https://medcitynews.com/2023/01/10

We expect 2023 to be a pivotal year for the industry, as the accelerated acceptance of virtual care and demographic trends, such as an aging population, increasing chronic illnesses and healthcare worker shortages, sustain demand for medtech-enabled solutions.
The combination of rapid developments in novel healthcare technology and heightened demand for integrated tech-enabled care has continued to fuel innovation in the medtech industry. At the same time, medtech innovators – whether in digital health, wearables and AI-driven offerings in healthcare, or diagnostics, telemedicine and health IT solutions – continue to face a patchwork of laws, rules and norms across the world. Life sciences and healthcare innovators and regulators are also looking to medtech to increase access to care and health equity. Here are ten global medtech themes we are tracking in the coming year:
Focus on digital tuck-in acquisitions in medtech M&A
Despite continued uncertainty in the overall financial market, medtech M&A activity continued at a steady pace in 2022. This year witnessed a rise in tuck-in acquisitions of smaller companies that can be easily integrated into buyers’ existing infrastructure and product offerings, as opposed to significantly sized takeovers of businesses that aren’t squarely aligned with buyers’ existing businesses lines. Medtech acquirers have been particularly focused on developing their digital capabilities to innovate and reach customers in new ways. As digitization continues to transform the industry, we expect acquirers to continue to prioritize the value of digital and data assets as they evaluate potential targets.
Continued interest by private equity and other financial sponsors
Private equity firms, healthcare-focused funds and other financial sponsors have continued to display a strong appetite for investing in Medtech companies, with top targets in subsectors such as diagnostics and healthcare IT solutions. Later-stage medtech companies in particular are gaining a larger share of venture capital funding, as later-stage investments allow financial sponsors to focus on businesses with higher yields, as well as less time to market and capital reimbursement. Demographic trends, including an aging population and the increasing prevalence of chronic diseases, coupled with healthcare technology advancements have created robust demand for medtech-enabled solutions. Additionally, medtech offerings have broad applications that can extend beyond stakeholders in a specific therapy area, product category or care setting, offering the ability to satisfy unmet needs with large patient bases.
Strategic medtech collaborations as the new norm
Strategic medtech collaborations and partnerships have become the new norm in our increasingly connected digital healthcare ecosystem. In response to heightened consumer demand for tech-enabled care, pharmaceutical and medtech companies are collaborating to use digital technologies to engage with consumers, unlocking a vast range of treatments such as personalized medicine. Additionally, as the market rapidly evolves towards data-driven healthcare, we expect medtech companies to continue to work collaboratively to address existing barriers to data sharing and promote interoperability of healthcare data.
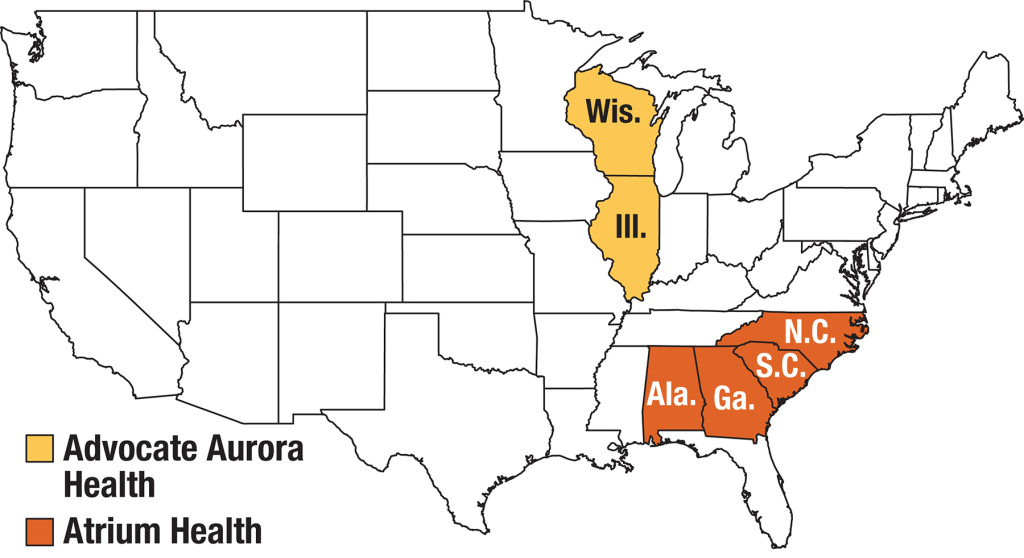
Continued scrutiny by antitrust and competition authorities
As expected, global antitrust and competition authorities continued to focus on the tech, life sciences and medtech sectors in 2022. The US, UK and EU authorities have stepped up efforts to investigate and challenge conduct by large pharma and technology companies pursuing mergers and acquisitions. We expect these authorities to assess similar concerns in the digital health context in an effort to account for the value of combined datasets and the interoperability of various offerings that could be derived from digital health mergers and acquisitions. Furthermore, geopolitical tensions have resulted in new and expanded foreign investment regimes to improve the resilience of domestic healthcare systems. Notably this year, the UK government implemented the National Security and Investment Act that allows it to restrict transactions that may threaten national security, including in the AI and data infrastructure sectors. Sensitive data continues to be a recurring theme for foreign investment review for Committee on Foreign Investment in the US and that of the EU as well.
Growing importance of data privacy and security
Increasing regulatory attention to sensitive health data and the escalating rise of ransomware attacks has made data privacy and security more important than ever for medtech innovators. The Federal Trade Commission has issued several statements about its willingness to “fully” enforce the law against the illegal use and sharing of highly sensitive data. Additionally, several state privacy laws coming into effect in 2023 create new categories of sensitive personal data, including health data, and impose novel obligations on innovators to obtain data-related consents. As ransomware continues to pose security-related threats, the US Department of Health and Human Services renewed calls for all covered entities and business associates to prioritize cybersecurity. New standards, such as cybersecurity label rating programs for connected devices, aim to address security risks. In the EU, medtech providers will need to consider how the launch of the European Health Data Space and newly proposed data regulation, such as the Data Act and AI Act, could impact their data use and sharing practices.
More active engagement with FDA/EMA/MHRA
We expect companies active in the medtech sector, particularly those that make use of AI and other advanced technologies, to continue their conversations with the U.S. Food and Drug Administration (“FDA”), the European Medicines Agency (“EMA”), the Medicines and Healthcare Products Regulatory Agency (“MHRA”) and other regulators as such companies grow their medtech business lines and establish their associated regulatory compliance infrastructure. Given the unique regulatory issues arising from the implementation of digital health technologies, we expect the FDA, EMA and MHRA to provide additional guidance on AI/ML-based software-as-a-medical device and the remote management of clinical trials. 2022 saw stakeholders in the life sciences and medtech industries collaborate with regulatory authorities to push forward the acceptance of digital endpoints that rely on sensor-generated data collected outside of a clinical setting. As the industry shifts to decentralized clinical trials, we expect both innovators and regulators to work together to evaluate the associated clinical, privacy and safety risks in the development and use of such digital endpoints.
Increasing medtech localization in the Asia Pacific region
2022 saw multinational companies (“MNCs”), including American pharma/device makers make an active effort to expand their medtech business lines in the Asia Pacific region. At the same time, government authorities in the region have been increasingly focused on incentivizing local innovation, approving government grants and prohibiting the importation of non-approved medical equipment. In light of MNCs’ market share of the medical device market in the Asia Pacific region, especially in China, we expect the emergence of the domestic medtech industry to prompt discussions among MNCs, local innovators and government authorities over the long-term development of the global market for medical technology.
Long-term adoption of telehealth and remote patient monitoring technologies
The Covid-19 pandemic saw the rise of telehealth and remote patient monitoring technologies as key modes of healthcare delivery. The telehealth industry remains focused on enabling remote consultations and long-term patient management for patients with chronic conditions. Looking forward, we expect to see increased innovation in non-invasive technologies that can provide early diagnostics and ongoing disease management in a low-friction manner. At the same time, we anticipate telehealth companies to face increasing scrutiny from regulatory authorities around the world for fraud and abuse by patients and providers. Consumer and patient data privacy and security in connection with telehealth and remote patient monitoring continue to remain top of mind for regulators as well.
Women’s health and privacy concerns for medtech
We expect to see increased consumer health tech adoption for reproductive care, especially in light of the U.S. Supreme Court’s decision to overturn Roe v. Wade. Following the Dobbs decision, a number of states introduced or passed legislation that prohibits or restricts access to reproductive health services beyond abortion. In response, women’s health-focused companies are expanding their virtual fertility and pregnancy, telemedicine and other services to patients. At the same time, such companies need to assess the legal risks stemming from the collection and storage of their customers’ personal health information, which could then be used as evidence to prosecute customers for obtaining illegal reproductive health services. We expect companies active in this space to take steps to navigate the patchwork of data privacy and security laws across jurisdictions while establishing clear digital health governance mechanisms to safeguard their customers’ data privacy and security.
Addressing inequities in the implementation of digital healthcare technologies
Medtech innovators and regulators have been increasingly focused on addressing inequities in the healthcare system and the data used to train AI and ML-based digital healthcare technologies. In 2022, a number of medtech companies collaborated to provide technologies that result in improved patient outcomes across all populations, as well as boost participation of diverse populations in clinical trials. In parallel, we are seeing increased interest from regulators to reduce bias in digital health technologies and the accompanying datasets, as evidenced by the EU’s proposed AI Act and the UK’s health data strategy. In the US, which currently lacks comprehensive government regulation of AI in healthcare, there have been increasing calls for institutional commitments in the area of algorithmovigilance. Because of the inaccurate conclusions that may result from biased technologies and data, MedTech companies must prioritize health equity in the implementation of digital healthcare technologies so that everyone can benefit from the latest scientific advances.
In conclusion, the medtech industry has remained resilient amidst the challenging macroeconomic environment. We expect 2023 to be a pivotal year for the industry, as the accelerated acceptance of virtual care and demographic trends, such as an aging population, increasing chronic illnesses and healthcare worker shortages, sustain demand for medtech-enabled solutions. At the same time, the rapidly changing legal and regulatory landscape will continue to be a key issue for medtech innovators moving forward. Adopting a global, forward-thinking regulatory compliance strategy can help MedTech companies stay competitive and ultimately, achieve better outcomes for patients.