To understand the fatal attack on UnitedHealthcare CEO Brian Thompson and the unexpected reaction on social media, you have to go back to the 1990s when managed care was in its infancy. As a consumer representative, I attended meetings of a group associated with the health care system–doctors, academics, hospital executives, business leaders who bought insurance, and a few consumer representatives like me.
It was the dawn of the age of managed care with its promise to lower the cost and improve the quality of care, at least for those who were insured.
New perils came with that new age of health coverage.
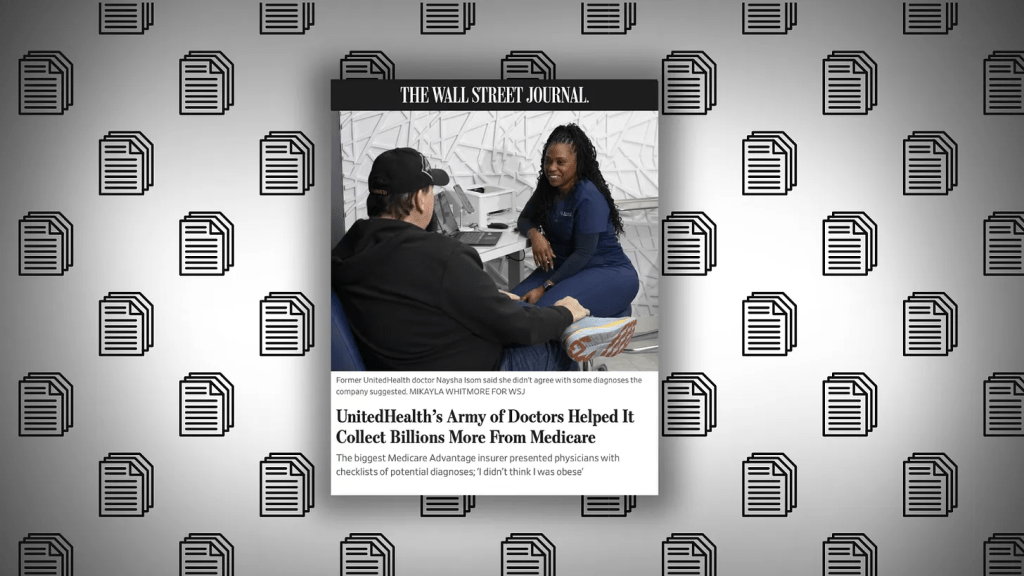
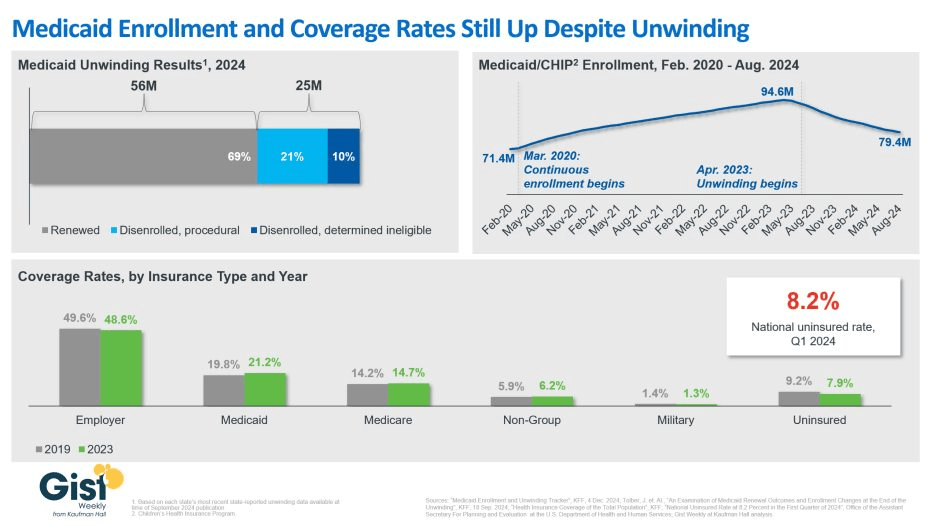
In the quest to save money while ostensibly improving quality, there was always a chance that the managed care entities and the doctors they employed or contracted with – by then called managed care providers – could clamp down too hard and refuse to pay for treatments, leaving some people to suffer medically. Groups associated with the health care industry tried to set standards to guard against that, but as the industry consolidated and competition among the big players in the new managed care system consolidated, such worries grew.
Over the years the squeeze on care got tighter and tighter as the giants like UnitedHealthcare–which grew initially by buying other insurance companies such as Travelers and Golden Rule–and Elevance, which gobbled up previously nonprofit Blue Cross plans in the 1990s, starting with Blue Cross of California, needed to please the gods of the bottom line. Shareholders became all important. Paying less for care meant more profits and return to investors, so it is no wonder that the alleged killer of the UnitedHealthcare chief executive reportedly left the chilling message:
‘‘DENY. DEFEND. DEPOSE,” words associated with insurance company strategies for denying claims.
The American health care system was far from perfect even in the days when more employers offered good coverage for their workers and often paid much or all of the cost to attract workers. Not-for-profit Blue Cross Blue Shield plans in many states provided most of the coverage, and by all accounts, they paid claims promptly. In my now very long career of covering insurance, I cannot recall anyone in the old days complaining that their local Blue Cross Blue Shield organization was withholding payment for care.
Today Americans, even those who thought they had “good” coverage, are now finding themselves underinsured, as a 2024 Commonwealth Fund study so clearly shows. Nearly one-quarter of adults in the U.S. are underinsured meaning that although they have health insurance, high deductibles, copayments and coinsurance make it difficult or impossible for them to pay for needed care. As many as one-third of people with chronic conditions such as diabetes said they don’t take their medications or even fill prescriptions because they cost too much.
Before he passed away last year, one of our colleagues, Marshall Allen, had made recommendations to his followers on how to deal with medical bills they could not pay. KFF reporters also investigated the problems families face with super-high bills. In 2022 KFF reporters offered readers a thorough look at medical debt in the U.S. and reported alarming findings.
In 2019, U.S. medical debt totaled $195 billion, a sum larger than the economy of Greece. Half of adults don’t have enough cash to cover an unexpected medical bill while 50 million adults – one in five in the entire country – are paying off bills on an installment plan for their or a family member’s care.
One would think that such grim statistics might prompt political action to help ease the debt burden on American families. But a look at the health proposals from the Republican Study Committee suggest that likely won’t happen. The committee’s proposed budget would cut $4.5 trillion dollars from the Affordable Care Act, Medicaid, and the Children’s Health Insurance Program leaving millions of Americans without health care.
From the Democrats, there appear to be no earth-shaking proposals in their immediate future, either. Late last summer STAT News reported, “With the notable exception of calling to erase medical debt by working with the states, Democrats are largely eyeing marginal extensions or reinstatements of their prior policy achievements.” Goals of the Democratic National Committee were shoring up the Affordable Care Act, reproductive rights, and addressing ambulance surprise bills.
A few years ago when I was traveling in Berlin, our guide paused by a statue of Otto von Bismarck, Germany’s chancellor in the late 1800s, who is credited with establishing the German health system. The guide explained to his American travelers how and why Bismarck founded the German system, pointing out that Germany got its national health system more than a hundred years before Obamacare. Whether the Americans got the point he was making, I could not tell for no one in the group appeared interested in Germany’s health care system. Today, though, they might pay more attention.
In the coming months, I will write about health systems in Germany and other developed countries that, as The Commonwealth Fund’s research over many years has shown, do a much better job than ours at delivering high quality care – for all of their citizens – and at much lower costs.