Peoria, Ill.-based OSF HealthCare has seen drastic improvements to its financial performance over the last two years, a performance that has allowed the health system to see revenue growth and expand its M&A footprint.
OSF was able to turn around a $43.2 million operating loss (-4.5% margin) in the first quarter ended Dec. 31, 2022, to a $0.9 million gain over the same period in 2023.
But the health system didn’t stop there and, in the first six months ended March 31, 2023, transformed a $60.9 million operating loss to an $8.9 million gain for the same period in 2024.
OSF HealthCare CFO Michael Allen connected with Becker’s to discuss the strategies that helped OSF get to a more steady financial place and some of their plans for the future.
Question: What strategies has OSF HealthCare implemented to help it turn the corner financially?
Michael Allen: OSF Healthcare has improved operating results by more than $70 million compared to FY2023, after seeing an even larger improvement from FY2022 to FY2023. After a very difficult FY2022, from a financial perspective, the organization launched a series of initiatives to return to positive margins.
There has been a focus on reducing the reliance on contract labor, nursing and other key clinical positions, with better recruiting and retaining initiatives. The organization is actively implementing automation for repeatable tasks in hard-to-recruit administrative functions and is actively managing supply and pharmaceutical costs against inflationary pressures.
OSF has also seen revenue growth from patient demand, expanding markets, capacity management and improved payment levels from government and commercial payers.
Q: KSB Hospital and OSF HealthCare recently entered into merger negotiations. How do you expect hospital consolidation to evolve in your market as many small, independent providers continue to face financial challenges and struggle to improve their bottom lines?
MA: The economics of the healthcare delivery system model is challenging in most markets, but particularly difficult for small and independent hospitals and clinics. Given the structure of the payment system and the rising operating costs, I don’t see this pressure easing any time soon.
OSF is looking forward to our opportunity to extend our healthcare ministry to KSB and the greater Dixon area and continue their great legacy of patient care.
Q: What advice would you have for other health system financial leaders looking to get their margins up this year?
MA: There are no silver bullets to improving margins. It’s the daily work of using our costs wisely and executing on important strategies that will win the day. Automation, elimination of non-value-added costs and continuously looking for opportunities to get the best care, patient engagement and workforce engagement is where OSF and other health systems will continue to focus.
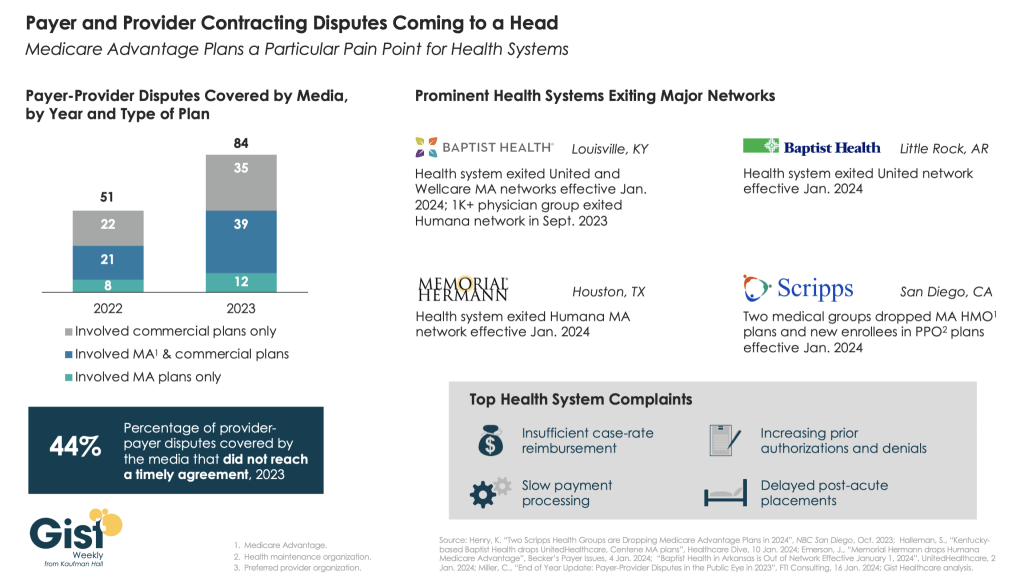
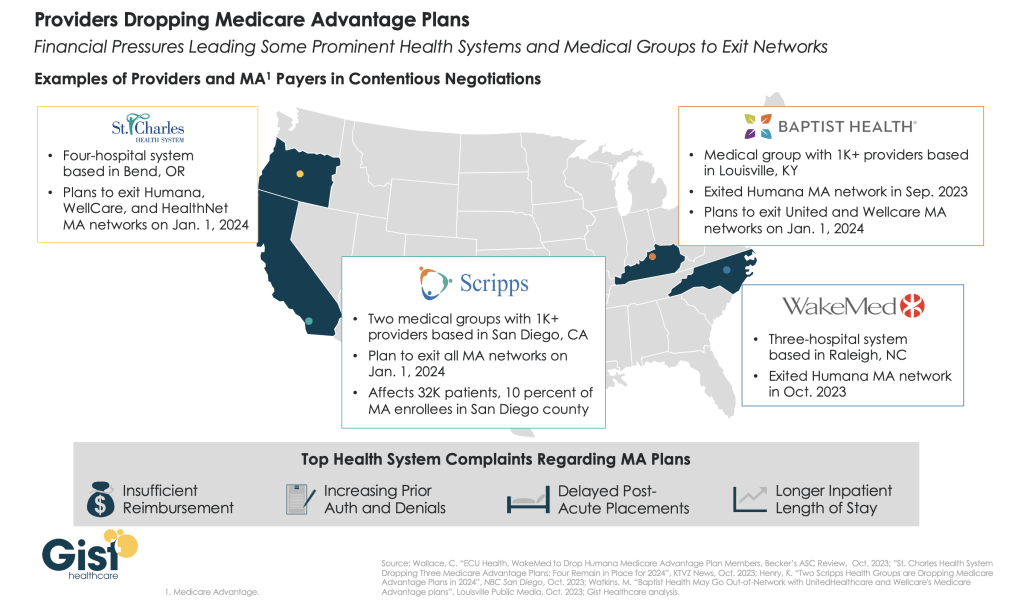
Q: An increasing number of hospitals and health systems across the U.S. are dropping some or all of their commercial Medicare Advantage contracts. Where do you see the biggest challenges and opportunities for health systems navigating MA?
MA: As more and more patients and payers are entering Medicare Advantage, we continue to watch our metrics on payment levels to ensure we are being paid fairly and within contract terms for our payer partners.
There does appear to be a trend of increasing denials that often aren’t justified or are not within our contract terms, and we will continuously work to rectify those issues with our payers to ensure our patients receive the appropriate care and OSF is paid fairly for services provided.