In the last 2 weeks, the Affordable Care Act (ACA) has been inserted itself in Campaign 2024 by Republican aspirants for the White House:
- On Truth Social November 28, former President Trump promised to replace it with something better: “Getting much better Healthcare than Obamacare for the American people will be a priority of the Trump Administration. It is not a matter of cost; it is a matter of HEALTH. America will have one of the best Healthcare Plans anywhere in the world. Right now, it has one of the WORST! I don’t want to terminate Obamacare, I want to REPLACE IT with MUCH BETTER HEALTHCARE. Obamacare Sucks!!!!”
- Then, on NBC’s Meet the Press December 3, Florida Governor Ron DeSantis offered “We need to have a healthcare plan that works,” Obamacare hasn’t worked. We are going to replace and supersede with a better plan….a totally different healthcare plan… big institutions that are causing prices to be high: big pharma, big insurance and big government.”
It’s no surprise. Health costs and affordability rank behind the economy as top issues for Republican voters per the latest Kaiser Tracking Poll. And distaste with the status quo is widespread and bipartisan: per the Keckley Poll (October 2023), 70% of Americans including majorities in both parties and age-cohorts under 65 think “the system is fundamentally flawed and needs major change.” To GOP voters, the ACA is to blame.
Background:
The Affordable Care Act (aka Obamacare aka the Patient Protection and Affordable Care Act) was passed into law March 23, 2013. It is the most sweeping and controversial health industry legislation passed by Congress since Lyndon Johnson’s Medicare and Medicaid Act (1965). Opinions about the law haven’t changed much in almost 14 years: when passed in 2010, 46% were favorable toward the law vs. 40% who were opposed. Today, those favorable has increased to 59% while opposition has stayed at 40% (Kaiser Tracking Poll).
Few elected officials and even fewer voters have actually read the law. It’s understandable: 955 pages, 10 major sections (Titles) and a plethora of administrative actions, executive orders, amendments and legal challenges that have followed. It continues to be under-reported in media and misrepresented in campaign rhetoric by both sides. Campaign 2024 seems likely to be more of the same.
In 2009, I facilitated discussions about health reform between the White House Office of Health Reform and the leading private sector players in the system (the American Medical Association, the American Hospital Association, America’s Health Insurance Plans, AdvaMed, PhRMA, and BIO). The impetus for these deliberations was the Obama administration’s directive that systemic reform was necessary with three-aims: reduce cost, increase access via insurance coverage and improve the quality of care provided by a private system. In parallel, key Committees in the House and Senate held hearings ultimately resulting in passage of separate House and Senate versions with the Senate’s becoming the substance of the final legislation. Think tanks on the left (I.e. the Center for American Progress et al.) and on the right (i.e. the Heritage Foundation) weighed in with members of Congress and DC influencers as the legislation morphed. And new ‘coalitions, centers and institutes’ formed to advocate for and against certain ACA provisions on behalf of their members while maintaining a degree of anonymity.
So, as the ACA resurfaces in political discourse in coming months, it’s important it be framed objectively. To that end, 3 major considerations are necessary to have a ‘fair and balanced’ view of the ACA:
1-The ACA was intended as a comprehensive health reform legislative platform. It was designed to be implemented between 2010 and 2019 in a private system prompted by new federal and state policies to address cost, access and quality. It allowed states latitude in implementing certain elements (like Medicaid expansion, healthcare marketplaces) but few exceptions in other areas (i.e.individual and employer mandates to purchase insurance, minimum requirements for qualified health plans, et al). The CBO estimated it would add $1.1 trillion to overall healthcare spending over the decade but pay for itself by reducing demand, administrative red-tape and leveraging better data for decision-making. The law included provisions to…
- To improve quality by modernizing of the workforce, creating an Annual Quality Report obligation by HHS, creating the Patient Centered Outcome Research Institute and expanding the the National Quality Forum, adding requirements that approved preventive care be accessible at no cost, expanding community health centers, increasing residency programs in primary care and general surgery, implementing comparative effectiveness assessments to enable clinical transparency and more.
- To increase access to health insurance by subsidizing coverage for small businesses and low income individuals (up to 400% of the Federal poverty level), funding 90% of the added costs in states choosing to expand their Medicaid enrollments for households earning up to 138% of the poverty level, extending household coverage so ‘young invincibles’ under 26 years of age could stay on their parent’s insurance plan, requiring insurers to provide “essential benefits” in their offerings, imposing medical loss ratio (MLR) mandates (80% individual, 85% group) and more.
- To lower costs by creating the CMS Center for Medicare and Medicaid Innovation to construct 5-year demonstration pilots and value-based purchasing programs that shift provider incentives from volume to value, imposing price and quality reporting and transparency requirements and more.
The ACA was ambitious: it was modeled after Romneycare in MA and premised on the presumption that meaningful results could be achieved in a decade. But Romneycare (2006) was about near-universal insurance coverage for all in the Commonwealth, not the triple aim, and the resistance calcified quickly among special interests threatened by its potential.
2-The ACA passed at a time of economic insecurity and hyper-partisan rancor and before many of the industry’s most significant innovations had taken hold. The ACA was the second major legislation passed in the first term of the Obama administration (2009-2012); the first was the $831 billion American Recovery and Reconstruction Act (ARRA) stimulus package that targeted “shovel ready jobs” as a means of economic recovery from the 2008-2010 Great Recession. But notably, it included $138 billion for healthcare including requirements for hospitals and physicians to computerize their medical records, extension of medical insurance to laid off workers and additional funding for states to offset their Medicaid program expenses. The Obama-Biden team came to power with populist momentum behind their promises to lower health costs while keeping the doctors and insurance plans they had. Its rollout was plagued by miscues and the administration’s most popular assurances (‘keep your doctor and hospitals’) were not kept. The Republican Majority in the 111th Congress’ (247-193)) seized on the administration’s miss fueling anti-ACA rhetoric among critics and misinformation.
3-Support for the ACA has grown but its results are mixed. It has survived 7 Supreme Court challenges and more than 70 failed repeal votes in Congress. It enjoys vigorous support in the Biden administration and among the industry’s major trade groups but remains problematic to outsiders who believe it harmful to their interests. For example, under the framework of the ACA, the administration is pushing for larger provider networks in the 18 states and DC that run their own marketplaces, expanded dental and mental health coverage, extended open enrollment for Marketplace coverage and restoration of restrictions on “junk insurance’ but its results to date are mixed: access to insurance coverage has increased. Improvements in quality have been significant as a result of innovations in care coordination and technology-enabled diagnostic accuracy. But costs have soared: between 2010 and 2021, total health spending increased 64% while the U.S. population increased only 7%.
So, as the ACA takes center stage in Campaign 2024, here are 4 things to watch:
1-Media attention to elements of the ACA other than health insurance coverage. My bet: attention from critics will be its unanticipated costs in addition to its federal abortion protections now in the hands of states. The ACA’s embrace of price and quality transparency is of particular interest to media and speculation that industry consolidation was an unintended negative result of the law will energize calls for its replacement. Thus, the law will get more attention. Misinformation and disinformation by special interests about its original intent as a “government takeover of the health system” will be low hanging fruit for antagonists.
2- Changes to the law necessary intended to correct/mitigate its unintended consequences, modernize it to industry best practice standards and responses to court challenges will lend to the law’s complex compliance challenges for each player in the system. New ways of prompting Medicaid expansion, integration of mental health and social determinants with traditional care, the impact of tools like ChatGPT, quantum computing, generative AI not imagined as the law was built, the consequences of private equity investments on prices and spending, and much more.
3-Public confusion. The ACA is a massive law in a massive industry. Cliff’s Notes are accessible but opinions about it are rarely based on a studied view of its intent and structure. It lends itself to soundbites intended to obscure, generalize or misdirect the public’s attention.
4-The ACA price tag. In 2010, the CBO estimated its added cost to health spending at $1.1 trillion (2010-2019) but its latest estimate is at least $3 trillion for its added insurance subsidies alone. The fact is no one knows for sure what its costs are nor the value of the changes it has induced into the health system. The ranks of those with insurance coverage has been cut in half. Hospitals, physicians, post-acute providers, drug manufacturers and insurers are implementing value-based care strategies and price transparency (though reluctantly) but annual health cost increases have consistently exceeded 4% annually as the cumulative impact of medical inflation, utilization, consolidation and price increases are felt.
Final thought:
I have studied the ACA, and the enabling laws, executive orders, administrative and regulatory actions, court rulings and state referenda that have followed its passage. Despite promises to ‘repeal and replace’ by some, it is more likely foundational to bipartisan “fix and repair’ regulatory reforms that focus more attention to systemness, technology-enabled self-care, health and wellbeing and more.
It will be interesting to see how the ACA plays in Campaign 2024 and how moderators for the CNN-hosted debates January 10 in Des Moines and January 21 in New Hampshire address it. In the 2-hour Tuscaloosa debate last Wednesday, it was referenced in response to a question directed to Gov. DeSantis about ‘reforming the system’ 101 minutes into the News Nation broadcast. It’s certain to get more attention going forward and it’s certain to play a more prominent role in the future of the system.
The ACA is back on the radar in U.S. healthcare. Stay tuned.
PS The resignations under pressure of Penn President Elizabeth Magill and Board Chair Scott Bok over inappropriate characterization of Hamas’ genocidal actions toward Jews are not surprising. Her response to Congressional questioning was unfortunate. The eventuality turned in 4 days, sparked by student outrage and adverse media attention that tarnished the reputations of otherwise venerable institutions like Penn, MIT and Harvard.
The lessons for every organization, including the big names in healthcare, are not to be dismissed: Beyond the issues of genocide, our industry is home to a widening number of incendiary issues like Hamas.
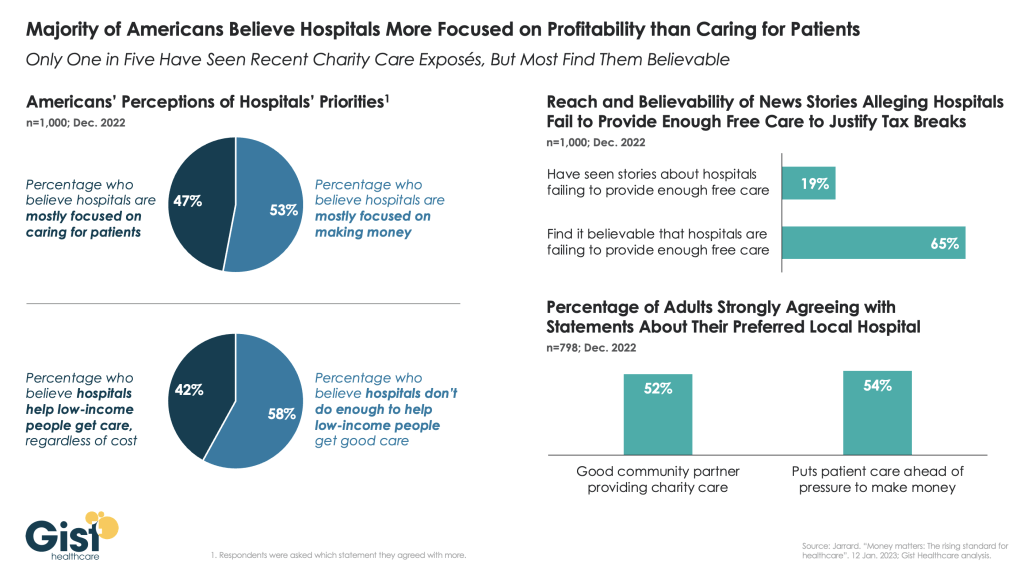
They’re increasingly exposed to public smell tests that often lead to more: Workforce strikes. CEO compensation. Fraud and abuse. Tax exemptions and community benefits. Prior authorization and coverage denial. Corporate profit. Patient collection and benevolent use policies. Board independence and competence and many more are ripe for detractors and activist seeking attention.
Public opinion matters. Reputations matter. Boards of Directors are directly accountable for both.