-use PPE were also putting nurses and patients at risk, the union said, and another reason for the strike.
But rapidly changing guidance around PPE use and generally inconsistent information from public officials are now making the nurses at his hospital feel apathetic.
“Unfortunately I feel like in the past few weeks it’s gotten to the point where you have to remind people about putting on their respirator instead of face mask, so people haven’t gotten lax, but definitely kind of become desensitized compared to when we first started,” Andrews said.

With two children at home, Andrews slept in a trailer in his driveway for 12 weeks when he first started treating coronavirus patients. The trailer is still there, just in case, but after testing negative twice he felt he couldn’t spend any more time away from his family.
He still worries though, especially about his coworkers’ families. Some coworkers he’s known for over a decade, including one staff member who died from COVID-19 related complications.
“It’s people you know and you know that their families worry about them every day,” he said. “So to know that they’ve had to deal with that loss is pretty horrifying, and to know that could happen to my family too.”