https://www.beckershospitalreview.com/finance/state-by-state-breakdown-of-130-rural-hospital-closures.html

Nearly one in five Americans live in rural areas and depend on their local hospital for care. Over the past 10 years, 130 of those hospitals have closed.
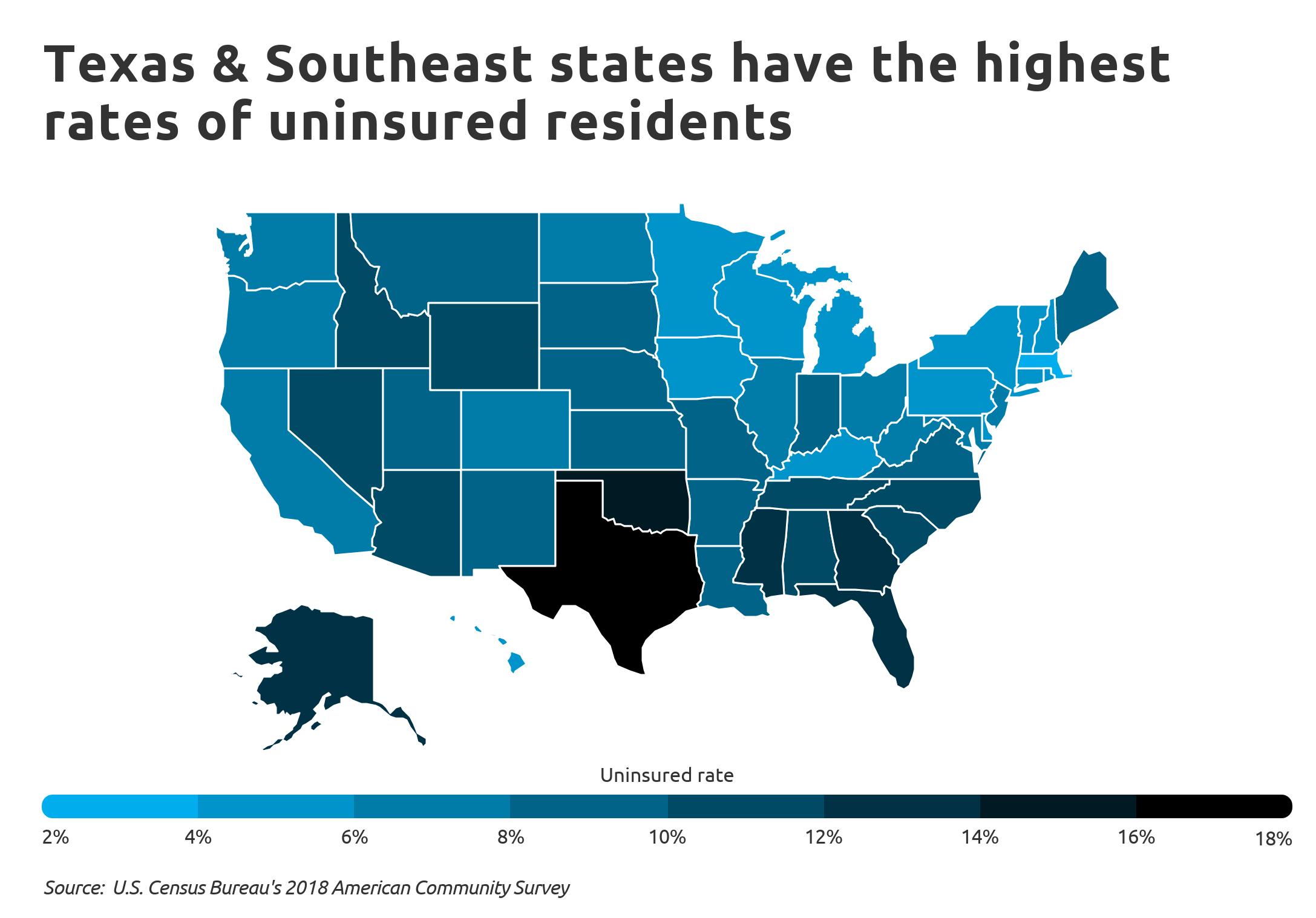
Thirty-three states have seen at least one rural hospital shut down since 2010, and the closures are heavily clustered in states that have not expanded Medicaid under the ACA, according to the Cecil G. Sheps Center for Health Services Research.
Twenty-one rural hospitals in Texas have closed since 2010, the most of any state. Tennessee has the second-most closures, with 13 rural hospitals shutting down in the past decade. In third place is Oklahoma with eight closures.
Listed below are the 130 rural hospitals that have closed since Jan. 1, 2010, as tracked by the Sheps Center. For the purposes of its analysis, the Sheps Center defined a hospital closure as the cessation in the provision of inpatient services.
“We follow the convention of the Office of Inspector General that a closed hospital is ‘a facility that stopped providing general, short-term, acute inpatient care,'” reads a statement on the Sheps Center’s website. “We did not consider a hospital closed if it: merged with, or was sold to, another hospital but the physical plant continued to provide inpatient acute care, converted to critical access status, or both closed and reopened during the same calendar year and at the same physical location.”
As of June 8, all the facilities listed below had stopped providing inpatient care. However, some of them still offered other services, including outpatient care, emergency care, urgent care or primary care.
Alabama
SouthWest Alabama Medical Center (Thomasville)
Randolph Medical Center (Roanoke)
Chilton Medical Center (Clanton)
Florence Memorial Hospital
Elba General Hospital
Georgiana Medical Center
Alaska
Sitka Community Hospital
Arizona
Cochise Regional Hospital (Douglas)
Hualapai Mountain Medical Center (Kingman)
Florence Community Healthcare
Arkansas
De Queen Medical Center
California
Kingsburg Medical Center
Corcoran District Hospital
Adventist Health Feather River (Paradise)
Coalinga Regional Medical Center
Florida
Campbellton-Graceville Hospital
Regional General Hospital (Williston)
Shands Live Oak Regional Medical Center
Shands Starke Regional Medical Center
Georgia
Hart County Hospital (Harwell)
Charlton Memorial Hospital (Folkston)
Calhoun Memorial Hospital (Arlington)
Stewart-Webster Hospital (Richland)
Lower Oconee Community Hospital (Glenwood)
North Georgia Medical Center (Ellijay)
Illinois
St. Mary’s Hospital (Streator)
Indiana
Fayette Regional Health System
Kansas
Central Kansas Medical Center (Great Bend)
Mercy Hospital Independence
Mercy Hospital Fort Scott
Horton Community Hospital
Oswego Community Hospital
Sumner Community Hospital (Wellington)
Kentucky
Nicholas County Hospital (Carlisle)
Parkway Regional Hospital (Fulton)
New Horizons Medical Center (Owenton)
Westlake Regional Hospital (Columbia)
Louisiana
Doctor’s Hospital at Deer Creek (Leesville)
Maine
St. Andrews Hospital (Boothbay Harbor)
Southern Maine Health Care-Sanford Medical Center
Parkview Adventist Medical Center (Brunswick)
Maryland
Edward W. McCready Memorial Hospital (Crisfield)
Massachusetts
North Adams Regional Hospital
Michigan
Cheboygan Memorial Hospital
Minnesota
Lakeside Medical Center
Albany Area Hospital
Albert Lea-Mayo Clinic Health System
Mayo Clinic Health System-Springfield
Mississippi
Patient’s Choice Medical of Humphreys County (Belzoni)
Pioneer Community Hospital of Newton
Merit Health Natchez-Community Campus
Kilmichael Hospital
Quitman County Hospital (Marks)
Missouri
Sac-Osage Hospital (Osceola)
Parkland Health Center-Weber Road (Farmington)
Southeast Health Center of Reynolds County (Ellington)
Southeast Health Center of Ripley County (Doniphan)
Twin Rivers Regional Medical Center (Kennett)
I-70 Community Hospital (Sweet Springs)
Pinnacle Regional Hospital (Boonville)
Nebraska
Tilden Community Hospital
Nevada
Nye Regional Medical Center (Tonopah)
New York
Lake Shore Health Care Center
Moses-Ludington Hospital (Ticonderoga)
North Carolina
Blowing Rock Hospital
Vidant Pungo Hospital (Belhaven)
Novant Health Franklin Medical Center (Louisburg)
Yadkin Valley Community Hospital (Yadkinville)
Our Community Hospital (Scotland Neck)
Sandhills Regional Medical Center (Hamlet)
Davie Medical Center-Mocksville
Ohio
Physicians Choice Hospital-Fremont
Doctors Hospital of Nelsonville
Oklahoma
Muskogee Community Hospital
Epic Medical Center (Eufaula)
Memorial Hospital & Physician Group (Frederick)
Latimer County General Hospital (Wilburton)
Pauls Valley General Hospital
Sayre Community Hospital
Haskell County Community Hospital (Stigler)
Mercy Hospital El Reno
Pennsylvania
Saint Catherine Medical Center Fountain Springs (Ashland)
Mid-Valley Hospital (Peckville)
Ellwood City Medical Center
UPMC Susquehanna Sunbury
South Carolina
Bamberg County Memorial Hospital
Marlboro Park Hospital (Bennettsville)
Southern Palmetto Hospital (Barnwell)
Fairfield Memorial Hospital (Winnsboro)
South Dakota
Holy Infant Hospital (Hoven)
Tennessee
Riverview Regional Medical Center South (Carthage)
Starr Regional Medical Center-Etowah
Haywood Park Community Hospital (Brownsville)
Gibson General Hospital (Trenton)
Humboldt General Hospital
United Regional Medical Center (Manchester)
Parkridge West Hospital (Jasper)
Tennova Healthcare-McNairy Regional (Selmer)
Copper Basin Medical Center (Copperhill)
McKenzie Regional Hospital
Jamestown Regional Medical Center
Takoma Regional Hospital (Greeneville)
Decatur County General Hospital (Parsons)
Texas
Wise Regional Health System-Bridgeport
Shelby Regional Medical Center
Renaissance Hospital Terrell
East Texas Medical Center-Mount Vernon
East Texas Medical Center-Clarksville
East Texas Medical Center-Gilmer
Good Shepherd Medical Center (Linden)
Lake Whitney Medical Center (Whitney)
Hunt Regional Community Hospital of Commerce
Gulf Coast Medical Center (Wharton)
Nix Community General Hospital (Dilley)
Weimar Medical Center
Care Regional Medical Center (Aransas Pass)
East Texas Medical Center-Trinity
Little River Healthcare Cameron Hospital
Little River Healthcare Rockdale Hospital
Stamford Memorial Hospital
Texas General-Van Zandt Regional Medical Center (Grand Saline)
Hamlin Memorial Hospital
Chillicothe Hospital
Central Hospital of Bowie
Virginia
Lee Regional Medical Center (Pennington Gap)
Pioneer Community Hospital of Patrick County (Stuart)
Mountain View Regional Hospital (Norton)
West Virginia
Williamson Memorial Hospital
Fairmont Regional Medical Center
Wisconsin
Franciscan Skemp Medical Center (Arcadia)





/cdn.vox-cdn.com/uploads/chorus_asset/file/13249599/GettyImages_984402230.jpg)






