Dive Brief:
- Hospitals’ labor costs rose by more than a third from pre-pandemic levels by March 2022, according to a report out Wednesday from Kaufman Hall.
- Heightened temporary and traveling labor costs were a main contributor, with contract labor accounting for 11% of hospitals’ total labor expenses in 2022 compared to 2% in 2019, the report found.
- Contract nurses’ median hourly wages rose 106% over the period, from $64 an hour to $132 an hour, while employed nurse wages increased 11%, from $35 an hour to $39 an hour, the report found.
Dive Insight:
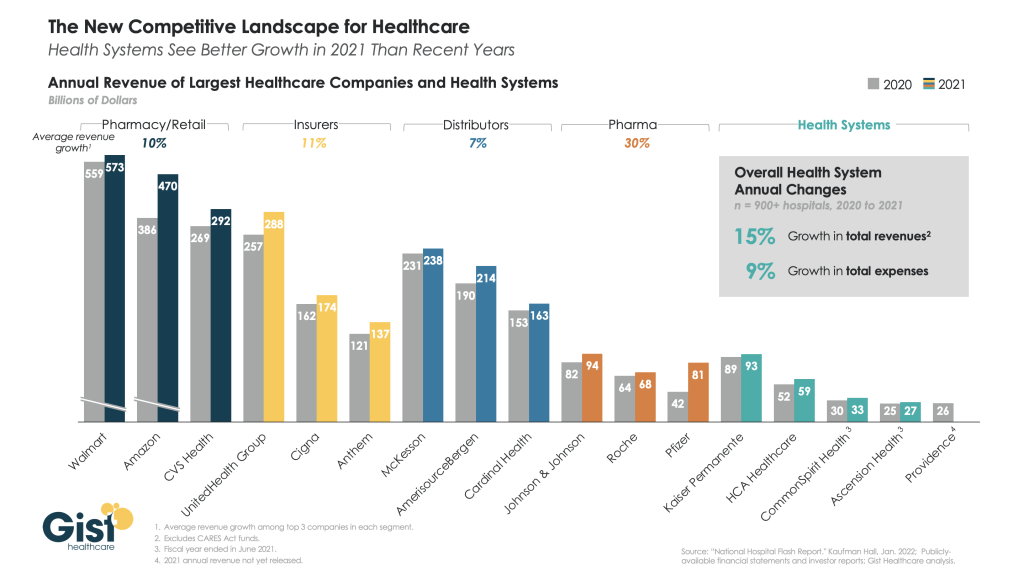
The new data from Kaufman Hall supports concerns hospital executives expressed while releasing first quarter earnings results, as higher-than expected labor costs spurred some operators, like HCA, to lower their financial full-year guidance.
The ongoing use of contract labor amid shortages driven by heightened turnover was a key factor executives cited for higher costs, and follows the findings from Kaufman Hall’s latest report.
More than a third of nurses surveyed by staffing firm Incredible Health said they plan to leave their current jobs by the end of this year, according to a March report. While burnout is driving them to leave, higher salaries are the top motivating factor for taking other positions, that report found.
Kaufman Hall’s report, which analyzes data from more than 900 hospitals across the country, found hospitals spent $5,494 in labor expenses per adjusted discharge in March compared to $4,009 roughly three years ago.
Costs rose for hospitals in every region, though the South and West experienced the largest increases from pre-pandemic levels as those expenses rose 43% and 42%, respectively.
The West and Northeast/Mid-Atlantic regions saw the highest expenses consistently from 2019 to 2022, according to the report.
“The pandemic made longstanding labor challenges in the healthcare sector much worse, making it far more expensive to care for hospitalized patients over the past two years,” said Erik Swanson, senior vice president of data and analytics at Kaufman Hall.
“Hospitals now face a number of pressures to attract and retain affordable clinical staff, maintain patient safety, deliver quality services and increase their efficiency,” Swanson said.
The report also notes that hospitals are competing with non-hospital employers also pursuing hourly staff, though those companies can pass along wage increases to consumers through higher prices “in a way healthcare organizations cannot,” the report said.
Some hospitals, like HCA Healthcare and Universal Health Services, are looking to raise prices for health plans amid rising nurse salaries, according to reporting from The Wall Street Journal.
Another recent report from group purchasing organization Premier found the CMS underestimated hospital labor spending when making payment adjustments for the 2022 fiscal year, resulting in hospitals receiving only a 2.4% rate increase compared to a 6.5% increase in hospital labor rates.
To match the rates hospitals are now paying staff, an adequate inpatient payment update for fiscal 2023 is needed, that report said.
The CMS proposed its IPPS rule for FY 2023 on April 18 that includes a 3.2% hike to inpatient hospital payments, which provider groups like the American Hospital Association rebuked as “simply unacceptable” considering inflation and rising hospital labor costs.