https://healthcareuncovered.substack.com/p/expect-more-hunger-in-america-with
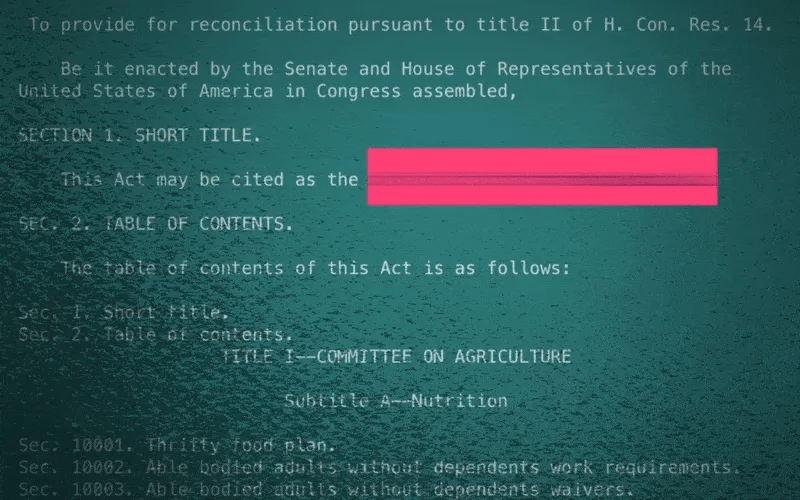
The recently passed One Big Beautiful Bill Act, which makes deep cuts to the Medicaid program, also puts the food assistance that 41 million low-income Americans rely on in jeopardy. Many of the families currently getting food provided by the Supplemental Nutrition Assistance Program (SNAP) stand to lose that support.
SNAP may well disappear for some families as the federal government moves to trim it. “The cuts are massive and extremely cruel when families need more support, not less,” says Signe Anderson, senior director of nutrition advocacy, at the Tennessee Justice Center in Nashville.
Government food assistance was established during the Great Depression, but it wasn’t until 1977 that the program became more accessible when the requirement that recipients had to pay for a portion of their food stamps was ended. Throughout its history, foes of the program have tried to dismantle it and may have succeeded as a result of provisions in the bill President Trump signed on July 4.
The new legislation calls for cutting spending for food stamps by $186 billion through 2034. “Everyone on food stamps will be affected in some way, and many will lose benefits,” Anderson says. “I don’t think the Congress understands the level of necessity in the community for food, health care and mental health treatment, some for the rest of their lives.”
One major change is being made to work requirements that have historically been part of the Medicaid program, which is administered and partially funded by the states. Anderson points out that under the new arrangements, participants may find the task of enrolling and staying enrolled more onerous. “We see a lot of people cut off already because too many life circumstances make it difficult for them to meet work requirements.”
Indeed when you look at the changes to SNAP, the first word that might come to mind is ‘draconian.’
To receive benefits those new to the program, and those already on it who are between 55 and 64 and do not have dependent children or who have children 14 and older, will have to prove they work. Or they will have to volunteer at least 20 hours a week or enroll in training programs. Parents of school-aged children will now be required to work.
Some five million people, including about 800,000 children and about a half million adults who are 65 and older, could lose their food benefits.
The programs the new law targets have been a lifeline for some. Nikole Ralls, a 43-year-old woman in Nashville, who was once a drug addict but now counsels others who need help, says, “I got my life turned around because of Medicaid and SNAP.”
In a recent memo to state agencies administering the SNAP program, Agriculture Secretary Brooke Rollins said she was concerned about what was described as abuse of the waiver system by states, noting that the new approach for the SNAP program would prioritize work, education and volunteering over what the department characterized as “idleness and excessive spending.”
Anderson said, “The public doesn’t understand what hunger looks like and are misinformed about how well-run and streamlined the SNAP program is.”
“Most of the people who can, do work. We have parents working two and three jobs,” Anderson said. For families in this predicament food banks, which have become default grocery stores, may be of little help. They, too, are stretched thin. The Wall Street Journal reported food banks across the country are already straining under rising demand, and some worry there won’t be enough food to meet demand.